Table of Contents
What is Body Lines of Defense?
- The human body is equipped with a remarkable defense system known as the immune system, which serves as a shield against harmful invaders such as bacteria, viruses, fungi, parasites, and abnormal cells. This intricate network of immune cells, along with vital proteins like cytokines, work together harmoniously to combat and eliminate these pathogenic threats.
- One of the remarkable abilities of the immune system is its capacity to distinguish between molecules that belong to the body itself (self-molecules) and those that are foreign (non-self molecules), with the exception of certain autoimmune diseases. This crucial discrimination is made possible by a group of proteins called Major Histocompatibility Complex (MHC) proteins, which are present on the surface of almost all body cells, except in the case of identical twins.
- There are two distinct types of MHC proteins: MHC I and MHC II. MHC I proteins play a vital role in differentiating the body’s own cells from foreign cells or pathogens. They accomplish this by displaying fragments of antigens, which are characteristic markers found on the surface of cells, thus signaling that these cells belong to the body. This mechanism enables immune cells to recognize and spare healthy cells while effectively targeting and eliminating foreign or infected cells.
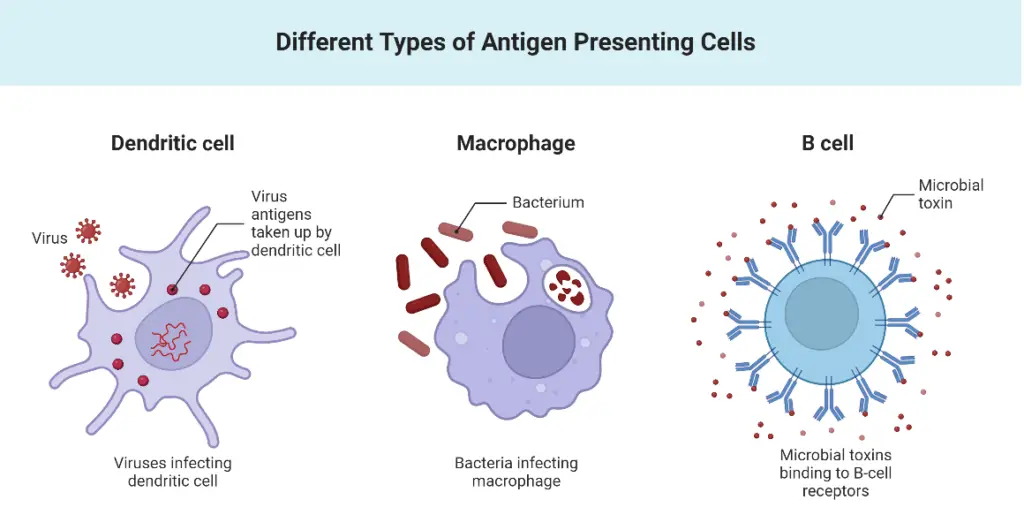
- On the other hand, MHC II proteins are primarily found in a specialized group of immune cells known as antigen-presenting cells (APCs), which include macrophages, dendritic cells, and B cells. These APCs engulf and internalize microbes through a process called phagocytosis, and subsequently, present fragments of the digested microbes on their cell surface using MHC II proteins. By doing so, these immune cells provide a visual representation of the pathogens they have encountered, effectively informing other immune cells about the presence of the invaders.
- It is important to note that red blood cells do not possess MHC proteins. This absence of MHC proteins on red blood cells is essential for their proper function in transporting oxygen throughout the body. While red blood cells do not directly participate in the immune response, they play a critical role in supporting the overall health and functioning of the immune system.
- In conclusion, the immune system relies on the intricate interplay of immune cells and MHC proteins to mount a defense against harmful pathogens. The ability to distinguish between self and non-self molecules, facilitated by MHC proteins, allows the immune system to identify and eliminate foreign invaders while preserving the body’s own cells. This complex system of defense is vital for maintaining optimal health and protecting the body from various diseases and infections.
Defense Systems – Innate and Acquired Defense Systems
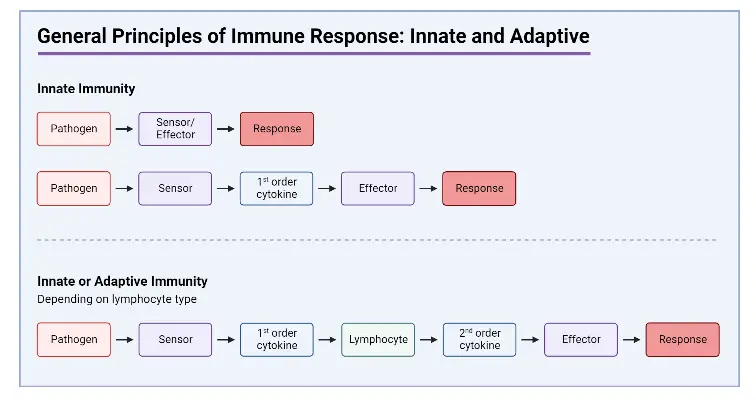
When the body encounters invaders, it deploys two distinct types of responses: the Innate (Natural/Non-specific) response and the Acquired (Adaptive/Specific) response. These responses form the body’s defense systems against foreign particles.
