Table of Contents
Epidermophyton floccosum is a type of filamentous fungus which causes nail and skin infection in human beings. The anthropophilic dermatophyte may cause diseases like tinea pedis (athlete’s foot) and tinea cruris, tinea corporis and even onychomycosis. The diagnostic methods for fungal infection are physical examination, testing for culture, and molecular examination. Treatment for fungal infections that are applied topically includes using terbinafine, itraconazole, voriconazole and ketoconazole are usually effective.
E. floccosum, is among two species of the family of Epidermophyton. In the 20th century, it was the 4th most frequent cause of dermatophytosis North America. The ascomycete is widespread in its distribution, but is more frequently isolated from patients living in subtropical and tropical regions. The fungus is non-soil-associated and does not have any specific growth requirements and displays distinctive smooth club-shaped macroconidia when examined under the microscope.
Morphology of Epidermophyton floccosum
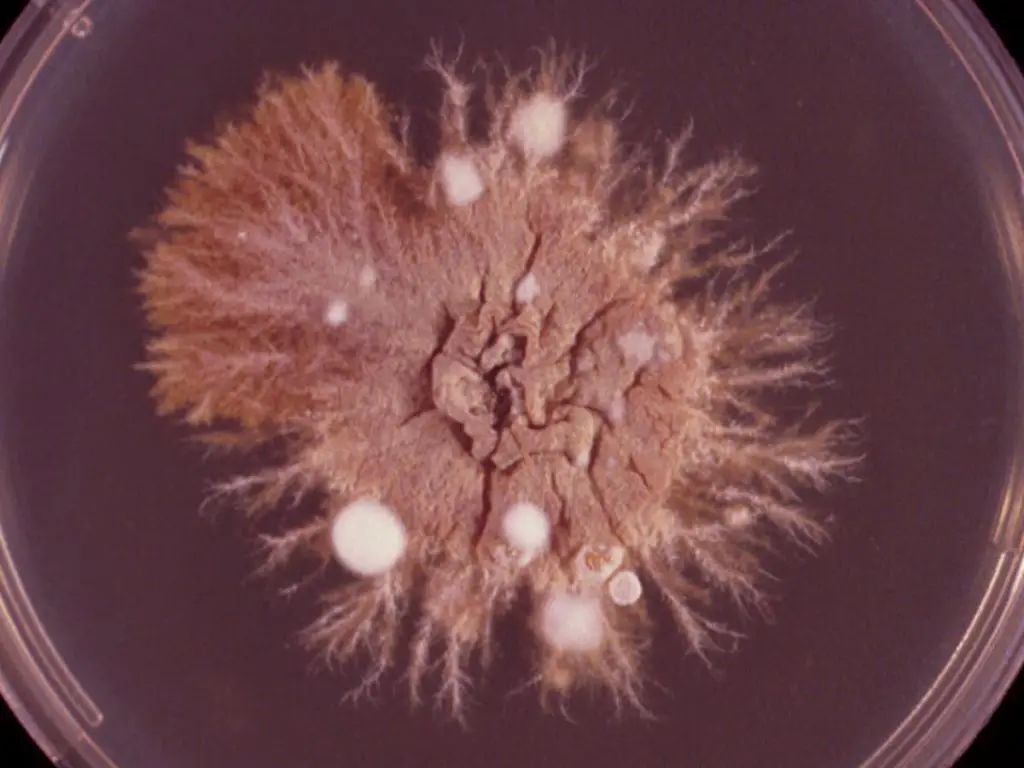
- Colonies from E. floccosum tend to be slow-growing, khaki or greenish brown with a suede-like appearance, with a fold at the center, and with a smooth periphery, and a growing fringes that are submerged, however above the image, they lack these characteristics because they are young cultures ( nine days incubation at 25°C).
- The older cultures can develop mycelium with white pleomorphic tufts.
- A deep yellowish-brown reverse color is common.
- Microscopic morphology reveals the characteristic macroconidia with thin, smooth walls which typically form in clusters that grow directly from hyphae (specific characteristic is that they have the hyphae racquets as seen in the above image).
- Numerous chlamydospores have been formed in older cultures , whereas microconidia do not form.

Habitat of Epidermophyton floccosum
E. floccosum is a species with global distribution but is found more frequently in subtropical and tropical regions. Fungal infections from the past were reported by US military personnel in Vietnam in Vietnam and British Army in Southeast Asia. E. floccosum is thought to be the fourth most frequent cause of dermatophytosis North America. With around 20 percent US instances in addition to 44 % of Asian cases, it’s also the third most prevalent cause of tinea pedis in the world in the world, after Trichophyton mentagrophytes as well as Trichophyton rubrum.
