Table of Contents
What is Blood Agar?
- Blood agar is a specialized bacterial growth medium that is commonly used in microbiology laboratories. It is an enriched medium designed to support the growth of fastidious organisms, particularly those belonging to the streptococci group, which do not thrive well on ordinary growth media.
- The composition of blood agar typically includes a base containing trypticase soy agar, which provides a source of nutrients such as tryptones, soybean protein digest, and sodium chloride (NaCl). Additionally, it is enriched with 5% sheep blood, which is crucial for the growth of certain bacteria.
- One of the reasons why blood agar is commonly used is its ability to detect hemolysis, the breakdown of red blood cells. Hemolysis can be categorized into three types: alpha, beta, and gamma. In the case of beta hemolysis, the bacteria produce enzymes that cause complete lysis of red blood cells, resulting in a clear zone surrounding the colonies. This distinct pattern helps in the identification of the organism.
- However, blood contains inhibitors that can hinder the growth of specific bacteria, such as those belonging to the Neisseria and Haemophilus genera. To overcome this limitation, the blood agar must be heated, which inactivates these inhibitors and releases essential growth factors, including the V factor. Heating the blood agar causes it to turn into chocolate agar, named after its characteristic chocolate color, and provides a suitable environment for the growth of Neisseria and Haemophilus bacteria.
- Blood agar can be prepared by supplementing a basal medium, such as Columbia Agar or Tryptic Soy Agar, with 5% defibrinated mammalian blood, including human, sheep, or horse blood. The presence of blood in the medium provides additional nutrients and creates an enriched environment for the cultivation of fastidious bacteria.
- One of the significant advantages of blood agar is its ability to support the growth of pathogenic organisms that produce extracellular enzymes capable of causing hemolysis. This property makes blood agar a valuable tool for the isolation and identification of such organisms. By observing the hemolysis patterns produced by the growing bacteria, microbiologists can gain insights into the characteristics and virulence of the organisms under investigation.
- In summary, blood agar is an enriched bacterial growth medium used for the cultivation of fastidious organisms. Its composition includes a base medium, such as Columbia Agar or Tryptic Soy Agar, supplemented with 5% sheep blood. Blood agar supports the growth of bacteria that may not thrive on general media and allows for the observation of hemolysis patterns, aiding in the identification of pathogenic organisms.

Composition of Blood Agar
The composition of blood agar includes several key ingredients, such as beef heart peptone, tryptose, sodium chloride, agar, and sheep blood.
The primary purpose of beef heart peptone and tryptose in blood agar is to serve as protein sources, providing essential amino acids and nutrients to support bacterial growth. The specific type of protein sources may vary depending on the manufacturer and can include pancreatic digest of casein, papain digest of soy meal, neutralized peptone, yeast extract, or a combination of these components.
Sodium chloride, also known as table salt, is added to the medium to maintain the osmotic balance necessary for bacterial growth. It helps regulate the concentration of ions inside and outside the bacterial cells, promoting optimal growth conditions.
Agar, derived from seaweed, is a gelatinous substance that serves as a solidifying agent. It provides a solid surface for bacterial colonies to grow on and allows for the isolation and observation of individual bacterial colonies.
One crucial component of blood agar is the addition of sheep blood. Sheep blood is the preferred choice for preparing blood agar plates due to its compatibility with a wide range of bacteria. However, if sheep blood is not readily available, horse, rabbit, or goat blood can be used as alternatives.
It is important to note that human blood, especially expired citrated donor blood, should not be used in blood agar preparation. Human blood may contain inhibitory substances that can interfere with the growth of certain pathogens. Additionally, residual antibiotics present in the host’s blood or antibodies, such as anti-streptolysin O (ASO) or anti-M protein antibodies, can hinder the growth of Streptococcus pyogenes. Citrate, commonly found in citrated donor blood, inhibits the growth of beta-hemolytic streptococci. Furthermore, infected human blood may contain other infectious agents, which can complicate the isolation and identification of bacteria.
To summarize, the composition of blood agar includes beef heart peptone, tryptose, sodium chloride, agar, and sheep blood. These ingredients provide the necessary nutrients, solidification, and optimal growth conditions for a wide range of bacteria. It is crucial to avoid using human blood in blood agar preparation due to potential inhibitory substances, residual antibiotics, antibodies, and other infectious agents that may be present.
| Ingredients | Gram/liter |
| Beed heart peptone | 10 gm |
| Tryptose | 10 gm |
| Sodium chloride | 5 gm |
| Agar | 15 gm |
| Sheep blood | 5% |
| Final pH at 25°C 7.3 ± 0.2 |
Principle of Blood Agar
The principle of blood agar revolves around its enriched and nutritious composition, which supports the growth of fastidious organisms. Blood agar can be used with or without the addition of blood, depending on the specific requirements of the organisms being cultured.
When blood is added to the base medium, it provides additional growth factors and nutrients that are essential for the growth of fastidious organisms. The blood acts as a supplement, enriching the medium and supporting the growth of these organisms more effectively.
One important aspect of blood agar is its ability to visualize hemolytic reactions of different bacteria. The hemolytic reactions, which involve the breakdown of red blood cells, can vary depending on the type of animal blood used. Sheep blood is commonly used for detecting hemolytic patterns in Group A Streptococci. However, it may not support the growth of Haemophilus haemolyticus due to its deficiency in pyridine nucleotides. In such cases, horse blood is preferred as it provides better growth and hemolysis for H. haemolyticus. Interestingly, the hemolytic pattern of H. haemolyticus on horse blood may even resemble that of Streptococcus pyogenes on sheep blood.
Apart from the blood component, peptone and tryptose are included in the medium to provide essential nutrients such as carbon, nitrogen, amino acids, vitamins, and minerals required for bacterial growth. Peptone and tryptose are water-soluble, making it easier for the bacteria to absorb these nutrients.
The addition of sodium chloride to the medium helps maintain osmotic equilibrium, ensuring that the medium’s osmotic pressure remains optimal for bacterial growth. It also prevents significant changes in the pH of the medium during bacterial growth.
Distilled water is used to dissolve the nutrients present in the medium, facilitating their absorption by the bacteria.
Agar acts as a solidifying agent in blood agar, providing a stable surface for the organisms to grow on. This allows for the observation of colony morphology and facilitates the enumeration of organisms.
In some cases, phenolphthalein phosphate may be added to the medium. Its purpose is to detect the production of phosphate by Staphylococci. The addition of salt and agar in this context is aimed at assessing surface contamination.
In summary, the principle of blood agar lies in its enriched composition, which provides essential nutrients and growth factors for fastidious organisms. The addition of blood aids in the visualization of hemolytic reactions, although the specific blood type used can impact the results. Peptone, tryptose, sodium chloride, distilled water, and agar all contribute to the medium’s functionality, ensuring optimal growth conditions and the ability to observe colony morphology and hemolytic patterns.
