Table of Contents
What is Human Respiratory System?
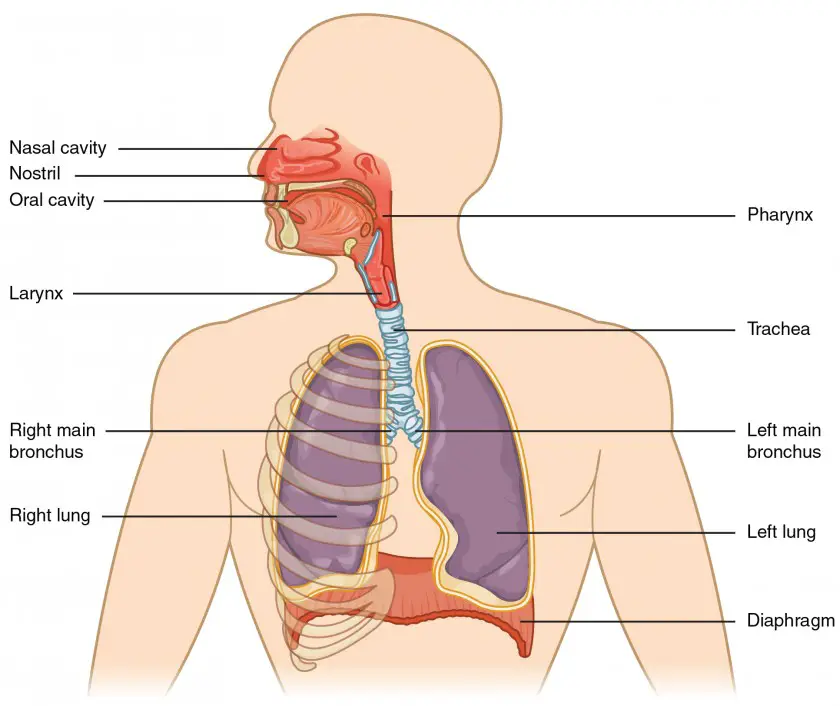
The human respiratory system is a complex network of organs and tissues responsible for the process of respiration, which involves the intake of oxygen and the removal of carbon dioxide from the body. It allows for the exchange of gases between the external environment and the bloodstream.
The major components of the human respiratory system include:
- Nasal Cavity: The process of respiration begins in the nasal cavity. The air enters the body through the nostrils and passes through the nasal cavity, where it is filtered, humidified, and warmed before reaching the rest of the respiratory system.
- Pharynx: The pharynx, or throat, is a muscular tube located at the back of the nasal cavity. It serves as a common pathway for both the respiratory and digestive systems.
- Larynx: The larynx, commonly known as the voice box, is situated below the pharynx. It contains the vocal cords, which vibrate to produce sound when air passes through them.
- Trachea: The trachea, also called the windpipe, is a tube that connects the larynx to the bronchi. It is lined with cilia and mucus-producing cells that help to trap foreign particles and protect the respiratory system.
- Bronchi: The trachea branches into two bronchi, with each bronchus leading to a lung. Inside the lungs, the bronchi divide further into smaller tubes called bronchioles.
- Lungs: The lungs are the main organs of respiration and are located in the chest cavity. The right lung has three lobes, while the left lung has two lobes. They are composed of millions of tiny air sacs called alveoli, where the exchange of oxygen and carbon dioxide takes place.
- Diaphragm: The diaphragm is a dome-shaped muscle located at the base of the chest cavity. It plays a crucial role in respiration by contracting and flattening during inhalation, allowing the lungs to expand and draw in air.
During the process of respiration, inhalation and exhalation occur. Inhalation involves the contraction of the diaphragm and other respiratory muscles, which expands the chest cavity and causes air to enter the lungs. Oxygen from the inhaled air is then transferred to the bloodstream through the walls of the alveoli. In contrast, during exhalation, the diaphragm and respiratory muscles relax, reducing the size of the chest cavity and causing carbon dioxide to be expelled from the lungs.
The human respiratory system is essential for the exchange of gases, ensuring the delivery of oxygen to cells throughout the body and the removal of waste carbon dioxide. It works in coordination with the circulatory system to support overall bodily functions.
Definition of Respiratory System
The respiratory system is the collection of organs and tissues in the human body responsible for breathing, gas exchange, and oxygen supply. It includes structures such as the nose, throat, lungs, and diaphragm, working together to facilitate the intake of oxygen and removal of carbon dioxide.
Anatomy of the Respiratory System
The respiratory system’s organs include the nose, throat, larynx, trachea, bronchi and their smaller branches, and the lungs, which contain the alveoli.
1. The Nose
The nose is an important component of the respiratory system. Here is a description of the nose based on the provided information:
The nose serves as the only externally visible part of the respiratory system. It consists of various structures that facilitate the intake of air and perform important functions. Here are the key features of the nose:
- Nostrils (Nares): Air enters the nose through the nostrils, also known as nares. These are the openings through which air passes during breathing.
- Nasal Cavity: The interior of the nose comprises the nasal cavity, which is divided by a midline nasal septum. It is a hollow space lined with specialized tissues.
- Olfactory Receptors: The superior part of the nasal cavity contains slit-like structures where olfactory receptors for the sense of smell are located. These receptors, housed in the mucosa just beneath the ethmoid bone, are responsible for detecting various scents.
- Respiratory Mucosa: The remaining mucosal lining of the nasal cavity, known as respiratory mucosa, rests on a network of thin-walled veins. This vascular network warms the air as it passes through the nasal cavity.
- Mucus: The mucosa’s glands produce a sticky mucus that serves multiple purposes. It moisturizes the air, capturing incoming bacteria and other foreign debris. Enzymes like lysozyme in the mucus help chemically destroy bacteria.
- Ciliated Cells: The nasal mucosa contains ciliated cells, which create a gentle current that moves the layer of contaminated mucus towards the throat. From there, it is swallowed and digested by stomach juices.