Pathogenesis of Epidermophyton floccosum
Like other fungal dermatophytes, E. floccosum has keratinase which allows it to break down keratin in the nails, skin, and hair. Recent research has demonstrated that it is able to infect the eyes and cause the condition known as keratitis. E. floccosum is unable to penetrate living tissues in people who have normal immunity that causes the infection to remain in the nonliving cornified layer (stratum of the cornea) of the epidermis. Wood’s lamp cannot be used to determine the presence of E. floccosum infection since the fungus is not able to shine under ultraviolet light.
Macroscopic Morphology of Epidermophyton floccosum
Macroscopic Morphology on petri dish
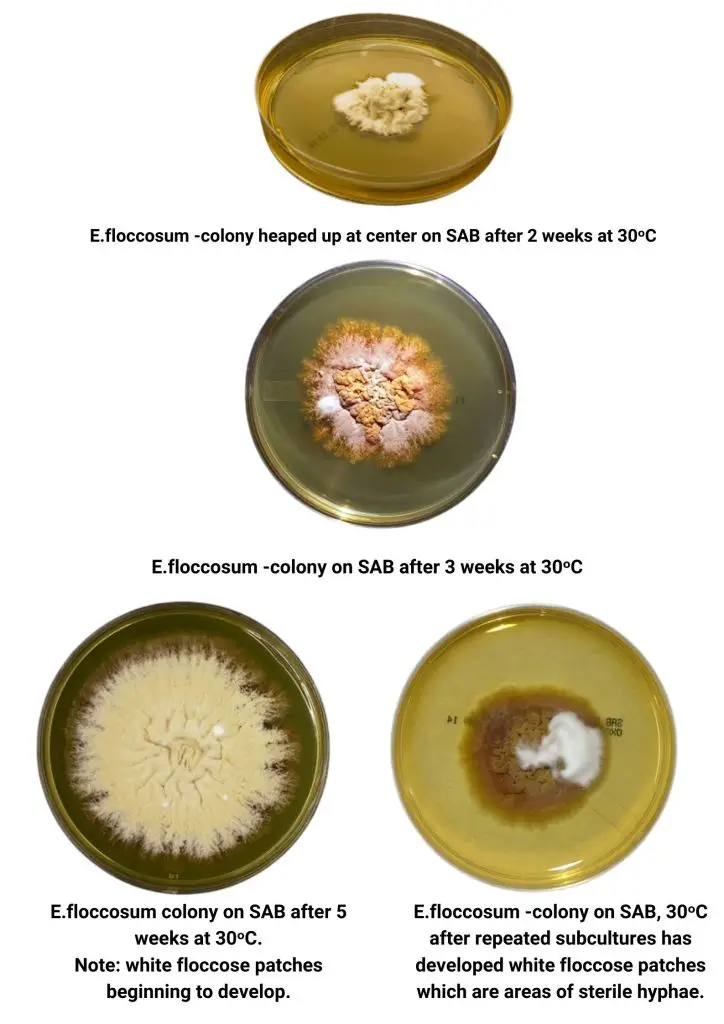
E.floccosum shows moderate growth, maturing between 10-14 days. Surface colonies (media affected) are described as yellowish mustard or mustard brown, ranging from olive-grey to (khaki) in color. Colonies can be powdery smooth or felty and may develop a folded appearance as the growth accelerates. After a long period of incubation, the sterile, floccose (hairy) white mycelia can be found covering the colony. The reverse can be described as ochre. It ranges from mustard-yellow to yellow-brown, and even orange-colored.