Blood Agar Hemolysis/Greening reaction on blood agar
Hemolysis is the process of destroying red blood cells within the blood because of extracellular enzymes that are produced by specific bacteria. The extracellular enzymes made from these bacteria can be referred to as hemolysins, which radiate outwards from colonies, leading to complete and partial destruction of red blood cells. Different types of hemolysis are visible on blood agar, which can be distinguished from an area of hemolysis within the colonies that are growing.
Four types of hemolysis are produced in sheep blood agar namely; alpha (α) hemolysis, beta (β) hemolysis, gamma (γ) hemolysis, and alpha prime or wide zone alpha hemolysis.

a. Alpha hemolysis on Blood Agar
- Alpha hemolysis (α) is the transformation of red blood cell haemoglobin into methemoglobin in the surrounding medium. This causes the medium to become green or brown in colour.
- The colour is analogous to “bruising” the cells. The cell membrane is intact upon microscopic examination of alpha-hemolyzed red blood cells, indicating that it is not, in fact, lysis.
- Some authors of textbooks refer to alpha as “partial hemolysis,” which might be confusing to students. Importantly, this “partial” or “incomplete” hemolysis should not be confused with the “weak” or “subtle” lysis of Streptococcus agalactiae or Listeria monocytogenes, as described above.
- Never will beta hemolysis result in brown or green staining of the surrounding medium’s cells. Many alpha hemolytic organisms will become clearer after prolonged incubation, but if the surrounding media has any brown or green hues, the “hemolysis” is still labelled “alpha.”
b. Beta hemolysis on Blood Agar
Complete or genuine lysis of red blood cells characterises beta hemolysis (β). The colony is surrounded by a clean zone that approaches the colour and transparency of the base medium. Numerous bacterial species generate toxins that are capable of damaging red blood cells.
Certain species create several poisons or exhibit variable degrees of beta hemolysis.
- One example is the rare Streptococcus pyogenes strain that produces solely an oxygen-labile hemolysin (“Streptolysin O”). In other words, hemolysin is only active when oxygen levels are low. A pour plate, agar overlay, or anaerobic incubation can be used to demonstrate hemolysis. After streaking the agar plate, the simplest technique to produce an anaerobic “pocket” is to “stab” the inoculating loop vertically into the agar. (As depicted in Figure 3, most strains of Streptococcus pyogenes also produce the oxygen-stable hemolysin “Streptolysin S,” which causes lysis in ambient air.)
- Streptococcus agalactiae (Lancefield group B) and Listeria monocytogenes are more examples. For some species, the hemolysin may be generated very slowly or have a poor reactivity. The visible hemolysis may be so mild that it is only discernible immediately beneath the colony (rather than broadly diffused as in S. pyogenes, above). To visualise this extremely mild reaction, the colony can be removed via an inoculating loop, allowing one to observe the lysed cells just beneath where the colony had been developing. (See CAMP technique for additional information on Streptococcus agalactiae and numerous hemolysins.)
c. Gamma hemolysis on Blood Agar
- Gamma hemolysis is also known as non-hemolysis because there is no hemolysis of red blood cells is observed.
- In the end, there is no color change or a hemolysis-like zone is seen under or around the colonies.
- The species like Neisseria meningiditis are not hemolytic or Gamma-hemolytic.
- Gamma hemolysis (γ) is inconsistent with itself. Gamma represents the absence of hemolysis. No reaction should occur in the surrounding media.
d. Alpha prime or wide zone alpha hemolysis
- Alpha prime hemolysis can be defined as small areas of erythrocytes in good condition close to the colony of bacterial cells and includes the complete lysis of RBCs that surrounds the area of intact erythrocytes.
- It could be confused with B-hemolysis due the presence of a clear area within the colonies.
e. Target Hemolysis
- Clostridium perfringens is easily detected in the laboratory by its distinctive “double zone” hemolysis, sometimes referred to as target hemolysis.
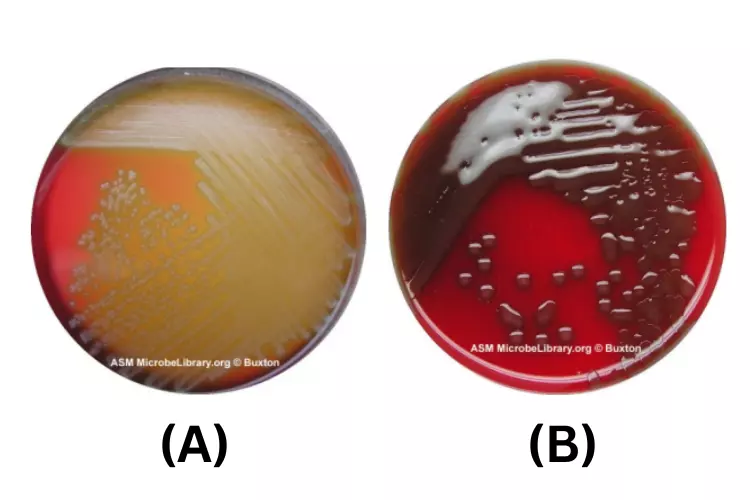
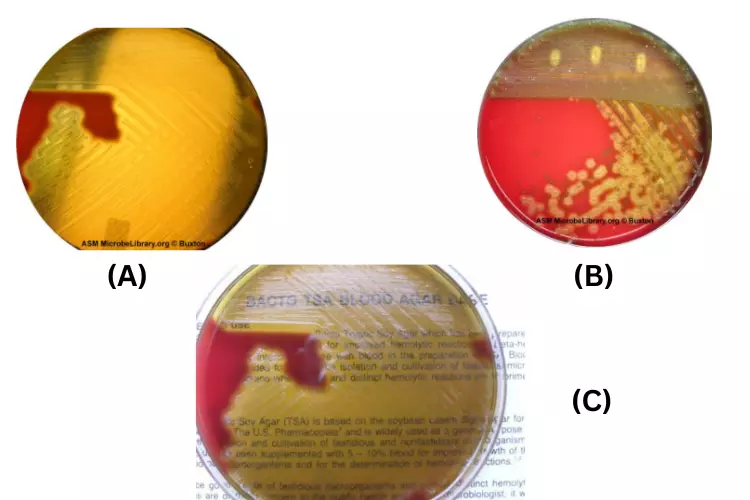
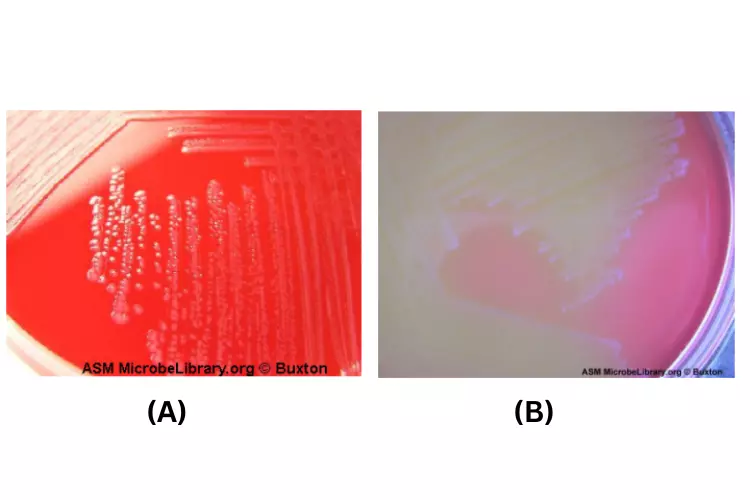
Image of Blood agar plates – Hemolysis on blood agar

Blood agar is a valuable medium for detecting and differentiating hemolytic reactions caused by bacterial species. Hemolysis refers to the lysis or destruction of red blood cells (RBCs) due to the production of extracellular enzymes called hemolysins by certain bacteria. The resulting hemolysis can be observed as distinct zones of different colors or appearances around the bacterial colonies on blood agar.