The Innate response remains consistent regardless of the number of exposures to a pathogen, while the Acquired response improves with subsequent encounters. The Innate response is executed by phagocytic cells like neutrophils, monocytes, macrophages, and Natural Killer (NK) cells. In contrast, the Acquired response involves antigen-specific B and T cells, as well as antigen-presenting cells (APCs).
The Innate response acts swiftly upon encountering foreign pathogens, providing an immediate defense mechanism. Conversely, the Acquired response takes a longer time to activate as it requires the recognition and mobilization of specific immune cells.
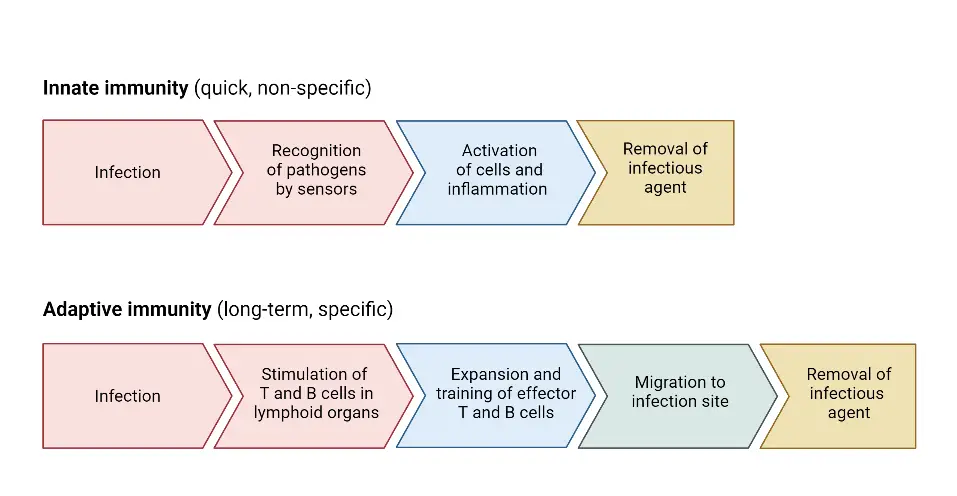
The Innate response is non-specific, combating a broad range of invaders, while the Acquired response is specific, targeting particular types of invaders based on their unique antigens.
These defense systems are further divided into three lines of defense:
- The First line of defense: This initial line of defense includes physical and chemical barriers, such as the skin, mucous membranes, and antimicrobial substances. These barriers serve to prevent the entry of pathogens into the body.
- The Second line of defense: In case the first line of defense is breached, the second line of defense comes into play. It involves the activation of phagocytic cells like macrophages and neutrophils, which engulf and destroy pathogens. Natural Killer (NK) cells also play a crucial role in the second line of defense by recognizing and eliminating infected cells.
- The Third line of defense: The third line of defense encompasses the Acquired response, which is highly specific and adaptive. It involves the activation of B and T cells, which are responsible for producing antibodies and orchestrating a targeted immune response against specific pathogens. This line of defense exhibits memory, allowing the immune system to mount a faster and more effective response upon subsequent exposures to the same pathogen.
1. First Line of Defense
- The first line of defence (or external defence system) consists of physical and chemical barriers that are constantly ready to defend the body against infection. These include your skin, tears, mucus, cilia, stomach acid, urine flow, “friendly” bacteria, and neutrophils, which are white blood cells.
- Pathogenic (disease-causing) bacteria must breach this initial barrier. If this defence is breached, your body’s second line of defence is engaged.
- Surface barriers that prevent viruses from entering the body are the body’s principal defence against infectious disease.
- These surface barriers include intact skin and mucous membranes (which preserve external boundaries) (protect internal boundaries).
- The skin and mucous membranes both secrete chemical substances that inhibit the growth of microorganisms on their surfaces.
- If infections cannot penetrate the host, they cannot interfere with normal physiological activities and cause disease.
Components of First Line of Defense
a. Physical Component – Physical defenses
Physical components of the immune system play a crucial role in protecting the body from pathogens. These components include physical barriers and mechanical defenses that act as the first line of defense against harmful invaders, effectively blocking their entry into the body.
- Skin: One of the primary physical barriers is the skin, which acts as a protective shield. The skin is composed of three layers: the epidermis, dermis, and hypodermis. The outermost layer, the epidermis, consists of tightly packed cells called keratinocytes. These cells contain a protein called keratin, making the skin tough and water-resistant. Additionally, the epidermis constantly sheds dead skin cells, renewing the protective barrier and preventing microbial growth.
- Respiratory system: In the respiratory system, physical defenses come into play. Nasal hairs act as filters, capturing microbes, dust, and dirt present in the air before they can enter the body. These tiny hairs effectively trap particles, preventing them from reaching deeper into the respiratory tract. Moreover, the respiratory tract is lined with microscopic hair-like structures called cilia. These cilia constantly move in coordinated motions, sweeping mucus along the respiratory passages. The mucus serves as a sticky substance that traps foreign particles, including pathogens, and facilitates their removal from the body. Through the mechanism of ciliary action, mucus is directed towards body openings, such as the mouth or nose, where it can be expelled through actions like coughing or sneezing.