- Conchae: The lateral walls of the nasal cavity are uneven due to three mucosa-covered projections called conchae. These conchae increase the surface area of the nasal mucosa exposed to the air and promote air turbulence within the nasal cavity.
- Palate: The nasal cavity is separated from the oral cavity by a partition called the palate. The front part, supported by bone, is known as the hard palate, while the back part without bony support is called the soft palate.
- Paranasal Sinuses: Surrounding the nasal cavity, there is a ring of paranasal sinuses located in the frontal, sphenoid, ethmoid, and maxillary bones. These sinuses serve to lighten the skull and act as resonance chambers for speech.
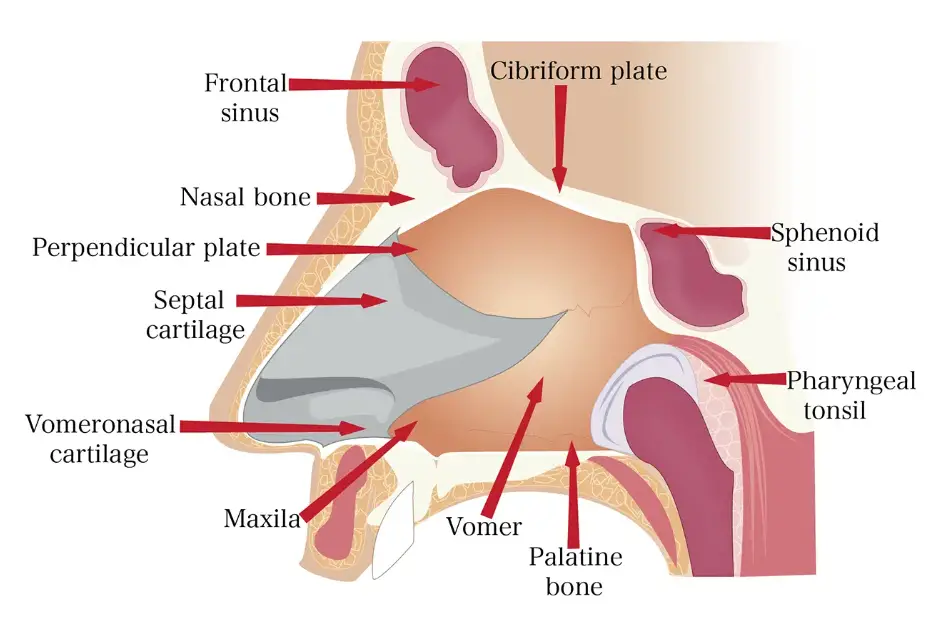
The nose plays a crucial role in the respiratory system by allowing the inhalation of air through the nostrils, filtering and humidifying it, detecting odors through olfactory receptors, and promoting the movement of mucus to protect the respiratory tract. Additionally, the nasal cavity is associated with paranasal sinuses that contribute to the overall function and structure of the head.
2. Pharynx
The pharynx is an important structure within the respiratory system. Here is a description of the pharynx based on the provided information:
The pharynx is a muscular passageway approximately 13 cm (5 inches) in length. It can be visualized as resembling a short length of red garden hose. The pharynx, commonly referred to as the throat, serves as a shared pathway for both food and air.
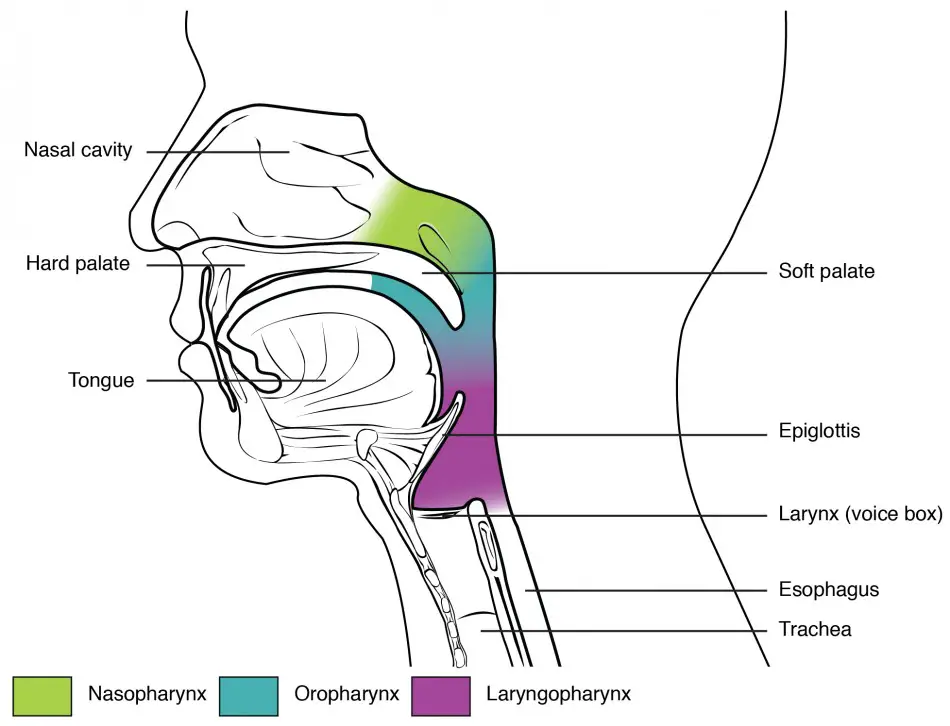
The pharynx is divided into several portions:
- Nasopharynx: The superior portion of the pharynx is called the nasopharynx. It is the region where air enters from the nasal cavity. The nasopharynx then serves as a passage for air as it descends towards the oropharynx and laryngopharynx.
- Oropharynx: Situated below the nasopharynx, the oropharynx is involved in both air and food passage. It serves as a common pathway for air from the nasopharynx and for food from the mouth. The palatine tonsils, found at the end of the soft palate, are located within the oropharynx.
- Laryngopharynx: The laryngopharynx is the lowest part of the pharynx. It connects the oropharynx to the larynx, which is situated below it. The laryngopharynx serves as a passage for both air and food, with air entering the larynx and food continuing down the esophagus.