- Alpha Hemolysis: Alpha hemolysis is characterized by a greenish-grey or brownish discoloration around the bacterial colonies. This discoloration is the result of partial lysis of the red blood cells. The hemolysin produced by the bacteria causes the conversion of hemoglobin in the RBCs to methemoglobin. Some species displaying alpha hemolysis, such as Streptococcus pneumoniae, are part of the normal human flora, while others can cause severe infections like pneumonia.
- Beta Hemolysis: Beta hemolysis is identified by a clear zone of complete hemolysis both underneath and surrounding the bacterial colonies on blood agar. The complete lysis of the red blood cells leads to the formation of colorless products due to the denaturation of hemoglobin. Bacteria displaying beta hemolysis include group A streptococci (e.g., Streptococcus pyogenes) and group B streptococcus (e.g., Streptococcus agalactiae). These bacteria are associated with severe infections in humans.
- Gamma Hemolysis: Gamma hemolysis, also known as non-hemolysis, is characterized by the absence of lysis of the red blood cells. As a result, no change in coloration or hemolysis zone is observed around or beneath the bacterial colonies on blood agar. Species such as Neisseria meningitidis exhibit gamma hemolysis or non-hemolytic behavior.
- Alpha Prime or Wide Zone Alpha Hemolysis: Alpha prime hemolysis is defined by a small zone of intact erythrocytes (red blood cells) adjacent to the bacterial colony, with a surrounding zone of complete lysis of RBCs. This can sometimes be mistaken for beta hemolysis due to the appearance of a clear zone around the colonies.
By observing the hemolytic reactions on blood agar, microbiologists can gain valuable information about the type of hemolysis exhibited by different bacterial species. This information aids in the identification and classification of bacteria and can assist in diagnosing infections caused by specific hemolytic pathogens.
Preparation of Blood Agar
To prepare blood agar, follow these steps:
- Start with a dehydrated blood agar base obtained from a reputable manufacturer. Follow the instructions provided by the manufacturer for the preparation of the base. This usually involves dissolving the dehydrated base in an appropriate amount of distilled water.
- After preparing the blood agar base, sterilize it by autoclaving. Place the prepared base in autoclave-safe containers and subject them to autoclaving at 121°C for 15 minutes. Autoclaving ensures the sterilization of the medium, eliminating any potential contaminants.
- Once the autoclaving process is complete, transfer the sterilized blood agar base to a water bath set to 50°C. Allow the base to cool down to this temperature. The water bath provides a controlled environment to cool the medium evenly.
- When the blood agar base reaches a temperature of 50°C, aseptically add sterile sheep blood to the medium. Gently mix the blood and the agar base to ensure thorough and even distribution. Take care to avoid the formation of air bubbles during mixing. It is recommended to warm the sheep blood to room temperature before adding it to the agar base.
- After mixing, aseptically dispense 15 ml portions of the prepared blood agar into sterile Petri plates. Maintain strict aseptic technique during this step to prevent contamination of the plates. Use a sterile pipette or pouring technique to distribute the medium evenly in each plate.
- Label each plate with the date of preparation and, if necessary, assign it a batch number for identification purposes. Proper labeling ensures accurate record-keeping and tracking of the medium.
- Store the prepared blood agar plates at a temperature of 2-8°C. It is advisable to place the plates in sealed plastic bags to prevent the loss of moisture, which can affect the quality of the medium. Stored properly, the prepared blood agar plates can have a shelf life of up to four weeks.
Note: Before preparing a large batch of blood agar plates, it is recommended to prepare a few plates first to ensure the sterility of the blood used. This step helps identify any potential contamination issues early on and ensures the reliability of the prepared medium.
Storage and self-life of Blood Agar
Storage and shelf-life considerations for blood agar are as follows:
- Storage Temperature: The powdered form of blood agar should be stored in a tightly closed container within a temperature range of 10 to 30°C. This ensures the stability of the components and prolongs the shelf-life of the medium.
- Prepared Medium Storage: Once the blood agar medium has been prepared, it should be stored at a temperature of 20 to 30°C. This temperature range maintains the viability of the medium and supports its optimal performance.
- Protection Against Moisture: Blood agar is hygroscopic, meaning it has a tendency to absorb moisture from the surrounding environment. To prevent lump formation and maintain the quality of the medium, it is essential to tightly cap the container after opening and ensure it is stored in a dry area. This prevents moisture absorption and maintains the consistency of the medium.
- Dry Ventilated Storage: When storing the container with the blood agar medium, it is crucial to keep it in a dry and well-ventilated area. Adequate ventilation helps prevent the build-up of moisture and condensation, which can negatively impact the performance of the medium.
- Protection from Extreme Temperatures and Ignition Sources: The container with the blood agar medium should be protected from extremes of temperature and sources of ignition. Exposure to high temperatures can degrade the components of the medium, leading to reduced effectiveness. Additionally, keeping the medium away from ignition sources ensures safety in the laboratory environment.
- Expiry Date: It is essential to use the blood agar medium before the expiration date mentioned on the label. The expiration date indicates the period within which the medium is guaranteed to perform optimally. Using expired blood agar may lead to unreliable results and compromised microbial growth.
By following these storage guidelines and adhering to the indicated expiry date, the blood agar medium can be effectively stored and maintain its shelf-life for the recommended duration.
Result Interpretation on Blood Agar
Interpreting the results on Blood Agar Medium can provide valuable information about the growth characteristics, colony morphology, and hemolytic patterns of different bacteria. Here is a summary of the growth, colony morphology, and hemolysis observations for various medically important bacteria on Blood Agar Medium:
- Neisseria meningitidis:
- Growth: Good-luxuriant growth
- Colony Morphology: Grey and unpigmented colonies that are round, smooth, moist, glistening, and convex, with a clearly defined edge.
- Hemolysis: Non-hemolytic or gamma-hemolytic.
- Salmonella Typhi:
- Growth: Good-luxuriant growth
- Colony Morphology: Smooth, colorless colonies that are smooth, moist, and flat with a diameter range of 2-4 mm.
- Hemolysis: Non-hemolytic or gamma-hemolytic.
- Staphylococcus aureus:
- Growth: Luxuriant growth
- Colony Morphology: Golden yellow-colored circular, convex, and smooth colonies with a diameter range of 2-4 mm. The colonies may have an opaque appearance with a zone of hemolysis.