- Mucous membranes: Mucous membranes also play a vital role in the body’s defense mechanisms. These membranes line various body tracts, including the respiratory, urinary, and reproductive tracts. Mucous membranes produce mucus, a slimy substance that serves as a physical barrier. Mucus traps foreign particles and pathogens, preventing their entry into deeper tissues. Additionally, the mechanical actions of shedding, coughing, peristalsis (muscular contractions), and the flushing of bodily fluids, like urination and tears, help to remove trapped particles from the body.
Overall, these physical components of the immune system provide a robust defense against pathogens. Through intact skin, nasal hairs, cilia, and mucous membranes, the body establishes formidable barriers that prevent the entry of pathogens and facilitate their removal. These mechanisms work in harmony with other aspects of the immune system to maintain the body’s health and protect it from infections.
b. Chemical Component – Chemical defenses
Chemical defenses are an essential component of the immune system, consisting of various chemicals and enzymes present in body fluids. These chemical defenses help in the destruction of pathogens on the body’s surfaces, at body openings, and within the inner linings of the body.
Here are some chemical defenses in the immune system:
- Body fluids such as sweat, tears, mucus, and saliva contain enzymes that possess antimicrobial properties. For example, lysozyme, found in tears, perspiration, and saliva, can break down the cell walls of bacteria, effectively killing them.
- Secretory IgA is another chemical defense found in body fluids. It functions similarly to lysozyme by attacking the peptidoglycans in the cell walls of bacteria.
- Antimicrobial peptides (AMPs) play a crucial role in defending against pathogens. Examples of AMPs include dermcidin, cathelicidin, defensins, histatins, and bacteriocins. These peptides are produced in response to the presence of pathogens on the skin and help in neutralizing and eliminating them.
- Cerumen, commonly known as ear wax, serves as a chemical defense in the auditory canal. It contains fatty acids that lower the pH between 3 and 5, creating an acidic environment. This acidic environment helps protect the ear canal from foreign particles, including microbes.
- Gastric juice in the stomach is highly acidic with a pH ranging from 2 to 3. Pathogens that enter the stomach through the oral cavity or nasal tract are destroyed by the acidic nature of gastric juice.
- Urine flow, which is acidic in pH, plays a role in eliminating microbes from the urinary system. The acidity of urine helps in killing microbes and directing them out of the body through the urethra.
- Serum, a component of blood, contains unsaturated fatty acids that not only reduce water loss but also inhibit microbial growth. However, it’s important to note that certain compounds in serum can provide nutrition for certain microbes.
These chemical defenses work in conjunction with other components of the immune system to protect the body from pathogens. They help destroy microbes, neutralize their harmful effects, and create an environment that is unfavorable for their growth and survival.
c. Biological Component
Biological components of the immune system involve the presence of friendly and beneficial microorganisms known as resident natural flora. These microorganisms reside in various parts of our body, including the skin, bowel, mouth, gut, and reproductive organs. They play a crucial role in defending against pathogens and maintaining a healthy microbial balance within the body.
Here are somebiological components of the immune system:
- Resident natural flora act as a biological defense by preventing the adherence and colonization of pathogens. They achieve this by creating an acidic environment through the fermentation of sugars into acids.
- The production of acids by resident flora helps create an unfavorable environment for pathogens, hindering their growth and survival.
- These friendly microorganisms occupy cellular binding sites, making it difficult for pathogens to attach and invade host tissues.
- The resident natural flora also compete with pathogens for available nutrients, limiting the resources necessary for the proliferation of harmful microorganisms.
- In addition to their physical and competitive mechanisms, resident normal microbiota contribute to chemical defenses by producing substances called bacteriocins. Bacteriocins are antimicrobial peptides that possess antibacterial activity, aiding in the elimination of potential pathogens.
Overall, the biological components of the immune system provided by resident natural flora are vital for maintaining a balanced microbial ecosystem within the body. Their presence creates a hostile environment for pathogens through the production of acids, occupation of binding sites, competition for nutrients, and the production of bacteriocins. These biological defenses work synergistically with other components of the immune system to protect the body from harmful invaders and promote overall health.
2. Second Line of Defense
- The second line of defense, also referred to as the immune system, plays a crucial role in protecting our bodies against invading pathogens. When the initial barrier provided by the first line of defense is breached, the second line of defense is activated to confront the pathogens head-on. This mechanism involves the activation and participation of various immune cells, particularly white blood cells or leukocytes, including phagocytes, NK cells, dendritic cells, mast cells, and complement proteins. Unlike the adaptive immune response, the second line of defense does not possess immunological memory.
- Once the pathogens manage to surpass the physical and chemical barriers of the first line of defense, they encounter the second line of defense within our bodies. The second line of defense relies on a range of immune cells, each with its own unique functions, to detect and eliminate any non-specific pathogens that have entered the body.
- One type of immune cell that plays a crucial role in the second line of defense is the phagocyte. Phagocytes encompass various cell types, including neutrophils and macrophages, which are capable of engulfing and destroying pathogens through a process called phagocytosis. These cells are equipped with receptors that allow them to recognize and bind to the pathogens, subsequently engulfing them and breaking them down.
- Natural killer (NK) cells are another important component of the second line of defense. These specialized lymphocytes are responsible for recognizing and destroying infected cells, particularly those that have been compromised by viruses or cancerous transformation. NK cells detect abnormalities in the surface proteins of cells and release cytotoxic substances to induce cell death.
