Table of Contents
Sporothrix schenckii is a globally distributed fungus that was first isolated from a human specimen in 1896 by medical student Benjamin Schenck. The species is found in soil as well as on living and decaying plant matter, such as peat moss, and in soil. It is capable of infecting both humans and animals and is the agent responsible for sporotrichosis, also known as “rose handler’s disease.” The most prevalent route of infection is through a cut or puncture wound in the skin, through which spores enter the body. Infections are common in otherwise healthy individuals, but they are rarely fatal and treatable with antifungals. It is found in the environment as filamentous hyphae. In host tissue, it manifests as yeast. The temperature-dependent transition between the hyphal and yeast forms makes S. schenckii a thermally dimorphic fungus.
| Kingdom: | Fungi |
| Division: | Ascomycota |
| Class: | Sordariomycetes |
| Order: | Ophiostomatales |
| Family: | Ophiostomataceae |
| Genus: | Sporothrix |
| Species: | S. schenckii |
Morphology of Sporothrix schenckii
Sporothrix schenckii can exist in either hyphal or yeast morphology. The hyphal form is commonly found on vegetation and decomposing matter. When a fungus transforms into a host, yeast-like morphology predominates.
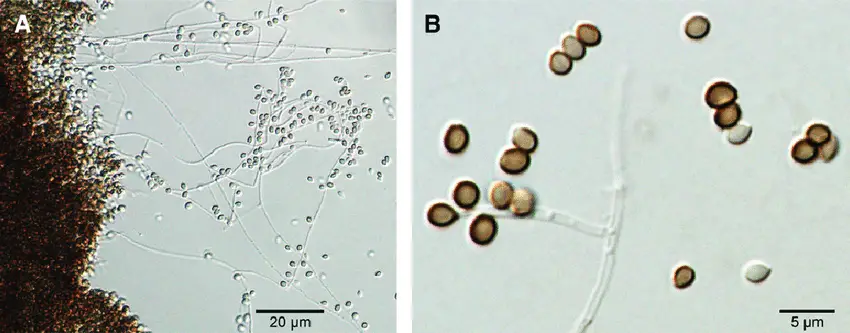
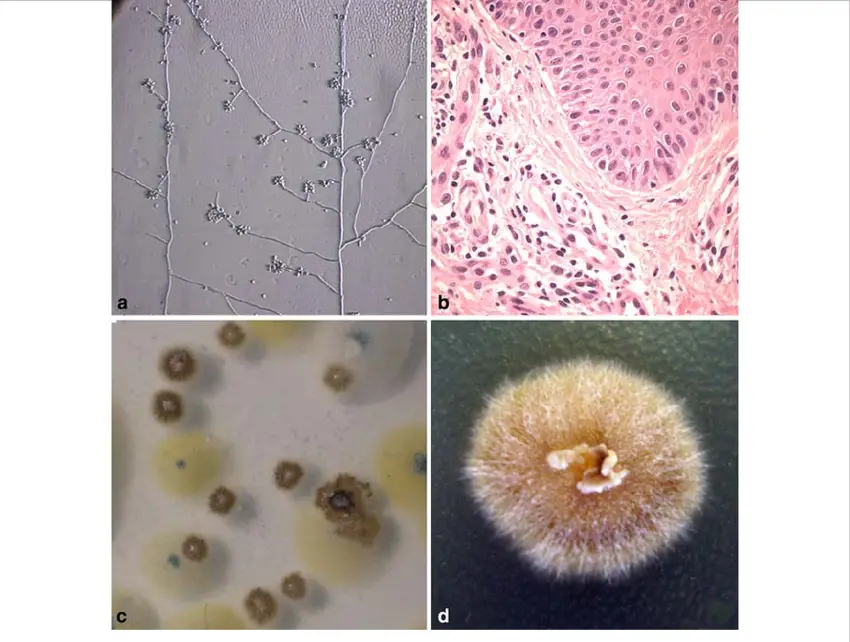
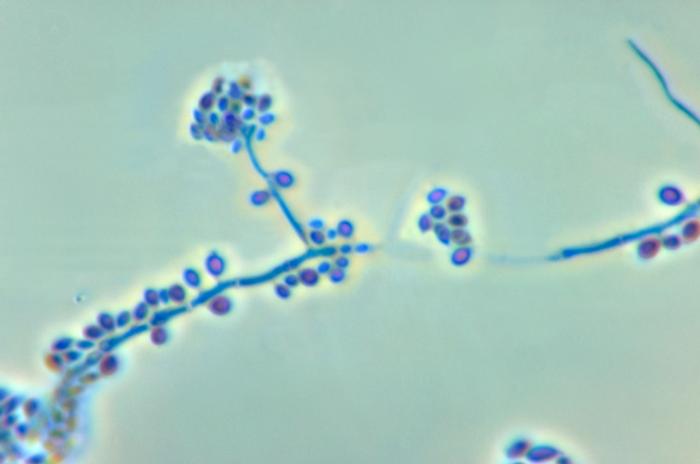
Hyphal
At 25 °C (77 °F) in the environment or in the laboratory, S. schenckii adopts its hyphal form. Macroscopically, filaments are visible and colonies have a surface that is moist, leathery to velvety, and exquisitely wrinkly. The colour may alter from white to cream to dark brown (“dirty candle-wax” colour) as time passes. Microscopically, hyphae are approximately 1 to 2 μm in diameter and are septate. Conidia are oval-shaped and appear to be made of glass (hyaline). They may be colourless or of a dark hue. Conidia are occasionally described as resembling a flower.
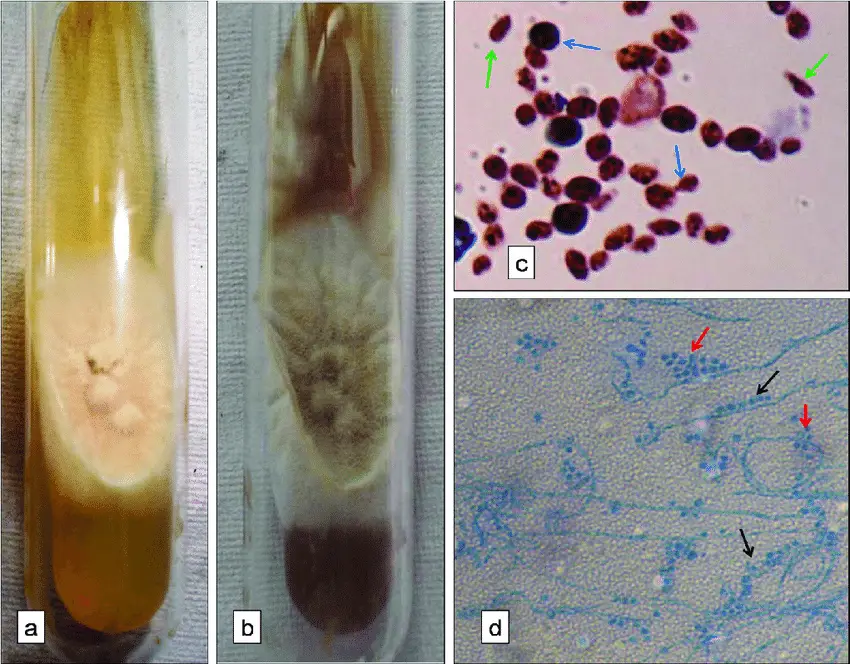
Yeast
S. schenckii acquires its yeast form at 37 °C (99 °F), whether in a laboratory or in a host tissue. The yeast form appears macroscopically as uniform white or off-white colonies. Yeast cells are between 2 and 6 μm in length and exhibit a cigar-shaped morphology.
Habitat of Sporothrix schenckii
Sporothrix schenckii is a fungus that is ubiquitous in the natural world. However, it can also be found on plants and in decomposing organic matter. The fungus is most prevalent in regions with mild and humid climates.