- Hemolysis: Beta-hemolytic.
- Staphylococcus epidermidis:
- Growth: Luxuriant growth
- Colony Morphology: Circular colonies with a size of 1-4 mm in diameter, grey to white-colored, low convex elevation, and moist, glistening appearance.
- Hemolysis: Non-hemolytic or gamma-hemolytic.
- Streptococcus pyogenes:
- Growth: Luxuriant growth
- Colony Morphology: White-greyish-colored colonies with a diameter of > 0.5 mm. The colonies are often surrounded by a zone of beta-hemolysis, which is two to four times as large as the colony diameter.
- Hemolysis: Beta-hemolytic.
- Streptococcus pneumonia:
- Growth: Luxuriant growth
- Colony Morphology: Small, grey, moist (sometimes mucoidal in encapsulated virulent strains) colonies with a characteristic zone of alpha-hemolysis (green). The appearance of hemolysis may be dimple-like rather than the typical crater-like appearance due to autolysis.
- Hemolysis: Alpha-hemolytic.
- Pseudomonas aeruginosa:
- Growth: Good-luxuriant growth
- Colony Morphology: Large colonies with a size of 2-5 mm in diameter. The colonies are flat, grey to white-colored, with an undulate margin and may exhibit a zone of beta-hemolysis.
- Hemolysis: Beta-hemolytic.
By observing the growth, colony morphology, and hemolytic patterns on Blood Agar Medium, it becomes possible to identify and differentiate various bacteria based on their distinct characteristics. This information is valuable for diagnostic and research purposes in microbiology.
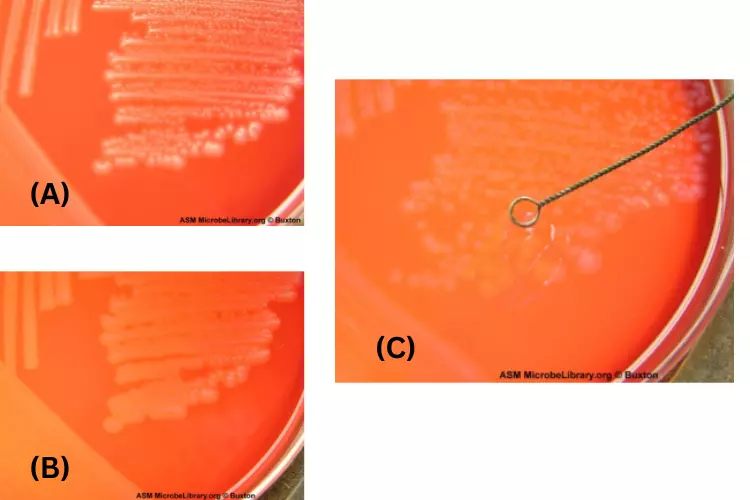
Pseudomonas aeruginosa on blood agar
Pseudomonas aeruginosa is a gram-negative bacterium that can be found in a variety of environments, including soil, water, and plants. It is also a common pathogen that can cause infections in humans, particularly in people with compromised immune systems.
On blood agar, Pseudomonas aeruginosa typically appears as small, shiny, and round colonies that are surrounded by a halo of beta-hemolysis. Beta-hemolysis is the partial or complete lysis of red blood cells, and it can be seen as a clear zone around the colonies on blood agar. Pseudomonas aeruginosa is also a facultative anaerobe, which means that it can grow in the presence or absence of oxygen.
In addition to its characteristic appearance on blood agar, Pseudomonas aeruginosa can also be identified based on its biochemical properties. For example, it is a positive test for the production of the enzymes catalase and oxidase, and it is also a positive test for the production of fluorescein, which is a pigment that can be seen under UV light.
Overall, Pseudomonas aeruginosa is a common cause of infections in humans, and it is important to accurately identify this bacterium in order to initiate appropriate treatment.
Streptococcus pneumoniae blood agar
Streptococcus pneumoniae is a bacterium that can cause a variety of infections, including pneumonia, sinus infections, and ear infections. It is often cultured on blood agar plates in order to identify and study the bacterium. Blood agar is a type of agar plate that contains sheep blood, which allows for the growth of fastidious organisms like S. pneumoniae. The bacteria can be identified on the plate by its characteristic appearance and by the presence of certain enzymes and other metabolic products. Additionally, various biochemical tests can be performed on the culture to confirm the identity of the bacterium.
On a blood agar plate, Streptococcus pneumoniae typically appears as small, round, and white or cream-colored colonies. The colonies may appear translucent or slightly opaque, and they are usually surrounded by a clear zone. This clear zone is caused by the bacterium’s production of a substance called alpha-hemolysin, which breaks down the red blood cells in the agar and causes the blood to appear clear or greenish around the colony. In some cases, the colonies of S. pneumoniae may appear gray or green due to the production of a pigment called pneumolysin. The appearance of the colonies can vary depending on the specific strain of S. pneumoniae and the conditions of the culture.
Streptococcus pyogenes on blood agar
Streptococcus pyogenes is a bacterium that can cause a variety of infections, including strep throat, impetigo, and cellulitis. It is often cultured on blood agar plates in order to identify and study the bacterium. On a blood agar plate, S. pyogenes typically appears as small, round, and white or cream-colored colonies. The colonies may appear translucent or slightly opaque, and they are usually surrounded by a clear zone. This clear zone is caused by the bacterium’s production of a substance called alpha-hemolysin, which breaks down the red blood cells in the agar and causes the blood to appear clear or greenish around the colony. In some cases, the colonies of S. pyogenes may appear gray or green due to the production of a pigment called pyocyanin. The appearance of the colonies can vary depending on the specific strain of S. pyogenes and the conditions of the culture.
Staphylococcus aureus on blood agar
Staphylococcus aureus is a bacterium that can cause a variety of infections, including skin infections, respiratory infections, and food poisoning. It is often cultured on blood agar plates in order to identify and study the bacterium. On a blood agar plate, S. aureus typically appears as small, round, and yellow or golden-colored colonies. The colonies may appear shiny or glossy and are usually surrounded by a zone of clear or greenish-colored fluid. This fluid is caused by the bacterium’s production of a substance called alpha-hemolysin, which breaks down the red blood cells in the agar and causes the blood to appear clear or greenish around the colony. The appearance of the colonies can vary depending on the specific strain of S. aureus and the conditions of the culture.
Enterococcus faecalis blood agar
Enterococcus faecalis is a gram-positive bacterium that is commonly found in the human intestinal tract and is also present in the environment. It is often used as a model organism in laboratory research. When grown on blood agar, E. faecalis can produce small, circular, green-black colonies with a metallic sheen. It is a facultative anaerobe, meaning that it can grow in the presence or absence of oxygen, but it grows better in the presence of oxygen. E. faecalis is resistant to many antibiotics, including penicillins, making it an important pathogen in the hospital setting. It can cause a range of infections, including urinary tract infections, endocarditis, and wound infections.