- Dendritic cells are crucial antigen-presenting cells that bridge the innate and adaptive immune responses. They capture and process antigens from pathogens, then migrate to the lymph nodes to present these antigens to T cells, initiating an adaptive immune response.
- Mast cells, found in connective tissues, are involved in the inflammatory response. They release chemical mediators such as histamine in response to pathogens or tissue damage, triggering inflammation and attracting other immune cells to the site of infection.
- Complement proteins, a group of plasma proteins, also contribute to the second line of defense. They aid in the destruction of pathogens by forming a membrane attack complex that can lyse the invading microorganisms or enhance phagocytosis by opsonization.
- Unlike the adaptive immune response, which generates immunological memory to mount a faster and more specific response upon subsequent exposure to the same pathogen, the second line of defense lacks this memory aspect. It provides a rapid, non-specific response to a wide range of pathogens, serving as a crucial early defense mechanism to contain and eliminate invading microorganisms.
- In summary, the second line of defense, or the immune system, employs various immune cells such as phagocytes, NK cells, dendritic cells, mast cells, and complement proteins to detect and eliminate non-specific pathogens. Although it lacks immunological memory, the second line of defense acts as an essential line of protection in our bodies, contributing to our overall health and well-being.
Phagocytes (eating cells) and their relatives
Phagocytes, also known as “eating cells,” are a crucial group of immune cells involved in the second line of defense. They play a significant role in engulfing and eliminating pathogens and other foreign substances in the body. Let’s explore some of the key phagocytes and their relatives:
- Basophils: Although they account for only 1% of white blood cells (WBCs), basophils are well-known for their involvement in inflammatory responses associated with asthma and allergies. When stimulated, basophils release substances like heparin and histamine, which contribute to the inflammatory process.
- Mast cells: Similar to basophils, mast cells have functional similarities but are primarily found within tissues. When activated by various inflammatory mediators and antigens, mast cells trigger an inflammatory response. They release granules containing histamine, an inflammatory compound, upon recognizing pathogens.
- Monocytes: Known as the “garbage trucks” or “vacuum cleaners” of the immune system, monocytes make up around 2-6% of WBCs in the blood. These cells are specialized in scavenging and cleaning up cellular debris and pathogens. After leaving the circulation and migrating into tissues in response to inflammation, monocytes differentiate into macrophages and dendritic cells.
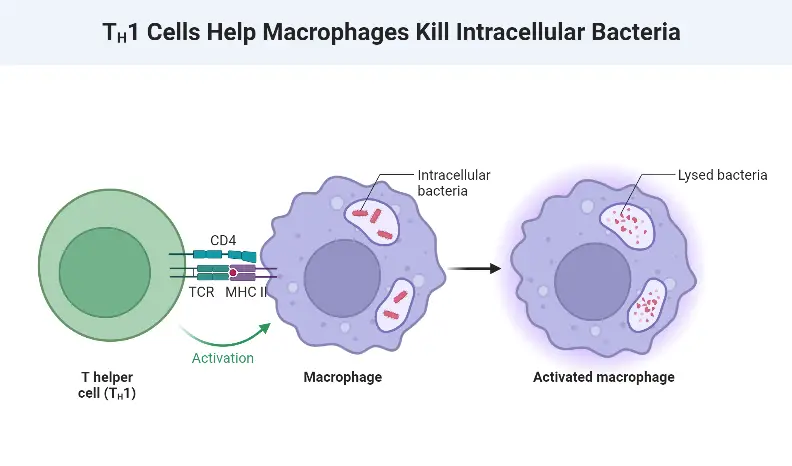
- Macrophages: Macrophages are found in various tissues and organs throughout the body. They engulf and digest pathogens, including cancerous cells, microbes, and cellular debris. Macrophages play an active role in the immune response by releasing regulatory factors like interferons and interleukins, as well as a wide array of chemicals such as enzymes and complement proteins. They also act as “antigen-presenting cells,” presenting engulfed antigens to T cells and activating the adaptive immune system.
- Dendritic cells: Differentiated from monocytes, dendritic cells are present in tissues that come into contact with the external environment, such as the skin, nose, and lungs. These cells serve as a link between innate and adaptive immunity. When they encounter foreign particles, dendritic cells migrate to lymph nodes where they present antigens to T cells and B cells, initiating an adaptive immune response. Their name derives from their distinctive “tree-like” cellular morphology.
- Neutrophils: Neutrophils are the first immune cells to respond to intruders, making up approximately 65% of WBCs. They swiftly migrate out of capillaries to the site of infection and release signals to alert other immune cells, earning them the nickname “patrol tissue.” Neutrophils have a short lifespan of about eight hours after being released from the bone marrow.
- Natural Killer (NK) cells: As the only cytotoxic lymphocytes in the innate immune system, NK cells exhibit rapid responses to virus-infected cells and tumor cells without requiring prior activation. Their “natural” killing ability allows them to detect and control early signs of cancer.
In summary, phagocytes and their relatives, including basophils, mast cells, monocytes, macrophages, dendritic cells, neutrophils, and NK cells, play critical roles in the second line of defense. These cells contribute to the immune response by engulfing and eliminating pathogens, initiating inflammatory responses, presenting antigens, and detecting and destroying infected or cancerous cells. Their combined efforts contribute to the overall effectiveness of the immune system in maintaining our health and well-being.