Sporothrix schenckii is the fungus responsible for sporotrichosis, an infection that can affect the epidermis, lymph nodes, and bones. The most prevalent route for Sporothrix schenckii infection is through a puncture wound that introduces the fungus to the skin. Additionally, the fungus can be inhaled or ingested, but these routes of infection are less prevalent.
Sporotrichosis symptoms vary depending on the site of infection. Typically, skin infections manifest as a small, red, painful or irritating bump. The protrusion may then develop into a long, ulcerated, raised sore that can spread along the lymph node’s path. Infections of the bones can cause pain, edoema, and sensitivity.
Typically, antifungal drugs are used to treat Sporothrix schenckii. The type of medication and duration of treatment will be determined by the infection’s severity. Sporotrichosis is typically a curable infection.
Here are some locations where Sporothrix schenckii is located:
- Soil
- Plants
- Decomposing organic matter
- Wood
- Straw
- Moss
- Flowers
- Thorns
- Fur
- Hair
- Water
- Air
Cultural Characteristics of Sporothrix schenckii
Sporothrix schenckii is a dimorphic fungus, which means it can exist in both a filamentous and yeast form. When the fungus is expanding in its natural environment, it assumes the filamentous form. When the fungus is proliferating inside the body, it assumes the form of yeast.
Sporothrix schenckii’s filamentous variety is a branching, septate fungus that grows at 25°C. The hyphae have a diameter of 1-2 micrometres and are hyaline. Tear-shaped to clavate (club-shaped) conidia are generated in clusters on small, densely packed denticles.
Sporothrix schenckii yeast is a round to oblong, budding yeast that grows at 37 degrees Celsius. The cells have a flat surface and a diameter between 2 and 4 micrometres.
Sporothrix schenckii can be cultured at 25°C or 37°C on Sabouraud dextrose agar (SDA). At 25°C, the filamentous form will grow on SDA, while at 37°C, the yeast form will proliferate. Additionally, the fungus can be grown on blood agar, chocolate agar, and other media.
Here are some of Sporothrix schenckii’s cultural characteristics:
- Temperature: The filamentous variety of Sporothrix schenckii grows optimally between 25 and 30 degrees Celsius (room temperature). Sporothrix schenckii yeast flourishes optimally at body temperature (37 degrees Celsius).
- Media: Sporothrix schenckii can thrive on a variety of media, including blood agar, chocolate agar, and Sabouraud dextrose agar.
- Growth rate: Sporothrix schenckii is a fungus that grows slowly. The fungus can take up to 10 days to develop in culture.
- Morphology: Sporothrix schenckii’s filamentous form is a branching, septate fungus that develops in long, thin filaments. The filaments are typically white or grey in hue and can reach a maximum length of 100 microns. The yeast form of Sporothrix schenckii is a 2-4 microns in diameter, single-celled, round or oblong fungus. Yeast is typically cream or white in colour.
- Pigmentation: Sporothrix schenckii is devoid of pigmentation.
- Microscopic appearance: The filamentous form of Sporothrix schenckii can be observed as branching, septate hyphae under a microscope. Microscopically, the yeast form of Sporothrix schenckii consists of single-celled, round or oval yeast cells.
- Biochemical reactions: Sporothrix schenckii is non-fermentative and produces no pigments in biochemical reactions.
- Pathogenicity: In its natural environment, the fungus Sporothrix schenckii is nonpathogenic. However, if it enters the body through a break in the epidermis, it can cause an infection in humans. The condition is known as sporotrichosis. Typically, sporotrichosis is a moderate infection that can be treated with antifungal drugs. In some instances, the infection can become more severe and spread to the lungs, bones, and joints.
Transmission of Sporothrix schenckii
Sporothrix schenckii is transmitted to humans predominantly through traumatic inoculation into the skin. The most prevalent mode of transmission is direct contact with infected plant material or contaminated soil. Here are the primary modes of Sporothrix schenckii gearbox:
- Traumatic Inoculation: The most prevalent mode of transmission occurs when the fungus enters the body through a puncture wound, laceration, or scratch caused by contaminated plant material, such as thorns, splinters, or barbs. The fungus can be found in soil, decomposing plant matter, and plant detritus.