Additionally, there are specific structures associated with the pharynx:
- Pharyngotympanic Tubes: The pharyngotympanic tubes, also known as Eustachian tubes, connect the middle ear to the nasopharynx. These tubes are responsible for equalizing pressure in the middle ear and draining fluids.
- Pharyngeal Tonsil: The pharyngeal tonsil, commonly referred to as the adenoid, is located in the high region of the nasopharynx. It is a mass of lymphoid tissue that plays a role in the immune system’s defense against infections.
- Palatine Tonsils: The palatine tonsils are found in the oropharynx, situated at the end of the soft palate. They are also a part of the immune system and help in defending against pathogens entering the body through the mouth and throat.
- Lingual Tonsils: The lingual tonsils are located at the base of the tongue. They are composed of lymphoid tissue and contribute to the immune response in the oral cavity and throat.
The pharynx serves as a vital passageway for air and food, facilitating their movement through the respiratory and digestive systems, respectively. It also houses various tonsils that play a role in the immune response, helping to protect the body against infections and pathogens.
3. Larynx
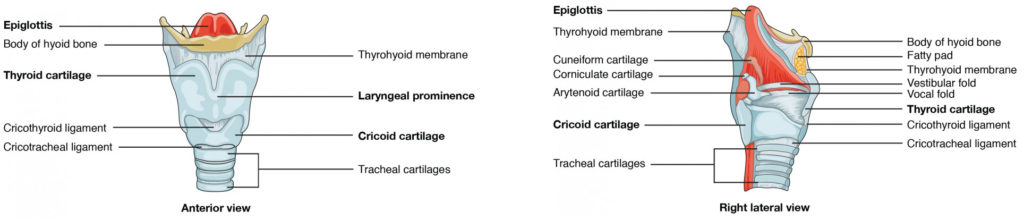
- The larynx, also known as the voice box, is a crucial structure in the respiratory system that plays multiple roles in the routing of air and food and the production of speech. Here is a description of the larynx based on the provided information:
- The larynx is located below the pharynx and connects the pharynx to the trachea. It is composed of several cartilages, including the thyroid cartilage, epiglottis, and cricoid cartilage. The thyroid cartilage, commonly known as the Adam’s apple, is the largest of the hyaline cartilages and protrudes anteriorly. The epiglottis, often referred to as the “guardian of the airways,” is a spoon-shaped flap of elastic cartilage that protects the superior opening of the larynx.
- One of the essential features of the larynx is the vocal folds, also known as true vocal cords. These are formed by a pair of mucous membrane folds within the larynx. The vocal folds vibrate when air passes through them, enabling us to produce speech and various vocal sounds. The space between the vocal folds is called the glottis, which is a slit-like passageway.
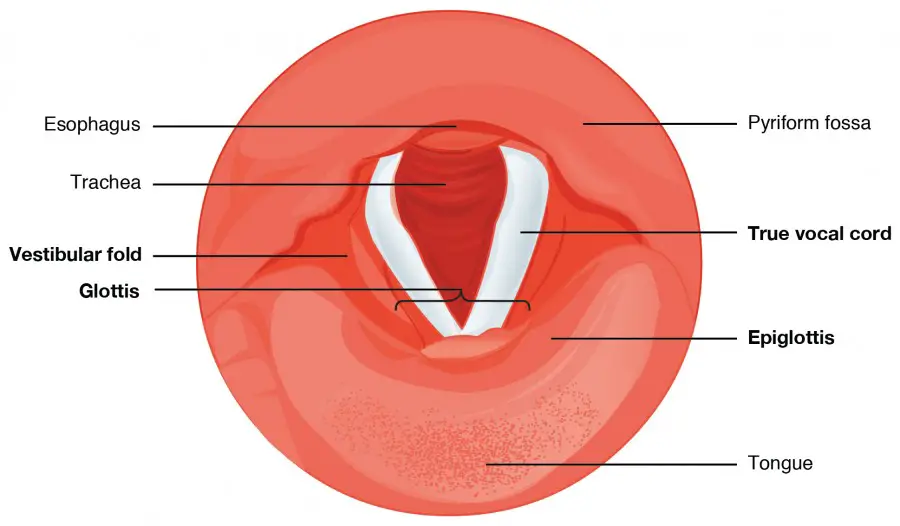
- Additionally, there are smaller cartilages in the larynx, including the arytenoids, corniculates, and cuneiforms, which attach to the epiglottis and the muscles responsible for moving the vocal cords during speech production.
- The larynx has important functions in respiration and swallowing. During swallowing, the pharynx and larynx elevate, allowing the pharynx to expand and the epiglottis to swing downward, effectively closing the opening to the trachea. This action prevents food and beverages from entering the trachea and directs them toward the esophagus.
- The lining of the superior portion of the larynx, continuous with the laryngopharynx, is lined with stratified squamous epithelium, which transitions into pseudostratified ciliated columnar epithelium containing goblet cells. This specialized epithelium produces mucus that helps trap debris and pathogens as they enter the trachea. The cilia present in the epithelium beat in an upward motion, moving the mucus toward the laryngopharynx, where it can be swallowed and transported down the esophagus.
- In summary, the larynx serves as a crucial structure for routing air and food in the respiratory system. It houses the vocal folds that allow for speech production and contains the epiglottis, which protects the airways during swallowing. The specialized epithelium lining the larynx helps to filter and remove debris, ensuring the smooth passage of air into the trachea.
4. Trachea
- The trachea, also known as the windpipe, is a vital part of the respiratory system. It serves as a passage for air to travel from the larynx to the lungs. The trachea has a length of approximately 10 to 12 cm (about 4 inches) and extends to the level of the fifth thoracic vertebra, which is located in the middle of the chest.
- One of the notable features of the trachea is its structural composition. The walls of the trachea are reinforced with C-shaped rings made of hyaline cartilage. These rings provide rigidity to the trachea, ensuring that it remains open and patent even during pressure changes that occur during breathing. The open parts of the C-shaped rings allow the adjacent esophagus to expand forward when we swallow large pieces of food. This arrangement helps prevent any obstruction in the airway.