Quality control of Blood Agar
Quality control of Blood Agar involves specific steps to ensure the reliability and performance of the medium. Here is an outline of the quality control measures for Blood Agar:
- pH Range: Check the pH of the blood agar plates, which should typically range from 7.2 to 7.6 at room temperature. This pH range is important to create an optimal environment for bacterial growth and hemolytic reactions.
- Inoculation: Inoculate one plate with a 5-hour broth culture of Streptococcus pyogenes and another with a 5-hour broth culture of Streptococcus pneumoniae. Additionally, streak a plate with Staphylococcus aureus to perform the Satellitism Test. The Satellitism Test involves streaking S. aureus close to a streak of H. influenzae to observe the interaction between the two bacteria.
- Incubation: Place the inoculated blood agar plates in a carbon dioxide-enriched atmosphere, typically achieved using a CO2 incubator. Incubate the plates at a temperature of 35-37°C overnight. The carbon dioxide-enriched atmosphere promotes the growth of certain bacteria that require this specific condition.
- Growth Characteristics: After incubation, examine the plates for the growth characteristics of each species:
- Streptococcus pyogenes: Look for clear zones of complete hemolysis surrounding the colonies, indicating beta-hemolysis.
- Streptococcus pneumoniae: Observe colonies with a greenish discoloration and a characteristic zone of partial hemolysis (alpha-hemolysis).
- Satellitism of H. influenzae: Examine the streak of H. influenzae and check for the presence of satellite colonies around the streak of Staphylococcus aureus. This indicates the Satellitism phenomenon, where H. influenzae depends on the products released by S. aureus for growth.
By performing these quality control steps, microbiologists can ensure that the blood agar medium is performing as expected and that it provides accurate and reliable results. It helps in verifying the growth characteristics and hemolytic patterns of specific bacterial species, which are crucial for correct identification and interpretation of microbial cultures.
| Organism | Growth | Haemolysis |
| Streptococcus pneumoniae | luxuriant | alpha |
| Streptococcus pyogenes | luxuriant | Beta |
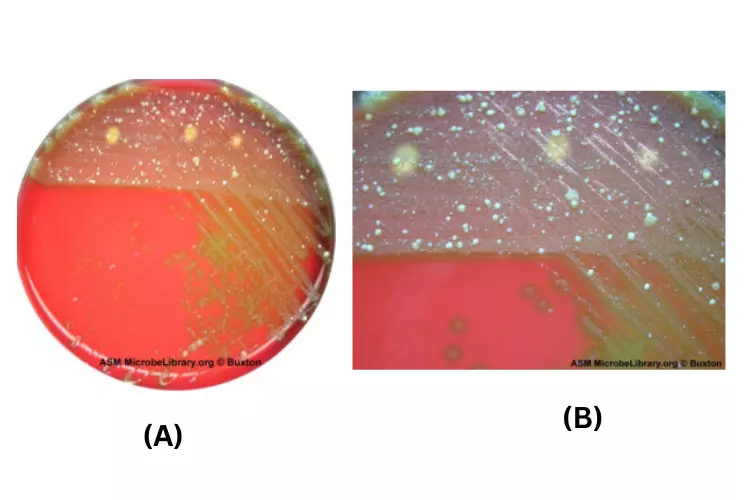
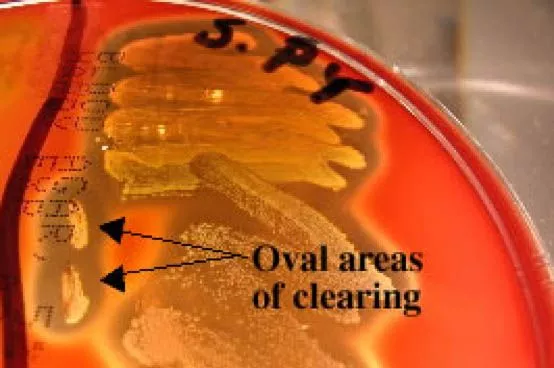
Streak-stab technique
In order to better see hemoloysis patterns, researchers will often puncture multiple holes in the agar with an inoculating loop when inoculating a BAP. A specific hemolysin produced by Streptococcus pyogenes, streptolysin O, can be detected with this jab. Hemolysin is deactivated by oxygen and is only detected below the surface (in anaerobic conditions) around the site of the wound. Streptolysin O is responsible for the oval-shaped clearance around the puncture wounds in the image below.
Types of Blood Agar
1. Blood agar plate
- Blood agar plates (BAPs) typically contain 5–10% concentrations of mammalian blood (often that of sheep or horse). BAPs are enriched, differentiated media used to separate difficult-to-cultivate organisms and detect their hemolytic activity.
- The lysis and complete digesting of red blood cell contents surrounding a colony will be evidenced by β-hemolytic activity. Among the examples is Streptococcus haemolyticus. Due to the conversion of haemoglobin to methemoglobin, α-hemolysis will only induce a partial lysis of the red blood cells (the cell membrane will remain intact) and will result in a green or brown hue. This is illustrated by Streptococcus viridans.
- γ-Hemolysis (or nonhemolytic) describes the absence of hemolytic activity. Additionally, BAPs include beef extract, tryptone, sodium chloride, and agar.
2. Chocolate agar
- Blood cells are lysed on chocolate agar by heating the plate to 80 degrees Celsius. It is used to cultivate finicky respiratory bacteria like Haemophilus influenzae. Chocolate agar gets its name from its colour, however it contains no genuine chocolate.
3. Horse blood agar
- Horse blood agar is a form of microbiological culture medium containing blood. As it is enriched, it permits the growth of specific finicky bacteria and enables the detection of hemolytic activity in these cultures.
4. Thayer–Martin agar
- Thayer–Martin agar is developed to isolate Neisseria gonorrhoeae.
5. Thiosulfate–citrate–bile salts–sucrose agar
- Thiosulfate–citrate–bile salts–sucrose agar promotes growth of Vibrio spp., including Vibrio cholerae.
Uses of Blood Agar
Blood agar has a wide range of uses in microbiology, primarily focused on the cultivation, isolation, and differentiation of various bacteria. Here are the key uses of blood agar:
- Cultivation and Isolation of Fastidious Organisms: Blood agar is particularly useful for the cultivation and isolation of fastidious organisms that have specific nutritional requirements. Examples include Neisseria species and Streptococcus species. The enriched nutrients and growth factors in blood agar support the growth of these organisms, aiding in their isolation and identification.
- Differentiation of Hemolytic Patterns: Blood agar allows for the differentiation of bacteria based on the type of hemolysis they produce. The three types of hemolysis observed are alpha (partial hemolysis), beta (complete hemolysis), and gamma (no hemolysis). The distinct hemolytic patterns exhibited by bacteria on blood agar can provide valuable information for species identification.
- Detection of Phosphate-Producing Staphylococci: Blood agar can be used to detect the production of phosphate by Staphylococci. Phenolphthalein phosphate can be added to the medium, and the appearance of a color change indicates the presence of phosphate-producing Staphylococci.
- Preparation of Salmonella Typhi Antigens: Blood agar is commonly used in the preparation of Salmonella Typhi antigens, which are crucial in diagnosing typhoid fever. The bacteria are cultured on blood agar to obtain the necessary antigens for serological testing.