Mechanism of the second line of defense
- The second line of defense operates through a series of mechanisms aimed at combating invading pathogens. When a pathogen breaches the entry site, neutrophils swiftly come into action to engulf and destroy them. If the pathogens manage to evade neutrophils, macrophages and dendritic cells enter the battle. These cells play crucial roles in phagocytosis, the process of engulfing and internalizing pathogens, as well as presenting antigens to T cells, initiating an adaptive immune response.
- The second line of defense encompasses various internal defense mechanisms, including phagocytosis, natural killer (NK) cells, the inflammatory response, fever, and the complement system. Immune cells and infected cells release different cytokines, which act as signaling molecules to amplify the quantity of cytokine secretion. This triggers an inflammatory response characterized by capillary dilation and increased permeability of the capillary wall.
- Macrophages play a significant role in resolving inflammation and clearing cellular debris at the inflamed site. They contribute to the healing process and ensure the removal of remnants left behind by pathogens. Additionally, cytokines released during the inflammatory response increase the core body temperature, leading to fever. The elevated temperature inhibits microbial growth and accelerates recovery and repair processes.
- NK cells are instrumental in detecting viral-infected cells or cancerous cells, inducing apoptosis, or programmed cell death. They serve as a surveillance mechanism, recognizing and eliminating aberrant cells that pose a threat to the body.
- Furthermore, the complement system, composed of various complement proteins present in the blood serum, plays a crucial role in the second line of defense. Complement proteins are attracted to pathogens that have been tagged by the adaptive immune system. A cascade of binding events occurs, coating the pathogen and serving as a marker for phagocytes to recognize its presence. This opsonization process facilitates the recognition and digestion of pathogens through phagocytosis.
- Overall, the second line of defense operates through a coordinated effort involving phagocytosis, NK cells, the inflammatory response, fever, and the complement system. These mechanisms work together to identify, eliminate, and neutralize invading pathogens, ultimately safeguarding the body against infections and promoting recovery and repair processes.
3. Third Line of Defence (Adaptive Immune System)
- The third line of defense, also known as the adaptive immune system, is acquired during an individual’s lifetime and provides specific and targeted immunity against pathogens. Unlike innate immunity, which is present from birth, the adaptive immune system exhibits characteristics such as long-lasting immunity, a robust immune response, and immunological memory. It takes time to develop an adaptive immune response, with a lag period between initial exposure and the maximal response. However, upon repeated exposure to the same antigen, the adaptive immune system responds quickly and efficiently to eliminate the pathogen.
- The primary function of the adaptive immune system is to identify, destroy, and remember specific pathogens. It comes into action only when pathogens successfully bypass the first and second lines of defense. The main cellular components involved in the third line of defense are antigen-presenting cells (APCs), B lymphocytes (B cells), and T lymphocytes (T cells).
- Lymphocytes, which include T cells, B cells, and natural killer (NK) cells, account for approximately 20-30% of white blood cells (WBCs) and are predominantly found in the lymphatic system, hence the name lymphocytes. T cells and B cells are integral components of the adaptive immune response, while NK cells primarily function in the innate immune response, as mentioned earlier.
- The adaptive immune system employs two primary mechanisms: the humoral immune response and the cell-mediated immune response. The humoral immune response involves the production of antibodies by B cells, which are specialized proteins that bind to specific antigens on pathogens. These antibodies can neutralize pathogens, promote their destruction, and facilitate their removal from the body. The humoral immune response is particularly effective against extracellular pathogens.
- On the other hand, the cell-mediated immune response relies on the actions of T cells. T cells have various subsets, including helper T cells, cytotoxic T cells, and regulatory T cells, each with specific functions. Helper T cells assist in activating B cells and cytotoxic T cells, promoting an effective immune response. Cytotoxic T cells directly target and destroy infected cells or cancerous cells. Regulatory T cells play a crucial role in maintaining immune homeostasis by suppressing excessive immune responses.
- The adaptive immune system possesses a remarkable ability to develop immunological memory. Once the immune system has encountered a specific pathogen, memory B and T cells are generated. These memory cells “remember” the pathogen and can mount a faster and more efficient immune response upon subsequent exposure. This immunological memory is the basis for long-lasting immunity provided by vaccines.
- In summary, the third line of defense, or the adaptive immune system, is not present at birth but acquired during an individual’s lifetime. It provides targeted immunity against specific pathogens, exhibits immunological memory, and generates long-lasting immunity. The key players in the adaptive immune system are antigen-presenting cells, B cells, and T cells, which work together to mount a tailored immune response. The humoral immune response, mediated by B cells and antibodies, and the cell-mediated immune response, involving T cells, are integral components of the adaptive immune system’s defense mechanisms.
Humoral or antibody-mediated immune response
- The humoral or antibody-mediated immune response is a vital component of the adaptive immune system, primarily orchestrated by B cells. When B cells come into contact with a pathogen, they are activated and initiate the production of antibodies that are subsequently released into the bloodstream. The name “B” cell originated from an experiment conducted by Max Cooper in the 1960s. He demonstrated that antibody production was significantly impaired in irradiated chickens after the surgical removal of the Bursa of Fabricius, the primary site of B cell development in birds.