- The trachea is lined with a specialized type of epithelium called pseudostratified ciliated columnar epithelium. This lining contains tiny hair-like structures called cilia. The cilia continuously beat in a coordinated manner, moving in a direction opposite to that of the incoming air. This motion helps propel mucus, which is secreted by goblet cells in the epithelium, along with dust particles and other debris away from the lungs. The mucus is transported towards the throat, where it can be either swallowed or expelled through coughing.
- The trachea is supported by the fibroelastic membrane, which is formed by the trachealis muscle and elastic connective tissue. This membrane lies on the posterior surface of the trachea and connects the C-shaped cartilages. The fibroelastic membrane allows the trachea to stretch and expand slightly during inhalation and exhalation, contributing to its flexibility. The cartilaginous rings provide structural support, preventing the trachea from collapsing and maintaining its open shape.
- Posteriorly, the trachea is bordered by the esophagus, the tube that carries food from the throat to the stomach. These structures are closely situated but separated by dense connective tissue.
- Overall, the trachea plays a crucial role in facilitating the flow of air into the lungs. Its rigid structure, supported by C-shaped cartilages, along with the coordinated movement of cilia and mucus production, helps to protect the respiratory system from the entry of harmful substances and ensures efficient gas exchange.
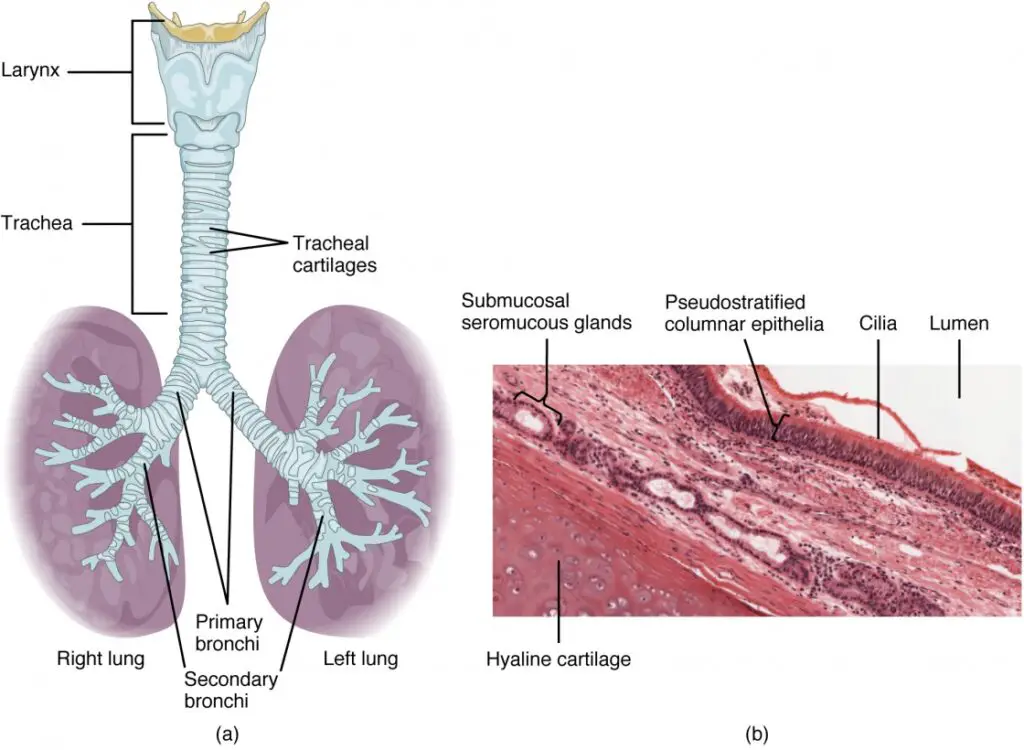
5. Main Bronchi
- The main bronchi, also known as primary bronchi, are the largest airway passages that branch off from the trachea. They are formed by the division of the trachea into two separate tubes. One main bronchus leads to the right lung, while the other leads to the left lung.
- In terms of their location, each main bronchus takes an oblique course before entering the medial depression of the lung on its respective side. This means that they run diagonally downward before descending into the lung tissue.
- When it comes to size, there is a noticeable difference between the right and left main bronchi. The right main bronchus is wider, shorter, and straighter compared to its counterpart on the left side. This structural difference can be attributed to the fact that the right lung has three lobes, while the left lung has only two. The right main bronchus needs to accommodate the larger right lung, hence its wider diameter and straighter path.
- The main bronchi serve as major conduits for air to enter and exit the lungs. They further divide into smaller bronchial branches known as secondary bronchi, which then divide into even smaller tertiary bronchi, bronchioles, and ultimately, the smallest airways called alveoli. The branching network of bronchi and bronchioles within the lungs allows for efficient distribution of air and facilitates the process of gas exchange between the respiratory system and the bloodstream.
- Overall, the main bronchi play a vital role in respiratory function, serving as the initial pathways for air to reach the lungs. Their structure, location, and size are adapted to accommodate the unique characteristics of each lung and contribute to the efficient exchange of oxygen and carbon dioxide during respiration.