- Occupational Exposure: Due to their frequent contact with soil and vegetation, those who work in occupations such as gardening, agriculture, horticulture, forestry, and landscaping are at a greater risk of exposure to Sporothrix schenckii. This occupational exposure may increase the likelihood of traumatic infection.
- Zoonotic Transmission: Sporothrix schenckii can infect animals, including cats, canines, and horses, via zoonotic transmission. Transmission of zoonotic diseases occurs when humans come into contact with the skin, fur, or secretions of an infected animal, especially through wounds or bites. Manipulating or grooming an infected animal without taking the necessary precautions can result in transmission.
- Rare Modes of Transmission: In uncommon instances, sporotrichosis can be transmitted via inhalation of fungal spores, particularly in immunocompromised individuals. Person-to-person transmission has been reported in extremely rare instances, typically in the context of intimate and protracted skin-to-skin contact.
Pathogenesis of Sporothrix schenckii
Sporothrix schenckii’s pathogenesis entails a complex interaction between the fungus and the host’s immune response. Here is an overview of the process of pathogenesis:
- Entry and Adhesion: Sporothrix schenckii enters the body through traumatic inoculation, typically through a puncture wound or abrasion of the epidermis. The fungus can be found in soil, decaying plant matter, and contaminated plant matter. It has adhesion molecules on its surface that allow it to adhere to cells and tissues of the host.
- Dimorphic Transformation: Sporothrix schenckii endures a temperature-dependent dimorphic transformation following germination. It exists at ambient temperature (25-30°C) as the mycelial form, which is prevalent in nature. Once it enters the host’s tissues and encounters the elevated temperature of the body (37°C), the fungus transforms into its pathogenic yeast form.
- Invasion of Tissues: The invasive phase of Sporothrix schenckii is the yeast form. It can invade host tissues, including skin, subcutaneous tissue, lymphatic vessels, and occasionally other organs. The fungus produces enzymes and factors that aid in the invasion and devastation of tissue.
- Immune Response: The immune response of the host is essential to the pathogenesis of sporotrichosis. The outcome of the interaction between Sporothrix schenckii and the immune system can vary. In immunocompetent individuals, the immune response typically limits the infection to a localised form. The recognition and phagocytosis of the fungal cells involve macrophages, neutrophils, and T cells.
- Lymphatic System Preference: Sporothrix schenckii has a special affinity for the lymphatic system. It is capable of infecting and replicating within lymphatic vessels, causing characteristic nodular or ulcerative lesions along lymphatic channels. The infection can travel along lymphatic vessels proximally, forming a chain of lesions known as “sporotrichoid spread.”
- Chronic and Disseminated Infections: In some cases, sporotrichosis can progress to a chronic or disseminated form, particularly in individuals with compromised immune systems. In such instances, the infection may spread to deeper tissues, bones, and joints, as well as internal organs.
Virulence Factors of Sporothrix schenckii
Sporothrix schenckii possesses a number of virulence factors that contribute to its pathogenesis and infectivity. Despite the fact that our understanding of the specific virulence factors of Sporothrix schenckii is still evolving, the following factors have been identified:
- Thermal Dimorphism: Sporothrix schenckii demonstrates a dimorphic lifestyle, capable of switching between two morphological forms: mycelial (mould) form at ambient temperatures and yeast form at higher temperatures, including human body temperature. This ability enables the fungus to adapt to diverse environments, thereby facilitating tissue invasion and host survival.
- Adhesion Molecules: Sporothrix schenckii expresses a number of adhesion molecules on its surface, allowing it to adhere to host cells and extracellular matrix components. These adhesion molecules facilitate the initial attachment of the pathogen to the tissues of the host, thereby facilitating the onset of infection.