- B cells originate and mature in the bone marrow. They possess diverse antigen-specific molecules on their outer surface, known as B cell receptors (BCRs), which enable them to detect specific antigens. When naive B cells encounter an antigen in the lymphatic system, they undergo clonal expansion, leading to the generation of a large number of identical B cell clones. Some of these clones differentiate into two distinct cell types: memory B cells and plasma B cells (also known as plasma cells or effector B cells).
- Plasma B cells play a pivotal role in the humoral immune response as they are responsible for the secretion of antibodies, also referred to as immunoglobulins (Igs). These antibodies are released into the bloodstream and have various functions, including neutralizing pathogens, promoting their destruction, and facilitating their clearance from the body. Each plasma B cell produces a specific type of antibody that recognizes and binds to a particular antigen.
- Memory B cells are another crucial component of the humoral immune response. These cells provide the immune system with long-lasting memory of previously encountered antigens. When the immune system encounters the same antigen in the future, memory B cells quickly recognize it and mount a rapid and robust immune response. This immunological memory is the basis for long-lasting immunity against specific pathogens and is the underlying principle of vaccination.
- In summary, the humoral or antibody-mediated immune response involves the activation and differentiation of B cells. These specialized immune cells produce and secrete antibodies, known as immunoglobulins, into the bloodstream. Plasma B cells are responsible for antibody secretion, while memory B cells contribute to long-term immunity by providing a rapid and effective immune response upon re-exposure to a previously encountered antigen. The humoral immune response plays a vital role in neutralizing pathogens, promoting their elimination, and conferring long-lasting immunity against specific diseases.
Mechanism of antibody-mediated immune response
The mechanism of the antibody-mediated immune response involves a series of steps that contribute to the generation of specific antibodies and their subsequent actions against antigens. Here is a breakdown of the key events:
- Recognition of Antigen: B cells possess specific B cell receptors (BCRs) on their surface, which can bind to antigens that match their receptor. When a B cell encounters its matching antigen, the antigen binds to the BCR on the B cell’s surface.
- Internalization and Processing: Once the antigen binds to the BCR, the B cell internalizes the antigen through a process called endocytosis. The internalized antigen is then digested into smaller fragments within the B cell.
- Presentation of Antigen Fragments: The processed antigen fragments are displayed on the B cell’s surface, bound to unique Major Histocompatibility Complex II (MHC II) molecules. This complex acts as a signal for mature helper T cells that recognize the specific antigen-MHC II combination.
- Activation of Helper T Cells: The mature helper T cells, which possess T cell receptors (TCRs) specific to the antigen presented by the B cell, interact with the antigen-MHC II complex. This interaction triggers the secretion of cytokines, such as interleukins, by the helper T cells.
- Stimulation of B Cell Proliferation: The cytokines and other secretions from the helper T cells act as signals that stimulate mitosis, or cell division, in the B cells. This stimulation leads to the multiplication of the activated B cells.
- Differentiation into Plasma and Memory Cells: As a result of B cell proliferation, some B cells mature into plasma cells, which are specialized for antibody production. These plasma cells secrete large amounts of antibodies into the bloodstream. Additionally, some B cells differentiate into memory B cells, which provide long-term immunity and can rapidly respond to future exposures to the same antigen.
- Antibody Actions: The antibodies secreted by plasma cells circulate throughout the body and bind to antigens, forming antigen-antibody complexes. These complexes can be cleared off through various mechanisms, including the complement cascade, which leads to the destruction of the antigen-antibody complexes. Antibodies can also neutralize pathogens by blocking their ability to infect host cells, promote agglutination (clumping) of pathogens for easier recognition and elimination, and facilitate precipitation of soluble antigens for their removal.
In summary, the mechanism of the antibody-mediated immune response involves the recognition of antigens by B cells, internalization and processing of antigens, presentation of antigen fragments, activation of helper T cells, stimulation of B cell proliferation, differentiation into plasma and memory cells, secretion of antibodies by plasma cells, and subsequent actions of antibodies against antigens. These steps collectively contribute to the clearance and elimination of pathogens and provide long-term immunity against specific antigens.
Cell-mediated immune response
The cell-mediated immune response is primarily orchestrated by T lymphocytes, along with antigen-presenting cells (APCs) like macrophages, B cells, and dendritic cells, as well as various cytokines. Unlike the humoral immune response, it does not rely on antibodies and is particularly effective against viruses and cancerous cells. Let’s explore the different types of T lymphocytes involved in this immune response:
- T-Helper Cells (TH or CD4+ T cells): These specialized cells play a crucial role in coordinating the immune response. They secrete cytokines, such as interleukins, that stimulate the division and maturation of B cells into plasma and memory cells. T-helper cells also activate macrophages, enhancing their phagocytic capabilities, and promote clonal expansion of other T-helper cells, amplifying the immune response.
- T-Killer Cells (Tc or CD8+ T cells): T-killer cells are responsible for eliminating infected or cancerous cells. They recognize specific antigens displayed on the surface of target cells. Once activated, T-killer cells secrete cytotoxins or create holes in the target cell’s membrane using perforin. This disrupts the target cell’s integrity, leading to cell lysis (cell rupture) or apoptosis (programmed cell death).
- T-Suppressor Cells (Treg or Regulatory T cells): T-suppressor cells play a crucial role in maintaining immune balance. They serve as a built-in mechanism to prevent excessive immune reactions and help prevent autoimmune diseases. Once the pathogen has been defeated and the immune response needs to be dampened, T-suppressor cells downregulate T cell-mediated immunity, ensuring that the immune system returns to a balanced state.