6. Lungs
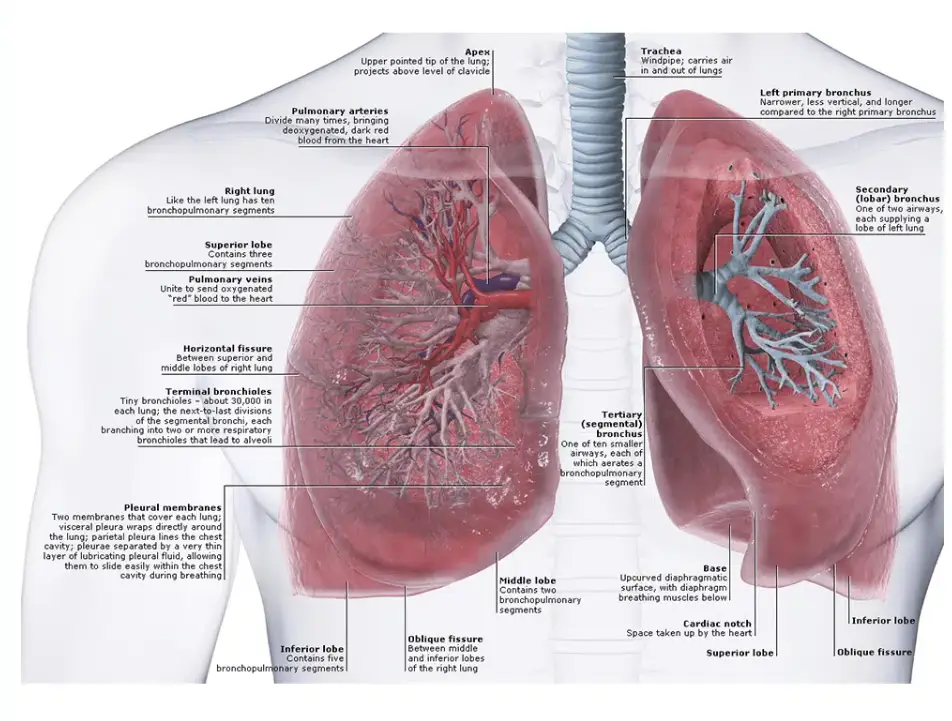
- The lungs are vital organs of the respiratory system that occupy the majority of the thoracic cavity, except for the central area known as the mediastinum. The mediastinum houses various organs, including the heart, great blood vessels, bronchi, esophagus, and others, while the lungs extend on either side.
- Each lung has specific anatomical features. The superior portion of each lung, called the apex, is located just beneath the clavicle. On the other hand, the base of the lungs is a broad area that rests on the diaphragm, the primary muscle involved in respiration.
- The lungs are divided into lobes by fissures. The left lung has two lobes, while the right lung has three. These lobes help to compartmentalize the lung tissue and contribute to efficient respiratory function.
- The surface of each lung is covered by a serous membrane called the visceral pleura, or pulmonary pleura. This membrane is in close contact with the lung tissue. The walls of the thoracic cavity are lined by another layer of pleura known as the parietal pleura. The pleural membranes secrete a slippery serous fluid called pleural fluid, which allows the lungs to glide smoothly over the thoracic wall during breathing movements and helps the two pleural layers to adhere to each other.
- The lungs are tightly held against the thoracic wall, and the pleural space, where the pleural fluid resides, is more of a potential space than an actual one.
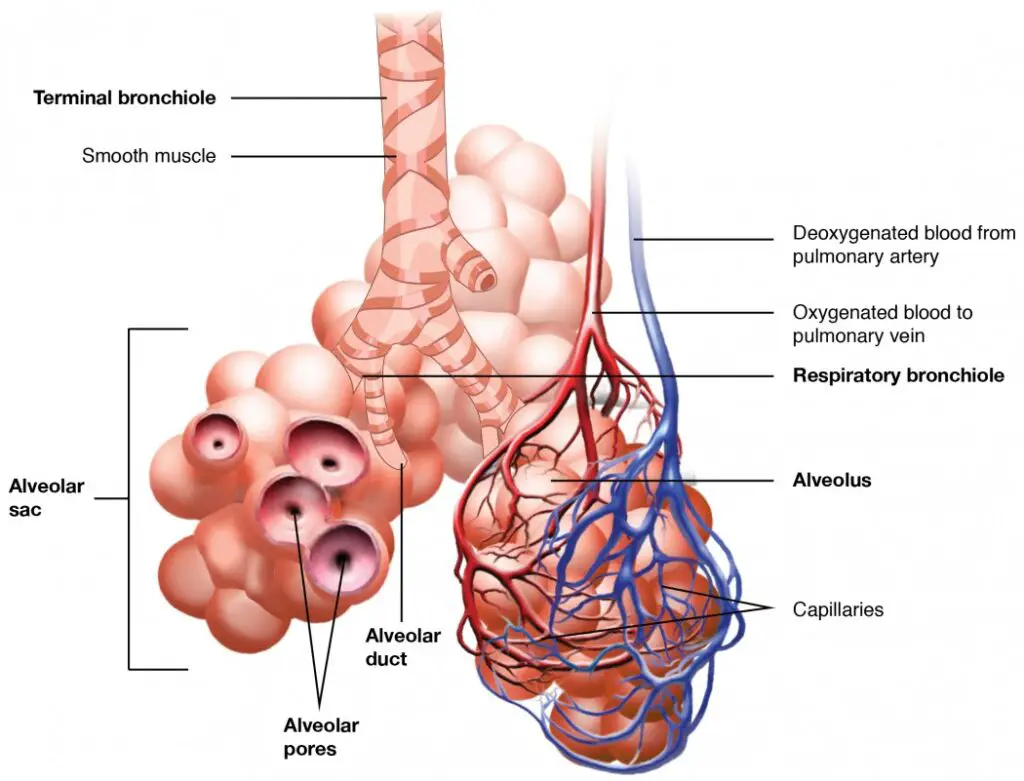
- The conducting passageways of the respiratory system include bronchioles, which are the smallest of these structures. They further lead to the respiratory zone, where gas exchange occurs. The respiratory zone includes respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli, which are tiny air sacs responsible for gas exchange between the respiratory system and the bloodstream.
- All other respiratory passages, apart from the respiratory zone structures, are considered conducting zone structures. They serve as conduits to facilitate the movement of air to and from the respiratory zone.
- The lung tissue primarily consists of elastic connective tissue, known as the stroma. This elastic tissue allows the lungs to passively recoil during exhalation, aiding in the expulsion of air.