Microscopic Morphology
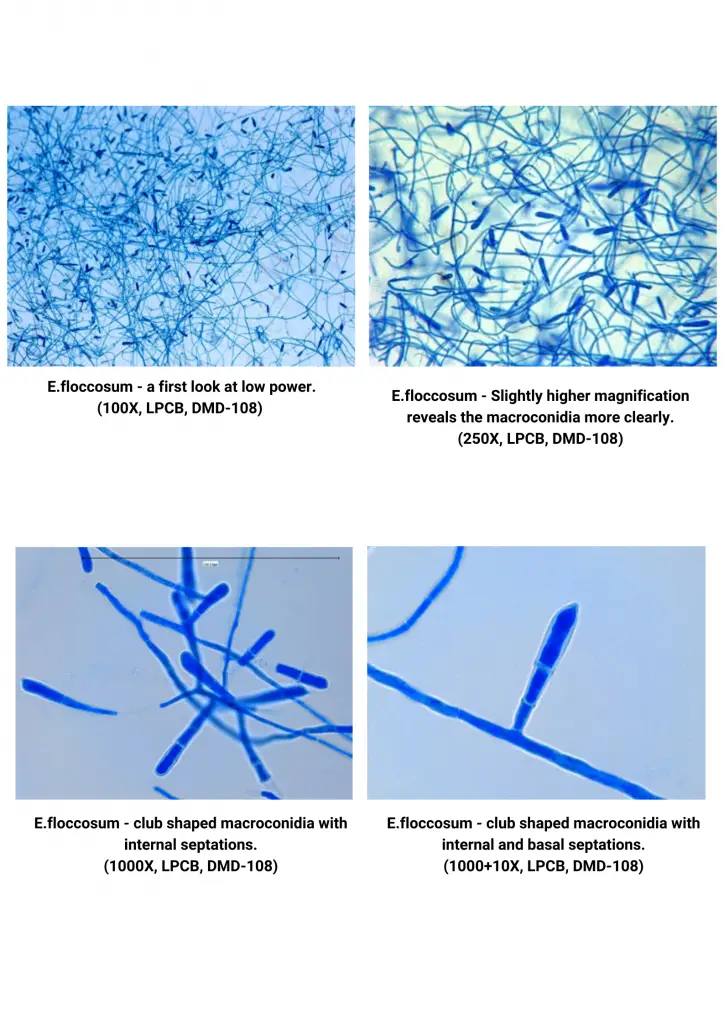
E.floccosum contains septate hyphae, however microconidia aren’t produced, that distinguish it from other genera of Dermatophytes. Macroconidia grow as terminal or lateral outgrowths from mature hyphae. They first lack a basal septum. The macroconidia with a thin wall (10 40 um x 6-12 um) comprise 2 to five cells. They can be found in distinct clusters or singly. As the culture matures and macroconidia develop, they can transform to chlamydoconidia (chlamydospores) which is why they’re best seen early in the development. They are smooth-walled and clavate (club shape) and have a sharp point. It is also distinct against Microsporum as well as Trichophyton.
Clinical Manifestations of Epidermophyton
1. Tinea pedis or Athlete’s foot
- It’s the ringworm fungal infection of the feet that involves interdigital webs as well as the sole.
- The most commonly observed clinical sign is an intertriginous condition that is which is associated with maceration, swelling as well as fissuring and erythema that is characterized by burning and itching sensations.
- The most commonly used agents that cause the problem include E. floccosum T. rubrum as well as T. mentagrophytes.
- It is very common for office workers and athletes and is due to the regular wearing of synthetic nylon socks that do not retain sweat.
2. Tinea cruris or Jock itch or Dhobie’s itch
- It’s a ringworm that affects the inguinal area that involves the perianal, groin and perineal, and thigh areas. It is most commonly seen in an upper part of the thigh.
- The most common dermatophytes include T. rubrum T. mentagrophytes as well as E. floccosum.
- It is most commonly seen in students who typically wear tight, synthetic undergarments where sweat doesn’t absorve and the presence of moisture can cause fungal infections.
3. Tinea corporis
- Ringworm of the glabrous skin. The lesions are well-marginated with an erythematous border that is raised.
- The scaly, annular patches can coalesce into an extensive area of chronic inflammation.
- The most common causative agents for Dermatophytes include T. rubrum T. mentagrophytes and T. tonsurans and there is the possibility of E. floccosum.
- It has been observed to be more prevalent in people who have a medical history of the disease in their family and can be passed on via the direct contact of other infected people.
- Tinea capitis is the 2nd most significant clinical manifestation in people who have a familial history of condition. This is due to the fact that these illnesses can be transmitted via fomites like combs hairbrushes, bedding towels, pillows, clothes or furniture. Additionally tinea corporis may be caused by unhygienic personal hygiene as well as heavy manual work.
4. Tinea unguium or onychomycosis
- It’s the ringworm disease that affects the nail plate.
- The distal subungual infection is the most common type and affects the nail bed and the underside of the nail’s distal part.
- It is hard thin, flexible, and thickened and could crack as a result of the accumulation of subungual debris.
- The nail’s color tends to be black or brown.