- Standard Method for Food Sample Analysis: The blood agar base is considered a standard method in the analysis of food samples for the presence of bacterial pathogens. It allows for the isolation and identification of various bacteria that may be present in food, aiding in assessing food safety and quality.
- Isolation, Identification, and Antimicrobial Susceptibility Testing of Streptococci: Blood agar is extensively used for the isolation, identification, and antimicrobial susceptibility testing of Streptococci. Optochin disc or bacitracin disc can be employed to differentiate between different species of Streptococci, and their antimicrobial susceptibility can be determined using the isolated colonies on blood agar.
In summary, blood agar has multiple uses in microbiology, including the cultivation and isolation of fastidious organisms, differentiation of hemolytic patterns, detection of specific bacterial characteristics, preparation of antigens, analysis of food samples, and isolation and identification of Streptococci. It serves as a versatile and valuable medium in various research, clinical, and diagnostic applications.
Limitations of Blood Agar
Blood agar, despite its widespread use and benefits, has certain limitations that should be taken into consideration. These limitations include:
- Inhibition of Haemophilus hemolyticus: Blood agar can inhibit the growth of Haemophilus hemolyticus due to the presence of specific inhibitors in the medium. To overcome this limitation, the inhibitors can be deactivated by heating the medium after adding the blood. This step is necessary to create an environment conducive to the growth of Haemophilus hemolyticus.
- Variability in Hemolytic Patterns: The pattern of hemolysis observed on blood agar may vary depending on the type of blood used. Different animal blood sources, such as sheep, horse, rabbit, or goat, can produce variations in the appearance and intensity of hemolysis. This variability can make the interpretation and differentiation of bacterial species more challenging.
- Similar Growth of H. hemolyticus to Streptococcus Species: When rabbit or horse blood is added to the basal medium, it can support the growth of Haemophilus hemolyticus. However, the growth characteristics of H. hemolyticus can resemble those of Streptococcus species. Therefore, further confirmatory tests or identification methods should be employed to accurately differentiate between these bacterial species.
These limitations of blood agar highlight the importance of using additional tests and techniques to complement the information obtained from blood agar. Supplemental tests, such as biochemical testing, serological assays, or molecular methods, may be required to confirm the identity of specific bacteria and overcome the limitations associated with blood agar.
Greening reaction on blood agar??
It is possible for bacteria growing on blood agar to produce a greening reaction, which is the production of a green pigment called pyocyanin. This pigment is produced by certain species of bacteria, including Pseudomonas aeruginosa and some strains of Staphylococcus aureus. The greening reaction is often seen when these bacteria are grown on blood agar that has been incubated at room temperature for an extended period of time. The green color is produced by the oxidation of the pyocyanin pigment, which can occur when the bacteria are exposed to oxygen.
In some cases, the greening reaction may be accompanied by the production of other pigments, such as pyoverdin, which is a fluorescent green pigment produced by Pseudomonas aeruginosa. The presence of these pigments can be used to help identify specific bacterial species and can also provide information about the metabolic activity of the bacteria.
Important Notes
- Blood is an excellent component of enriched medium for fussy organisms, despite the fact that it includes inhibitors for specific bacterial genera, such as Neisseria and Haemophilus, and that blood agar must be heated to deactivate these inhibitors and release critical growth factors (e.g., V factor). Heating blood agar transforms it into chocolate agar (at 75°C for 15 minutes, it turns chocolate-colored) and promotes the development of these bacteria.
- Hemolysis on blood agar: Streptococci cause primarily three types of hemolysis in Sheep blood agar: Alpha hemolysis, Beta hemolysis, and gamma hemolysis; however, alpha prime or wide zone alpha hemolysis may also occur. Hemolysis is most easily noticed by studying colonies formed in anaerobic circumstances or by viewing colonies beneath the surface. How can one determine whether the colonies observed on a plate caused alpha, beta, or gamma hemolysis? – Principle and interpretation should be followed.
- To determine the type of blood agar hemolysis, the plate must be put up to a source of bright transmitted light and inspected with the light coming from behind.
- Streptococcus pneumoniae has an alpha hemolysis.
- Group A beta-hemolytic streptococci—Streptococcus pyogenes and Group B beta-hemolytic streptococci—Streptococcus agalactiace are beta-hemolytic streptococci. For group A streptococci, the maximum activity of both oxygen-labile SLO and oxygen-stable SLS hemolysins is exclusively detected under anaerobic circumstances.
- Gamma or lack of hemolysis: Enterococcus species
- Alpha prime or wide zone alpha hemolysis: A tiny zone of undamaged erythrocytes immediately close to the bacterial colony, surrounded by a zone of complete red-cell hemolysis. This form of hemolysis can be mistaken for beta hemolysis.
- Some organisms, such as Clostridium perfringens and Aeromonas hydrophilia, exhibit what is known as target hemolysis, which is characterised by a twofold zone of hemolysis on its surface.
- Prepare a small number of blood agar plates before preparing a large quantity to check that the blood is sterile.
- Streptococcus agalactiae CAMP test. -positive blood agar as demonstrated below-
Blood Agar Plate Results – Video
Staphylococcus aureus on blood agar
Streptococcus pyogenes on blood agar
Streptococcus pneumoniae blood agar
FAQ
Is blood agar selective or differential?
Blood agar is a type of culture medium that is used to grow and isolate microorganisms, particularly bacteria. It is made by adding blood to a base agar medium, which is a solidifying agent that is commonly used in microbiology. Blood agar can be either selective or differential, depending on the specific formulation of the medium.
Selective media are designed to favor the growth of certain types of microorganisms while inhibiting the growth of others. For example, blood agar that contains antibiotics such as penicillin can be selective for bacteria that are resistant to the antibiotic.
Differential media are designed to differentiate between different types of microorganisms based on their biochemical characteristics. For example, blood agar that contains an indicator such as phenol red can be differential for bacteria that produce hydrogen sulfide, because these bacteria will cause the indicator to change color.
In general, blood agar is considered to be both selective and differential because it contains nutrients that can support the growth of many types of bacteria, as well as indicators that can be used to differentiate between different types of bacteria based on their biochemical properties.
Why is blood agar useful as a primary isolation medium?
Blood agar is a type of agar media that is used for the primary isolation of bacteria. It is a general-purpose medium that can be used to grow a wide variety of bacteria, including both aerobes and anaerobes. One of the main advantages of blood agar is that it contains red blood cells, which can be used as a source of nutrients for the bacteria. This makes it an excellent medium for growing fastidious bacteria, which are bacteria that have high nutritional requirements and are difficult to grow in other media.
In addition, blood agar can be used to differentiate between different types of bacteria based on their ability to hemolyze (break down) the red blood cells. Some bacteria produce enzymes that can break down the red blood cells, resulting in a zone of clearing around the bacterial colony on the agar. This is known as hemolysis. Different types of hemolysis, such as alpha hemolysis and beta hemolysis, can be used to identify specific bacterial species.