- In summary, the lungs are situated in the thoracic cavity, with specific regions such as the apex and base. They are divided into lobes and are covered by pleural membranes that produce pleural fluid. The lungs consist of conducting and respiratory zone structures, with the latter being responsible for gas exchange. The elastic connective tissue in the lung tissue enables passive recoil during exhalation. The lungs are essential for the exchange of oxygen and carbon dioxide, playing a crucial role in respiration.
7. The Respiratory Membrane
- The respiratory membrane is a specialized structure involved in the process of gas exchange within the lungs. It is formed by the combined components of the alveolar and capillary walls.
- The walls of the alveoli, the tiny air sacs within the lungs, are primarily composed of a single layer of thin squamous epithelial cells. This thinness is essential for efficient gas exchange, as it allows for a shorter diffusion distance for oxygen and carbon dioxide between the alveoli and the bloodstream.
- The respiratory membrane also contains alveolar pores, which serve as connections between neighboring air sacs. These pores provide alternative routes for air to reach the alveoli when the feeder bronchioles are obstructed by mucus or other blockages.
- The respiratory membrane itself is formed by the fusion of the alveolar and capillary walls, along with their associated basement membranes and occasional elastic fibers. This structure creates the air-blood barrier. On one side of the respiratory membrane, there is the flow of gas (air) within the alveoli, while on the other side, there is the flow of blood within the capillaries. This arrangement facilitates the diffusion of oxygen from the alveoli into the bloodstream and the transfer of carbon dioxide from the bloodstream into the alveoli for elimination.
- Within the alveoli, there are specialized cells called alveolar macrophages, sometimes referred to as “dust cells.” These macrophages play a crucial role in the immune defense of the lungs. They are highly efficient in capturing and removing bacteria, carbon particles, and other debris that may have entered the respiratory system.
- Scattered among the epithelial cells that make up the majority of the alveolar walls are cuboidal cells. These chunky cuboidal cells produce a lipid molecule called surfactant. Surfactant is important for lung function as it coats the gas-exposed surfaces of the alveoli. It helps reduce surface tension within the alveoli, preventing them from collapsing during exhalation and promoting the ease of lung expansion during inhalation.
- In summary, the respiratory membrane is the site of gas exchange in the lungs. It is composed of the thin epithelial cells lining the alveoli, along with the associated capillary walls, fused basement membranes, and occasional elastic fibers. Alveolar pores provide alternative pathways for airflow, while alveolar macrophages help clear debris. The production of surfactant by cuboidal cells is essential for maintaining proper lung function.
Physiology of the Respiratory System
The respiratory system’s primary duty is to give oxygen to the body and to expel carbon dioxide. To accomplish this, at least four different activities known collectively as respiration must occur.
Respiration
- Respiration is the overall process by which the body obtains oxygen from the environment and removes carbon dioxide. It involves several interconnected steps to ensure the exchange of gases between the external environment and the body’s tissues.
- Pulmonary ventilation, commonly referred to as breathing, is the first step in respiration. It involves the movement of air into and out of the lungs. Inhalation, or inspiration, occurs when the diaphragm contracts and the chest cavity expands, creating a pressure gradient that allows air to enter the lungs. Exhalation, or expiration, takes place when the diaphragm relaxes and the chest cavity decreases in size, causing air to be expelled from the lungs. Pulmonary ventilation is essential for continuously refreshing the gases in the air sacs, ensuring a constant supply of oxygen and removal of carbon dioxide.
- External respiration occurs in the lungs at the site of the alveoli. It is the process of gas exchange between the pulmonary blood and the air within the alveoli. Oxygen diffuses from the alveoli into the blood, while carbon dioxide moves in the opposite direction, from the blood into the alveoli. This exchange is driven by differences in partial pressures of oxygen and carbon dioxide between the air and the blood.
- Respiratory gas transport involves the transportation of oxygen and carbon dioxide to and from the lungs and the body’s tissues. Oxygen is primarily carried by red blood cells, which bind to oxygen molecules and transport them throughout the body via the bloodstream. Carbon dioxide, produced as a waste product of cellular metabolism, is also transported in the blood, primarily in the form of bicarbonate ions. The cardiovascular system plays a crucial role in facilitating the transport of respiratory gases to and from the lungs and tissues.
- Internal respiration occurs at the systemic capillaries, where gas exchange takes place between the blood and the body’s tissues. Oxygen diffuses from the blood into the cells, while carbon dioxide moves from the cells into the bloodstream. This exchange ensures that oxygen is delivered to the tissues for cellular respiration, where it is used to produce energy, while carbon dioxide, a waste product, is removed.
- In summary, respiration involves the processes of pulmonary ventilation, external respiration, respiratory gas transport, and internal respiration. Together, these processes ensure the continuous exchange of oxygen and carbon dioxide between the external environment, the lungs, the bloodstream, and the body’s tissues, supporting cellular metabolism and overall bodily function.
Mechanics of Breathing
- The mechanics of breathing involve the processes of inspiration (inhaling) and expiration (exhaling), which rely on volume changes in the thoracic cavity to create pressure changes that allow for the flow of gases.
- The fundamental rule is that volume changes lead to pressure changes, which, in turn, result in the flow of gases to equalize pressure. During inspiration, air flows into the lungs. This occurs when the chest expands laterally, the rib cage is elevated, and the diaphragm contracts and moves downward, becoming flattened. As a result, the lungs are stretched to a larger thoracic volume, causing the intrapulmonary pressure (pressure within the lungs) to decrease. The decrease in pressure allows air to flow into the lungs, filling the expanded space.
- On the other hand, expiration is the process of air leaving the lungs. During expiration, the chest is depressed, reducing the lateral dimension. The rib cage descends, and the diaphragm relaxes and moves upward, assuming a dome-shaped position. The elastic recoil of the lungs causes them to return to a smaller volume. This reduction in volume leads to an increase in intrapulmonary pressure, forcing air to flow out of the lungs.
- The intrapulmonary volume refers to the volume within the lungs. It changes during the breathing process as the lungs expand and contract.