- T-Memory Cells: T-memory cells are formed after the initial exposure to an antigen. These cells “remember” the antigen and remain in the body for an extended period. If the same antigen reappears, T-memory cells are quickly triggered to differentiate into cytotoxic T cells, capable of recognizing and eliminating the pathogen more efficiently. This process enables a faster and more effective immune response upon subsequent encounters with the same antigen.
The cell-mediated immune response demonstrates the critical role of T lymphocytes in coordinating and executing immune responses against specific pathogens and cancerous cells. Through the actions of T-helper cells, T-killer cells, T-suppressor cells, and T-memory cells, this immune response provides targeted and tailored defense mechanisms to eliminate threats to the body.
Mechanism of cell-mediated immune response
The mechanism of the cell-mediated immune response involves a series of interactions and signaling events between antigen-presenting cells (APCs) and T cells. Here is an overview of the key steps:
- Antigen Presentation: APCs, such as macrophages, B cells, or dendritic cells, internalize antigens and present antigenic fragments on their surface attached to Major Histocompatibility Complex II (MHC II) proteins. This complex allows the antigen to be recognized by naïve T cells.
- T Cell Activation: Naïve T cells, which possess T cell receptors (TCRs) on their surface, interact with the antigen-MHC II complex through their TCRs. This interaction is supported by several costimulatory interactions between the T cell and the APC. The T cell and APC engage in a cross-talk where the APC releases interleukins, while the T cell secretes cytokines and interferons.
- Effector T Cell Differentiation: Through the cross-talk, the secretion of cytokines and interferons induces the differentiation of naïve T cells into subsets of effector T cells. Helper T cells (TH) are activated by the release of IL-1 and differentiate into subsets that promote cellular immunity. TH cells also secrete IL-2, which leads to the proliferation of cytotoxic T cells (TC) and B cells.
- Stimulation of B Cell Differentiation: Helper T cells play an indirect role in promoting humoral immunity. They stimulate B cells through cytokine signaling, helping in their differentiation into plasma cells and memory B cells. Plasma cells secrete antibodies (immunoglobulins), contributing to the humoral immune response.
- Cytotoxic T Cell Activity: Cytotoxic T cells (TC) are involved in directly eliminating pathogens or infected cells. They secrete cytotoxins and release perforins, which can destroy pathogens by creating holes in their cell membranes or inducing apoptosis (programmed cell death) in infected cells.
Through these mechanisms, the cell-mediated immune response facilitates the coordination and activation of different subsets of T cells, leading to effective immune responses against pathogens and infected cells. The interaction between APCs and T cells, coupled with the release of cytokines and signaling molecules, ensures the appropriate differentiation of effector T cells, promotion of cellular immunity, and indirect support to humoral immunity through the stimulation of B cell responses.
Immunity Disorders
The Immune System can be inefficient if it fails to identify aberrant cells as malignant cells, or it can be overprotective and create other issues.
Allergies
- Hypersensitivity of the immune system to relatively harmless environmental antigens – the immune system reacts to an external material that it would ordinarily ignore – allergy kinds (food, dust, mould, seasonal), symptoms, and signs (skin rash, itching, red bumps, sneezing).
Asthma
- An obstructive pulmonary disorder characterised by recurrent spasms of bronchial wall muscles followed by edoema and mucus production that makes breathing difficult – it causes the airways of the lungs to swell and narrow, resulting in wheezing, shortness of breath, chest tightness, and coughing.
- Extrinsic asthma, often known as allergic asthma, is more prevalent (90% of all cases) and typically begins in childhood.
- Intrinsic asthma accounts for around 10% of all cases. It commonly manifests after the age of 30 and is typically unrelated to allergies. Inhaler containing drugs such as albuterol to open airways.
Autoimmune Disorder
- A disorder in which the immune system erroneously targets and destroys healthy human tissue – more than 80 different types – because the immune system cannot distinguish between healthy body tissue and antigens.
- Normal bodily tissues are destroyed as a result of an immunological reaction. This response is a hypersensitivity reaction comparable to the allergic response.
- Addison’s disease, Celiac disease – (gluten-sensitive enteropathy), Graves disease, Hashimoto’s thyroiditis, Multiple sclerosis, Myasthenia gravis, Pernicious anaemia, Rheumatoid arthritis, Systemic lupus erythematosus, and Type I diabetes are examples of autoimmune (or immune-related) conditions.
AIDS
- AIDS (acquired immune deficiency syndrome) is the last stage of HIV disease, which causes severe damage to the immune system due to infection with the human immunodeficiency virus (HIV).
Tissue Rejection – Foreign MHC Proteins
- White blood cells recognise the body’s tissues by searching for a set of antigens on the surface of each cell.
- The most essential of them constitute the main histocompatibility complex (MHC).
- Self-antigens – Protein markers of the major histocompatibility complex (MHC) – Two groups
- Class I MHC markers are expressed on all cell types except for RBCs.
- Class II MHC molecules are expressed on mature B-cells, some T-cells, and antigen-presenting cells.
- Doctors screen the MHC of potential organ donors to determine the greatest match.
Blood typing problems
ABO System RBC surface membranes contain proteins that serve as antigens in some receivers.