Overall, blood agar is an important tool in microbiology laboratories because it allows for the cultivation and identification of a wide range of bacteria.
What does blood agar test for?
Blood agar is a type of agar media that is used to isolate and identify bacterial species. It can be used to test for the presence of various types of bacteria, including both aerobes and anaerobes.
One of the main uses of blood agar is to determine the ability of bacteria to grow in the presence of red blood cells. The red blood cells in the agar provide a source of nutrients for the bacteria, and the presence of bacterial growth on the agar indicates that the bacteria are able to utilize these nutrients.
Blood agar can also be used to differentiate between different types of bacteria based on their ability to hemolyze (break down) the red blood cells. Some bacteria produce enzymes that can break down the red blood cells, resulting in a zone of clearing around the bacterial colony on the agar. This is known as hemolysis. Different types of hemolysis, such as alpha hemolysis and beta hemolysis, can be used to identify specific bacterial species.
Overall, blood agar is an important tool in microbiology laboratories because it allows for the cultivation and identification of a wide range of bacteria.
what bacteria grows on blood agar?
Blood agar is a general-purpose medium that can be used to grow a wide variety of bacteria. Many different types of bacteria are able to grow on blood agar, including both aerobes and anaerobes. Some examples of bacteria that can grow on blood agar include:
Streptococcus species
Staphylococcus species
Enterococcus species
Haemophilus species
Neisseria species
Bordetella species
Escherichia coli
Salmonella species
Shigella species
Pseudomonas aeruginosa
This is by no means an exhaustive list, as many other types of bacteria can also grow on blood agar. The specific types of bacteria that grow on the medium will depend on the conditions in which it is incubated, as well as the bacterial species present in the sample being tested.
Do all bacteria grow on blood agar?
Not all bacteria are able to grow on blood agar. Blood agar is a general-purpose medium that can support the growth of many different types of bacteria, including both aerobes and anaerobes. However, some bacteria may not be able to utilize the nutrients provided by the red blood cells in the agar, and as a result, may not grow well or may not grow at all on this medium.
Additionally, some bacteria may produce toxins or enzymes that can break down the red blood cells in the agar, resulting in reduced growth or no growth on the medium.
It is important to note that the specific types of bacteria that are able to grow on blood agar will depend on the conditions in which it is incubated, as well as the bacterial species present in the sample being tested.
Why is it called blood agar?
Blood agar is called blood agar because it contains red blood cells. Agar is a type of polysaccharide that is derived from algae and is used as a solidifying agent in the preparation of media for cultivating microorganisms. When agar is combined with blood, it forms a solid gel that is known as blood agar.
The red blood cells in the blood agar serve as a source of nutrients for the bacteria being cultured. They provide a rich source of proteins, lipids, and other nutrients that are essential for the growth and metabolism of many bacterial species. The blood also serves as a good indicator of the ability of the bacteria to utilize the nutrients in the media, as the presence of bacterial growth on the agar indicates that the bacteria are able to utilize the nutrients provided.
In addition to its use as a nutrient source, the blood in blood agar can also be used to differentiate between different types of bacteria based on their ability to hemolyze (break down) the red blood cells. This is why blood agar is an important tool in microbiology laboratories for the cultivation and identification of a wide range of bacteria.
What are the 3 types of hemolysis?
There are three types of hemolysis that can be observed when growing bacteria on blood agar: alpha hemolysis, beta hemolysis, and gamma hemolysis. These terms refer to the ability of the bacteria to break down the red blood cells in the agar, resulting in a zone of clearing around the bacterial colony.
1. Alpha hemolysis: Alpha hemolysis is a type of partial hemolysis that results in the production of a greenish discoloration of the agar surrounding the bacterial colony. This is caused by the production of enzymes that partially break down the red blood cells, releasing the hemoglobin into the agar.
2. Beta hemolysis: Beta hemolysis is a type of complete hemolysis that results in the complete breakdown of the red blood cells, producing a clear zone around the bacterial colony. This is caused by the production of enzymes that completely lyse (break down) the red blood cells.
3. Gamma hemolysis: Gamma hemolysis, also known as nonhemolytic, refers to the lack of hemolysis. In this case, the red blood cells remain intact, and no zone of clearing is observed around the bacterial colony.
The type of hemolysis observed can be used to differentiate between different bacterial species and can also provide information about the metabolic activity of the bacteria.
Is blood agar used for E coli?
Yes, blood agar can be used to isolate and identify Escherichia coli (E. coli). E. coli is a gram-negative bacterium that is commonly found in the human intestinal tract and is also present in the environment. It is an important indicator of fecal contamination and is often used as a marker for the presence of other pathogenic bacteria.
When grown on blood agar, E. coli typically produces small, circular, pink-red colonies with a moist, shiny appearance. It is a facultative anaerobe, meaning that it can grow in the presence or absence of oxygen, but it grows better in the presence of oxygen. E. coli is typically sensitive to a wide range of antibiotics, making it easier to treat than some other bacterial infections. However, some strains of E. coli are resistant to certain antibiotics and can cause serious infections, particularly in people with compromised immune systems.
Overall, blood agar is a useful medium for the cultivation and identification of E. coli and many other types of bacteria.
Why is blood agar used for Staphylococcus aureus?
Staphylococcus aureus is a gram-positive bacterium that is commonly found on the skin and in the nasal passages of humans and animals. It is an important pathogen that can cause a range of infections, including skin infections, wound infections, respiratory tract infections, and food poisoning.
Blood agar is often used to isolate and identify S. aureus because it is a general-purpose medium that can support the growth of a wide range of bacteria, including both aerobes and anaerobes. When grown on blood agar, S. aureus typically produces small, circular, yellow-gold colonies with a smooth, shiny appearance. It is a facultative anaerobe, meaning that it can grow in the presence or absence of oxygen, but it grows better in the presence of oxygen.
In addition to its use for the cultivation of S. aureus, blood agar can also be used to differentiate between different types of S. aureus based on their ability to produce certain enzymes or pigments. For example, some strains of S. aureus are able to produce the enzyme coagulase, which causes the blood in the agar to coagulate (clot). The presence of this enzyme can be used to distinguish S. aureus from other types of staphylococci.
Overall, blood agar is an important tool in microbiology laboratories for the cultivation and identification of S. aureus and many other types of bacteria.
Which factor does blood agar have?
Blood agar is a type of agar media that contains red blood cells suspended in a nutrient-rich medium. The red blood cells provide a source of nutrients for the bacteria being cultured, including proteins, lipids, and other essential nutrients. The blood also contains growth factors, such as vitamins and minerals, which are necessary for the growth and metabolism of many bacterial species.
In addition to the nutrients provided by the blood, blood agar also contains other factors that are important for the growth of bacteria. These include:
Agar: Agar is a type of polysaccharide that is derived from algae and is used as a solidifying agent in the preparation of media for cultivating microorganisms. It provides a solid matrix for the bacteria to grow on and also serves as a source of nutrients.
pH: Blood agar is usually prepared with a pH of around 7.2-7.4, which is neutral to slightly alkaline. This pH range is suitable for the growth of many bacterial species.