- An essential factor in the mechanics of breathing is the intrapleural pressure, which is the pressure within the pleural space surrounding the lungs. The intrapleural pressure is always negative compared to atmospheric pressure. This negative pressure is crucial in preventing the collapse of the lungs. It is created by the opposing forces of the elastic recoil of the lungs, which tends to collapse them, and the surface tension of the pleural fluid, which adheres the lungs to the thoracic wall. The negative intrapleural pressure keeps the lungs expanded and maintains their contact with the thoracic cavity.
- In addition to normal breathing, there are nonrespiratory air movements that can occur. These movements are typically a result of reflex activity but can also be produced voluntarily. Examples of nonrespiratory air movements include coughing, sneezing, crying, laughing, hiccups, and yawning. These movements serve specific purposes, such as clearing the airways or expressing emotions.
- In summary, the mechanics of breathing involve volume changes leading to pressure changes, which drive the flow of gases. Inspiration occurs when the chest expands and the diaphragm contracts, creating a decrease in intrapulmonary pressure and allowing air to enter the lungs. Expiration happens when the chest contracts and the diaphragm relaxes, causing an increase in intrapulmonary pressure and pushing air out of the lungs. The negative intrapleural pressure prevents lung collapse. Nonrespiratory air movements are additional actions that can occur alongside normal breathing and serve specific functions.
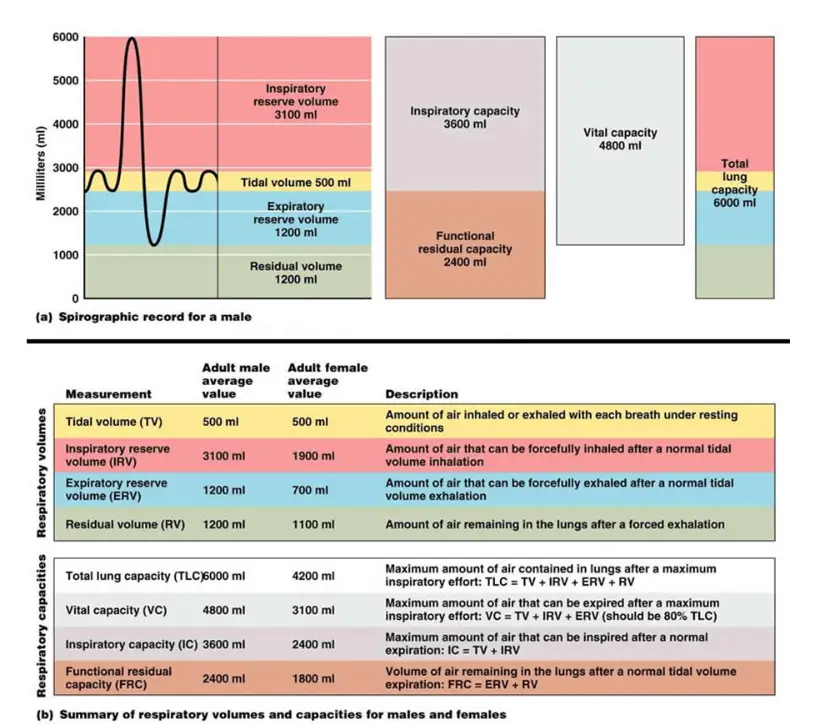
Respiratory Volumes and Capacities
- Respiratory volumes and capacities are important measurements that help assess lung function and efficiency. Here are some key terms related to respiratory volumes and capacities:
- Tidal volume refers to the amount of air that moves in and out of the lungs during normal quiet breathing. On average, approximately 500 ml of air is exchanged with each breath.
- Inspiratory reserve volume represents the additional amount of air that can be forcibly inhaled after a normal tidal volume inhalation. It ranges from 2100 ml to 3200 ml and reflects the maximum inhalation capacity.
- Expiratory reserve volume is the amount of air that can be forcibly exhaled after a normal tidal volume exhalation. It is approximately 1200 ml and demonstrates the maximum exhalation capacity.
- Residual volume is the volume of air that remains in the lungs even after a forceful exhalation. Around 1200 ml of air remains in the lungs at all times, contributing to gas exchange between breaths and helping to keep the alveoli inflated.
- Vital capacity is the total amount of air that can be exchanged during a maximal inhalation and exhalation. It is the sum of the tidal volume, inspiratory reserve volume, and expiratory reserve volume. In healthy young men, the typical vital capacity is around 4800 ml.
- Dead space volume refers to the portion of air that enters the respiratory tract but does not reach the alveoli for gas exchange. This air remains in the conducting zone passageways. During a normal tidal breath, the dead space volume is approximately 150 ml.
- Functional volume represents the portion of air that reaches the respiratory zone and actively participates in gas exchange. It is approximately 350 ml.
- To measure respiratory volumes and capacities, a device called a spirometer is used. A spirometer allows for the measurement of the volumes of air exhaled and inhaled by a person. As the individual breathes into the spirometer, the changes in air volume are recorded on an indicator, providing valuable information about lung function.
- In summary, respiratory volumes and capacities provide insights into the amount of air exchanged during breathing and lung function. They include tidal volume, inspiratory reserve volume, expiratory reserve volume, residual volume, vital capacity, dead space volume, and functional volume. These measurements help evaluate lung health and diagnose respiratory conditions. Spirometers are commonly used to assess respiratory volumes and capacities.
Respiratory Sounds
- Respiratory sounds provide valuable information about the condition and functioning of the respiratory system. Two distinct types of respiratory sounds are bronchial sounds and vesicular breathing sounds.
- Bronchial sounds are generated by the movement of air through the large respiratory passageways, namely the trachea and bronchi. These sounds are characterized by a relatively high pitch and intensity. They can be heard over the upper part of the chest, closer to the neck. Bronchial sounds are typically louder during expiration than inspiration.
- Vesicular breathing sounds, on the other hand, occur as air enters and fills the alveoli, which are the small air sacs in the lungs where gas exchange takes place. Vesicular sounds are softer, low-pitched, and resemble a gentle, muffled breeze. They are best heard over the peripheral lung fields, which are the lower parts of the chest closer to the base of the lungs. Vesicular sounds are more prominent during inspiration than expiration.