- Extracellular Enzymes: Sporothrix schenckii generates extracellular enzymes that aid in tissue invasion and pathogenesis. These enzymes, which degrade host tissue proteins, lipids, and elastin, include proteases, lipases, and elastases. By degrading host components, fungi are able to penetrate and invade host tissues, thereby facilitating the establishment and spread of infection.
- Melanin Production: Sporothrix schenckii is capable of producing the pigment melanin, which contributes to its virulence. Melanin protects fungi from host immune defences, including oxidative stress and phagocytosis. Additionally, it possesses immunomodulatory properties and can inhibit host immune responses.
- Evasive Strategies: Sporothrix schenckii possesses mechanisms to evade and modulate the immune response of the host. It can inhibit the phagocytic activity of host immune cells, such as macrophages, thereby reducing their ability to eliminate fungal cells. Altering the production of cytokines and other immune signalling molecules, the fungus can influence the immune response and promote its survival within the host.
Clinical Manifestations of Sporotrichosis
Sporotrichosis is a fungal infection caused by the dimorphic fungus Sporothrix schenckii. The clinical manifestations of sporotrichosis can vary depending on the form of the infection and the host’s immune status. There are several forms of sporotrichosis, including cutaneous or lymphocutaneous, fixed cutaneous, and disseminated forms. Here are the main clinical manifestations associated with each form:
- Cutaneous or Lymphocutaneous Sporotrichosis:
- Most common form of sporotrichosis.
- Begins as a small, painless bump or nodule at the site of inoculation (typically on the skin).
- The initial bump can slowly develop into an ulcer or an open sore, which may be accompanied by redness, swelling, and tenderness.
- Lesions can be localized or multiple, forming a linear or nodular pattern along the lymphatic vessels, known as “sporotrichoid spread.”
- Lymph nodes near the affected area may become enlarged and tender.
- Lesions usually occur on exposed areas of the body, such as the hands, arms, or legs, where inoculation has taken place.
- Fixed Cutaneous Sporotrichosis:
- Presents as a persistent, localized, non-healing skin lesion.
- The lesion is typically a plaque or an ulcer that remains confined to the initial site of inoculation.
- Unlike lymphocutaneous sporotrichosis, there is no evident spread along lymphatic vessels.
- Disseminated Sporotrichosis:
- A less common and more severe form of sporotrichosis, typically seen in individuals with compromised immune systems.
- The infection spreads beyond the initial site of inoculation to other organs and tissues.
- Can involve the lungs, bones, joints, central nervous system, and other internal organs.
- Disseminated sporotrichosis may present with systemic symptoms such as fever, weight loss, fatigue, and generalized illness.
- Pulmonary sporotrichosis: This is an extremely uncommon form of sporotrichosis that affects the airways. It may result in coughing, shortness of breath, and chest discomfort.
- Osteoarticular sporotrichosis: This is an uncommon variant of sporotrichosis that affects the bones and joints. It can cause joint pain and inflammation.
- Meningeal sporotrichosis: Meningeal sporotrichosis is a rare form of sporotrichosis that effects the membranes surrounding the brain and spinal cord (meninges). It can result in headache, fever, and cervical stiffness.
Diagnosis of Sporotrichosis
Sporothrix schenckii-caused sporotrichosis is diagnosed using a combination of clinical evaluation, laboratory investigations, and occasionally imaging studies. The following are the primary diagnostic techniques for sporotrichosis:
- Clinical Evaluation: The healthcare professional will evaluate the patient’s medical history and conduct a physical examination. Along the lymphatic vessels, they will search for indications and symptoms of sporotrichosis, such as skin lesions, nodules, and ulcers. However, clinical evaluation alone cannot provide a definitive diagnosis.
- Microscopic Examination: Direct microscopic examination of clinical samples enables the visualisation of fungal components. The hyphae or yeast cells in skin scrapings, tissue biopsies, or fluid samples obtained from lesions can be identified using a potassium hydroxide (KOH) solution or calcofluor white stain. However, the sensitivity of this technique may be limited.