- The most common species responsible for onychomycosis is tinea unguium. T. rubrum T. mentagrophytes and E. floccosum.
- It is a common practice in the household of servants and housewives because of the habit of cleaning the cowshed without gloves as well as washing the kitchen appliances with ash, as well as frequently dipping hands in soapy water, all of which increase the risk of fungal infection.
Laboratory Diagnosis of Epidermophyton infections
- Microscopic Examination: This can be performed using 10-20% potassium hydroxide without or with calcofluor and the specimen’s nail or skin.
- Cultural Examination: Performed Utilizing an inhibitory mold agar or SDA medium that contains cycloheximide as well as chloramphenicol, which inhibits the growth of bacterial and mold. Colonies usually grow slowly and greenish-brown to khaki-colored, with a suede-like texture which is raised and folded into the middle, with an elongated periphery, and a an underwater fringe of growth.
- LPCB Tease mount for Microscopic appearance: A colony has been teased, and LPCB mount is constructed to show the hyphae and spore. LPCB mount is created to show the hyphae as well as the spore ( conidia). Conidia comes in two forms i.e. Microconidia:small unicellular
- Macroconidia:- Multicellular, septate
- Special hyphae:- hyphae such as racquet hyphae as shown above picture.
- Biochemical test: Among biochemical test, Urease test can be used to detect Epidermophyton infections. Epidermophyton species shows negative result in urease test.
Other methods of diagnosis:
- Hair perforation test:- Fungi penetrate hair, causing wedge-shaped perforations.
- Positive:- Trichophyton mentagrophytes and Microsporum canis.
- Negative: Epidermophyton species
- Molecular methods: PCR assay: A number of PCR tests can be used and some of them are
- The PCR-Restriction Fraction Length Plormophism (PCR-RFLP) can be used identify the 12 species that trigger Dermatophytosis-related infections.
- Real-time PCR can also be used to detect E. floccosum following fungal elimination
Spread of Epidermophyton infections
E. floccosum is able to live for long durations by forming arthroconidia inside skin scales. Arthroconidia are spores that have thick walls and greater resistance to drying and hot environments than mycelium. Arthroconidia form can allow E. floccosum persist for many years in baths, showers towels, swimming pools sheets, blankets, shoes, and other clothings.The bacteria are typically spread by contact with showers and gym facilities.
Treatment of Epidermophyton infections
Tnea pedis, tinea cruris and tinea corporis are treated tropically using naftifine, terbinafine, butenafine, clotrimazole, ketoconazole,econazole miconazole,sulconazole, oxiconazole, cyclopyrox, and tolnaftate while tinea unguium onychomycosis(nail infections) The topical treatment for nail infections is typically ineffective, therefore, the use of systemic oral therapy over a long period of time is recommended.
Prevention and control Epidermophyton infections
- Avoid touching lesions on the skin or nails of those who have been infected.
- Wearing loose-fitting clothing in the affected regions.
- Maintaining a good hygiene practice when participating in activities that require close contact between skin and human
Reference
- Clinical Microbiology Procedure Handbook, Chief in editor H.D. Isenberg, Albert Einstein College of Medicine, New York, Publisher ASM (American Society for Microbiology), Washington DC.
- A Text-Book of Medical Mycology. Editor: Jagdish Chandar, Publication Mehata, India.
- Medical Mycology. Editors: Emmons and Binford, 2nd ed 1970, Publisher Lea and Febiger, Philadelphia.
- Practical Laboratory Mycology. Editors: Koneman E.W. and G.D. Roberts, 3rd ed 1985, Publisher Williams and Wilkins, Baltimore.
- https://universe84a.com/epidermophyton-general-characteristics/
- https://www.semanticscholar.org/paper/A-clinicomycological-study-of-dermatophytic-in-a-Mk-V./fb4734528338f1a0cdf3433b7ed66e92435509d1
- http://thunderhouse4-yuri.blogspot.com/2015/09/epidermophyton-floccosum.html
- https://moviecultists.com/what-does-epidermophyton-floccosum-cause
- https://en.wikipedia.org/wiki/Epidermophyton_floccosum
- https://www.sciencedirect.com/topics/medicine-and-dentistry/epidermophyton-floccosum
- https://www.creative-biolabs.com/drug-discovery/therapeutics/epidermophyton-floccosum.htm
- https://www.adelaide.edu.au/mycology/fungal-descriptions-and-antifungal-susceptibility/dermatophytes/epidermophyton