Oxygen: Blood agar is typically incubated in the presence of oxygen, which allows for the growth of aerobic bacteria. Some bacteria, such as obligate aerobes, require the presence of oxygen to grow.
Temperature: Blood agar is typically incubated at a temperature of 35-37°C, which is optimal for the growth of many bacterial species.
Overall, the combination of these factors in blood agar makes it a suitable medium for the cultivation and identification of a wide range of bacteria.
Does E coli grow on blood agar?
Yes, Escherichia coli (E. coli) can grow on blood agar. E. coli is a gram-negative bacterium that is commonly found in the human intestinal tract and is also present in the environment. It is an important indicator of fecal contamination and is often used as a marker for the presence of other pathogenic bacteria.
When grown on blood agar, E. coli typically produces small, circular, pink-red colonies with a moist, shiny appearance. It is a facultative anaerobe, meaning that it can grow in the presence or absence of oxygen, but it grows better in the presence of oxygen. E. coli is typically sensitive to a wide range of antibiotics, making it easier to treat than some other bacterial infections. However, some strains of E. coli are resistant to certain antibiotics and can cause serious infections, particularly in people with compromised immune systems.
Overall, blood agar is a useful medium for the cultivation and identification of E. coli and many other types of bacteria.
What is another name for hemolysis?
Hemolysis, also spelled haemolysis and referred to as hematolysis, is the disintegration or death of red blood cells, releasing the oxygen-carrying pigment haemoglobin into the surrounding media.
Is blood agar selective for Gram positive?
Blood agar is not inherently selective for Gram-positive bacteria. In other words, it does not have any properties that inhibit the growth of Gram-negative bacteria or promote the growth of Gram-positive bacteria.
However, blood agar can be made selective for Gram-positive bacteria by the addition of certain agents, such as bacitracin or vancomycin. These agents inhibit the growth of Gram-negative bacteria, while allowing Gram-positive bacteria to grow.
Alternatively, blood agar can be made selective for Gram-negative bacteria by the addition of certain agents, such as polymyxin B or anionic detergents (e.g., sodium lauryl sulfate). These agents inhibit the growth of Gram-positive bacteria, while allowing Gram-negative bacteria to grow.
Overall, the selectivity of blood agar depends on the specific additives that are used in its preparation.
Can Gram positive bacteria grow on blood agar?
Yes, Gram-positive bacteria can grow on blood agar. In fact, many Gram-positive bacteria are able to utilize the nutrients in blood agar for growth, and they may also produce enzymes that can break down red blood cells (hemolysins), leading to the production of visible halos on the agar surface.
However, it is important to note that the growth of Gram-positive bacteria on blood agar may be affected by the presence of certain agents that are added to the agar during its preparation. For example, the addition of bacitracin or vancomycin can make blood agar selective for Gram-positive bacteria, while the addition of polymyxin B or anionic detergents (e.g., sodium lauryl sulfate) can make blood agar selective for Gram-negative bacteria.
Overall, the ability of Gram-positive bacteria to grow on blood agar depends on the specific additives that are used in its preparation, as well as the growth requirements of the individual bacterial species.
Does blood agar show Gram positive or negative?
Blood agar does not inherently show whether a bacterium is Gram-positive or Gram-negative. In other words, it does not have any properties that specifically stain or differentiate between these two types of bacteria.
Gram staining is a laboratory technique that is used to differentiate between Gram-positive and Gram-negative bacteria based on the chemical and physical properties of their cell walls. In order to perform Gram staining, bacteria are first grown on a solid media such as blood agar, and then a series of steps are followed to apply crystal violet and iodine to the bacterial cells, decolorize them with alcohol or acetone, and counterstain them with safranin.
Based on the results of Gram staining, bacteria are classified as either Gram-positive (if they retain the crystal violet-iodine complex and appear purple or blue under the microscope) or Gram-negative (if they lose the crystal violet-iodine complex and appear pink or red under the microscope).
Overall, blood agar is a useful media for growing bacteria, but it is not used for the purpose of Gram staining or differentiation between Gram-positive and Gram-negative bacteria.
Does salmonella grow on blood agar?
Yes, Salmonella can grow on blood agar. Blood agar is a type of nutrient agar that is made by adding heat-inactivated blood (usually from a sheep or horse) to a base of nutrient agar. The blood serves as a source of nutrients for the bacteria, and it also helps to stimulate bacterial growth.
Salmonella is a type of Gram-negative bacteria that can cause a wide range of illnesses, including food poisoning, typhoid fever, and paratyphoid fever. It is an aerobic bacterium, meaning that it requires oxygen to grow and survive.
When grown on blood agar, Salmonella typically appears as small, pink-white or gray-white, circular colonies with a smooth, glossy surface. It may also produce a pitting or dimpling effect on the agar surface, known as “satellite colonies.”
Overall, blood agar is a useful media for the cultivation and identification of Salmonella in the laboratory.
Why is blood agar used when culturing bacteria?
Blood agar is a type of nutrient agar that is used to culture bacteria. It is made by adding heat-inactivated blood (usually from a sheep or horse) to a base of nutrient agar. The blood serves as a source of nutrients for the bacteria, and it also helps to stimulate bacterial growth.
There are several reasons why blood agar is used when culturing bacteria:
- It allows for the identification of bacteria that produce enzymes that can break down red blood cells (hemolysins), leading to the production of visible halos on the agar surface.
- It allows for the identification of bacteria that can utilize certain sugars, leading to the production of acid or gas.
- It allows for the differentiation of bacteria based on their ability to grow at different temperatures.
- It allows for the differentiation of bacteria based on their ability to grow in the presence or absence of oxygen.
Overall, blood agar is a useful tool for the identification and characterization of bacteria in the laboratory.
References
- https://www.wikilectures.eu/w/Blood_agar
- http://www.uwyo.edu/molb2021/additional_info/summ_biochem/bap.html
- https://www.sigmaaldrich.com/IN/en/search/blood-agar*?focus=products&page=1&perpage=30&sort=relevance&term=blood%20agar%2A&type=product_name
- https://www.thermofisher.com/order/catalog/product/R01198
- https://www.thermofisher.com/order/catalog/product/CM0055B
- https://www.microxpress.in/product.php?type=A&c_id=23&id=142
- https://www.srlchem.com/products/product_details/productId/3547
- https://anaerobesystems.com/products/plated-media/columbia-blood-agar-ca/
- https://www.himedialabs.com/in/
- https://universe84a.com/collection/blood-agar/
- https://labmal.com/product/blood-agar-base-500g/
- https://microbiologyinfo.com/blood-agar-composition-preparation-uses-and-pictures/
- https://microbeonline.com/blood-agar-composition-preparation-uses-and-types-of-hemolysis/
- https://www.vumicro.com/vumie/help/VUMICRO/Blood_Agar.htm
- https://asm.org/Protocols/Blood-Agar-Plates-and-Hemolysis-Protocols
- https://www.austincc.edu/microbugz/blood_agar_test.php