- Cultures of Fungi: Cultures of fungi are regarded as the gold standard for diagnosing sporotrichosis. The clinical sample (such as a skin biopsy, tissue specimen, or fluid) is cultured on fungal media, such as Sabouraud dextrose agar. Sporothrix schenckii grows slowly and visible colonies may take several weeks to form. Colony morphology, microscopic examination of fungal structures, and additional tests, such as molecular techniques or physiological testing, can confirm the fungus’ identification.
- Molecular Tests: Sporothrix schenckii can be directly detected and identified in clinical samples using polymerase chain reaction (PCR) assays. In instances where fungal cultures may be negative or delayed, PCR can provide a rapid and sensitive diagnosis. It can also distinguish between species of Sporothrix and aid in species identification.
- Imaging Studies: Imaging studies, such as X-rays, ultrasound, and computed tomography (CT) scans, may be performed in certain instances. In cases of disseminated sporotrichosis, where the fungus may infect internal tissues, bones, or organs, these studies can aid in determining the extent of the infection.
Treatment of Sporotrichosis
The treatment of sporotrichosis, a fungal infection caused by Sporothrix schenckii, typically involves antifungal medications. The choice of treatment depends on the form and severity of the infection. Here are the main treatment options for sporotrichosis:
- Cutaneous or Lymphocutaneous Sporotrichosis:
- Mild to moderate cases: Itraconazole is the preferred treatment. The standard dosage is 200-400 mg per day for 3-6 months or until the lesions have completely resolved. The duration of treatment may vary depending on the response to therapy.
- Severe or disseminated cases: Amphotericin B may be considered in severe or disseminated infections. It is administered intravenously under close medical supervision.
- Fixed Cutaneous Sporotrichosis:
- Itraconazole is the treatment of choice, with a standard dosage of 200-400 mg per day for 3-6 months. In some cases, shorter treatment durations may be effective.
- Disseminated Sporotrichosis:
- Disseminated sporotrichosis requires aggressive and prolonged treatment. Amphotericin B is the initial treatment of choice, followed by oral itraconazole for a prolonged period (up to 12 months or longer).
In addition to antifungal therapy, the following general measures may be recommended:
- Wound care: Good wound hygiene and proper wound care, including keeping the affected area clean and dry, may help prevent secondary bacterial infections.
- Supportive measures: Symptomatic treatment for pain, swelling, and inflammation may be prescribed, such as nonsteroidal anti-inflammatory drugs (NSAIDs).
- Monitoring and follow-up: Regular monitoring of the patient’s response to treatment and clinical progress is essential. Follow-up visits and tests may be scheduled to assess treatment efficacy.
Prevention and Control of Sporotrichosis
Prevention and control measures for sporotrichosis, a fungal infection caused by Sporothrix schenckii, primarily focus on reducing exposure to the fungus and promoting good hygiene practices. Here are some preventive measures that can be followed:
- Personal Protective Measures:
- When working with soil, plants, or other potential sources of Sporothrix schenckii, it is recommended to wear gloves, long sleeves, and other protective garments in order to minimise direct contact with the fungus.
- Those at a higher risk of exposure, such as gardeners, farmers, and landscapers, should be informed of the potential dangers and preventative measures.
- Avoiding Traumatic Inoculation:
- Avoid puncture wounds, scrapes, and scratches that can serve as entry points for the fungus by taking precautions. For instance, when handling sharp objects or working in environments with potential sources of Sporothrix schenckii, one should don protective gloves and clothing.
- Hygiene Practices:
- To reduce the risk of infection, thoroughly cleanse and clean any cuts, wounds, or skin abrasions with soap and water.
- Maintain good general hygiene by regularly washing your hands with soap and water, particularly after gardening or handling soil.
- Animal Handling:
- Take steps to reduce the risk of zoonotic transmission if you have pets, particularly cats. This includes avoiding direct contact with skin lesions or secretions of infected animals and immediately seeking veterinary care if canines exhibit sporotrichosis symptoms.