- Blood type A contains solely A antigens.
- Blood type B contains solely B antigens.
- Blood type AB has both A and B antigens.
- Blood type O is devoid of both A and B antigens.
- Blood plasma contains antibodies specific for blood types that are not present.
- Exposure to foreign blood antigens causes agglutination or clustering of RBCs, halts blood circulation, and causes RBCs to explode.
Rh System problems
- Another significant antigen utilised in blood type matching.
- Rh positive individuals have Rh factor on the RBC membrane; Rh negative individuals lack the Rh factor protein.
- Individuals who are Rh-negative do not have antibodies to the Rh factor, but develop immunity when exposed to it.
- HDN can arise when the mother is Rh-negative and the newborn is Rh-positive.
- Mother is only “inoculated” with a small amount of baby’s blood (and Rh protein) before delivery.
- The mother develops antibodies that are small enough to cross the placenta and are capable of destroying the baby’s red blood cells; the mother receives a booster at each birth; hence, the risk to subsequent infants increases.
- The problem is remedied by administering anti-Rh antibodies to the mother, generally after the birth of the baby, which attack any of the baby’s RBCs remaining in the mother’s blood before the mother can form antibodies.
FAQ
What are the body’s lines of defense?
The body’s lines of defense refer to the mechanisms and systems in place to protect the body from pathogens and foreign invaders. They are categorized into three lines: the first line of defense, the second line of defense, and the third line of defense (adaptive immune system).
What is the first line of defense?
The first line of defense includes physical and chemical barriers that prevent pathogens from entering the body. Examples include the skin, mucous membranes, tears, saliva, stomach acid, and beneficial bacteria in the body.
What is the second line of defense?
The second line of defense, also known as the innate immune system, involves non-specific immune responses that target a wide range of pathogens. It includes immune cells like phagocytes, natural killer cells, complement proteins, and the inflammatory response.
What is the third line of defense?
The third line of defense, known as the adaptive immune system, is a specific immune response that develops after exposure to pathogens. It involves the production of antibodies and the activation of T cells and B cells to target and eliminate specific pathogens.
How does the first line of defense work?
The first line of defense works by creating physical barriers, such as the skin and mucous membranes, which act as a physical barrier to prevent pathogens from entering the body. Additionally, chemical barriers like stomach acid and enzymes in bodily secretions help kill or neutralize pathogens.
What are the main cells involved in the second line of defense?
The main cells involved in the second line of defense are phagocytes (e.g., neutrophils, macrophages), natural killer cells, dendritic cells, and mast cells. These cells recognize and eliminate pathogens through processes like phagocytosis, release of cytotoxic substances, and activation of inflammatory responses.
How does the third line of defense provide immunity?
The third line of defense provides immunity by generating a specific response to pathogens. B cells produce antibodies that bind to and neutralize specific antigens, while T cells recognize and destroy infected cells. This response creates immunological memory, leading to a faster and more efficient immune response upon re-exposure to the same pathogen.
What is the role of antibodies in the immune system?
Antibodies, also known as immunoglobulins, are proteins produced by B cells. They recognize and bind to specific antigens on pathogens, marking them for destruction by other immune cells or neutralizing their harmful effects.
How does the immune system recognize self from non-self?
The immune system is capable of distinguishing between self and non-self through a mechanism called self-tolerance. Immune cells undergo a process of education and selection, ensuring they do not attack the body’s own cells and tissues.
How do the lines of defense work together to protect the body?
The lines of defense work collaboratively to provide comprehensive protection. The first line of defense acts as a physical and chemical barrier, while the second line of defense responds rapidly to eliminate pathogens. The third line of defense, the adaptive immune system, provides targeted and long-term immunity. Together, these lines of defense help maintain the body’s health and protect against various diseases and infections.
References
- https://www.sciencelearn.org.nz/resources/177-the-body-s-first-line-of-defence#:~:text=The%20first%20line%20of%20defence,white%20blood%20cells%20called%20neutrophil.
- https://www.news-medical.net/health/What-are-the-Three-Lines-of-Defense.aspx
- https://ib.bioninja.com.au/standard-level/topic-6-human-physiology/63-defence-against-infectio/lines-of-defense.html
- https://letstalkscience.ca/educational-resources/stem-in-context/immune-response
- https://opentextbc.ca/biology/chapter/12-2-innate-immunity/
- https://www.khanacademy.org/science/high-school-biology/hs-human-body-systems/hs-the-immune-system/a/hs-the-immune-system-review
- https://www.immunology.org/public-information/bitesized-immunology/cells
- https://www.austincc.edu/apreview/EmphasisItems/Inflammatoryresponse.html#ISF
- https://rsscience.com/white-blood-cells/
- https://www.soinc.org/sites/default/files/uploaded_files/2018_IMMUNE_SYSTEM_HANDOUT.pdf
- https://universe-review.ca/R10-40-Immune.htm
- https://bio.libretexts.org/Courses/Manchester_Community_College_(MCC)/Remix_of_Openstax%3AMicrobiology_by_Parker_Schneegurt_et_al/13%3A_Innate_Nonspecific_Host_Defenses/13.01%3A_1st_Line_defense-_Physical_and_Chemical_Defenses
- https://www.sciencelearn.org.nz/resources/178-the-body-s-second-line-of-defence