- Environmental Control:
- Sporothrix schenckii is commonly found in soil, decomposing plant matter, and plant matter. Wear appropriate footwear, clean and disinfect gardening implements, and avoid contact with soil or plant debris if you have open wounds.
FAQ
What is Sporothrix schenckii?
Sporothrix schenckii is a dimorphic fungus that causes sporotrichosis, a fungal infection that primarily affects the skin and lymphatic system.
How is Sporothrix schenckii transmitted?
Sporothrix schenckii is typically transmitted through traumatic inoculation, such as cuts or puncture wounds, when the fungus comes into contact with the skin or subcutaneous tissues.
What are the symptoms of sporotrichosis?
The symptoms of sporotrichosis can vary depending on the form of the infection. Common symptoms include skin lesions, nodules, ulcers, and the characteristic sporotrichoid spread along the lymphatic vessels.
Is sporotrichosis contagious?
Sporotrichosis is not highly contagious and does not spread easily from person to person. It is primarily acquired through environmental exposure to the fungus.
How is sporotrichosis diagnosed?
Diagnosis of sporotrichosis involves a combination of clinical evaluation, microscopic examination of clinical samples, fungal culture, and sometimes molecular tests. Imaging studies may also be used to evaluate the extent of the infection.
What is the treatment for sporotrichosis?
The treatment of sporotrichosis typically involves antifungal medications, such as itraconazole or amphotericin B, depending on the form and severity of the infection. Treatment duration can range from several weeks to months.
Can sporotrichosis be prevented?
Prevention of sporotrichosis involves personal protective measures, such as wearing gloves and protective clothing when working in environments with potential sources of Sporothrix schenckii. Good hygiene practices and avoiding traumatic inoculation are also important preventive measures.
Can animals transmit sporotrichosis to humans?
Yes, animals, particularly cats, can transmit sporotrichosis to humans. Direct contact with skin lesions or secretions of infected animals should be avoided, and veterinary care should be sought if pets show signs of sporotrichosis.
Are there any complications associated with sporotrichosis?
Sporotrichosis can lead to complications, especially in severe or disseminated cases. It can involve deeper tissues, bones, joints, and internal organs. Prompt diagnosis and appropriate treatment can help minimize complications.
Is sporotrichosis a common infection?
Sporotrichosis is considered a relatively rare infection. It is more commonly seen in certain geographical areas with specific environmental conditions, such as tropical and subtropical regions, as well as in individuals with occupational or recreational exposure to the fungus.
References
- Kauffman CA. Sporotrichosis. Clin Infect Dis. 1999;29(2):231-236.
- Marimon R, Cano J, Gené J, Sutton DA, Kawasaki M, Guarro J. Sporothrix brasiliensis, S. globosa, and S. mexicana, three new Sporothrix species of clinical interest. J Clin Microbiol. 2007;45(10):3198-3206.
- Barros MB, Schubach Ade O, do Valle AC, et al. Cat-transmitted sporotrichosis epidemic in Rio de Janeiro, Brazil: description of a series of cases. Clin Infect Dis. 2004;38(4):529-535.
- Mahajan VK, Sharma NL, Sharma RC, Gupta ML. Cutaneous sporotrichosis in Himachal Pradesh, India. Mycoses. 2005;48(2):123-128.
- Almeida-Paes R, de Oliveira MM, Freitas DF, do Valle AC, Zancopé-Oliveira RM, Gutierrez-Galhardo MC. Sporotrichosis in Rio de Janeiro, Brazil: Sporothrix brasiliensis is associated with atypical clinical presentations. PLoS Negl Trop Dis. 2014;8(8):e3094.
- Bonifaz A, Vázquez-González D, Tirado-Sánchez A, Paredes-Solis V, Araiza J, Hernández MA. Sporotrichosis caused by Sporothrix mexicana, an endemic species coexisting with Sporothrix schenckii in the tropical areas of Mexico. Rev Inst Med Trop Sao Paulo. 2012;54(5):273-277.