- These respiratory sounds provide important diagnostic clues to healthcare professionals. Abnormalities in the characteristics or patterns of these sounds can indicate various respiratory conditions. For instance, changes in the intensity or quality of bronchial sounds might suggest airway obstruction or consolidation of lung tissue, while alterations in vesicular sounds can indicate problems with lung ventilation or the presence of underlying lung diseases.
- By carefully listening to these respiratory sounds using a stethoscope, healthcare providers can gather valuable information about a patient’s respiratory health, diagnose respiratory disorders, and monitor treatment progress.
External Respiration, Gas Transport, and Internal Respiration
- The respiratory process involves external respiration, internal respiration, and the transport of gases within the body.
- External respiration, also known as pulmonary gas exchange, occurs in the lungs. During this process, oxygen is loaded into the bloodstream while carbon dioxide is unloaded from the blood. Oxygen moves from the alveoli in the lungs into the pulmonary capillaries, where it binds with hemoglobin molecules inside red blood cells (RBCs) to form oxyhemoglobin. Simultaneously, carbon dioxide, which has been produced as a waste product by the body’s cells, diffuses out of the blood into the alveoli to be exhaled.
- Internal respiration, or systemic capillary gas exchange, takes place in the body’s tissues. Here, oxygen is unloaded from the blood and delivered to the cells, while carbon dioxide is produced by cellular respiration and loaded into the bloodstream. Oxygen moves from the systemic capillaries into the surrounding tissues, diffusing across cell membranes to reach the mitochondria, where it is used in the production of energy. At the same time, carbon dioxide, produced as a byproduct of cellular metabolism, diffuses out of the cells into the systemic capillaries to be carried back to the lungs for elimination.
- The transport of gases within the bloodstream is crucial for their distribution throughout the body. Oxygen is primarily transported in two ways: the majority of it binds to hemoglobin molecules inside red blood cells, forming oxyhemoglobin, which accounts for the vast majority of oxygen transport. A smaller portion of oxygen is carried dissolved in the plasma. On the other hand, carbon dioxide is transported in plasma as bicarbonate ions, which result from the conversion of carbon dioxide to carbonic acid and further dissociation. Additionally, a smaller amount (around 20 to 30 percent) of carbon dioxide is carried inside red blood cells, bound to hemoglobin.
- These processes of external respiration, internal respiration, and gas transport ensure that oxygen is delivered to the body’s tissues and carbon dioxide is efficiently removed. The respiratory system plays a vital role in maintaining a balance of gases in the body and supporting cellular metabolism.
Control of Respiration
Control of Respiration refers to the various mechanisms and factors that regulate the rate and depth of breathing. It involves both neural and non-neural influences that ensure the body receives an adequate supply of oxygen and eliminates carbon dioxide.
Neural Regulation
- The phrenic and intercostal nerves play a crucial role in controlling the respiratory muscles, including the diaphragm and external intercostals. These nerves receive signals from neural centers located in the medulla and pons regions of the brain.
- The medulla and pons contain respiratory centers responsible for regulating the rhythm and depth of breathing. The medulla acts as a pacemaker, generating a self-exciting inspiratory center that sets the basic rhythm of breathing. Additionally, the medulla has an expiratory center that inhibits the pacemaker in a rhythmic manner. The pons centers help smooth out the breathing rhythm established by the medulla.
- Eupnea is the term used to describe the normal respiratory rate, which is typically maintained at a rate of 12 to 15 breaths per minute. Hyperpnea occurs during exercise when the brain centers send increased impulses to the respiratory muscles, resulting in more vigorous and deeper breathing.
Non-neural Factors Influencing Respiratory Rate and Depth
In addition to neural regulation, several non-neural factors can influence the rate and depth of breathing.
- Physical factors such as talking, coughing, and exercising can modify breathing patterns. For example, during exercise, the respiratory rate and depth increase to meet the increased oxygen demand. Similarly, an increased body temperature can stimulate an increase in breathing rate.
- Volition, or conscious control of breathing, is limited. The respiratory centers in the brain ignore signals from the cortex (our conscious desires) when oxygen supply in the blood is low or blood pH is falling, ensuring that the body’s vital needs take precedence.
- Emotional factors can also impact breathing. Emotional stimuli can initiate reflexes that act through centers in the hypothalamus, modifying the rate and depth of breathing accordingly.
- Chemical factors play a crucial role in regulating respiration. The levels of carbon dioxide (CO2) and oxygen (O2) in the blood are particularly important. Increased levels of CO2 and decreased blood pH stimulate an increase in the rate and depth of breathing. Conversely, low oxygen levels become significant stimuli when they reach dangerously low levels.
- Hyperventilation refers to rapid breathing that leads to the removal of excess CO2 and a decrease in carbonic acid levels. This process helps restore blood pH to a normal range when there is an accumulation of carbon dioxide or other acidic substances in the blood.
- On the other hand, hypoventilation involves slow or shallow breathing, allowing carbon dioxide to accumulate in the blood. This helps bring blood pH back into the normal range when the blood becomes slightly alkaline.
Overall, the control of respiration is a complex process involving neural centers in the medulla and pons, as well as various non-neural factors such as physical, volitional, emotional, and chemical influences. Together, these mechanisms ensure that breathing is appropriately regulated to maintain adequate oxygen levels and remove carbon dioxide from the body.
Functions of the Respiratory System
The respiratory system performs several vital functions in the human body. Here are the key functions of the respiratory system, based on the provided information:
- Oxygen Supplier: The respiratory system’s primary function is to ensure a continuous supply of oxygen to the body. It facilitates the inhalation of oxygen-rich air into the lungs, where it is transferred to the bloodstream for distribution to cells throughout the body.
- Elimination of Carbon Dioxide: Along with supplying oxygen, the respiratory system plays a crucial role in eliminating carbon dioxide, which is a waste product of cellular respiration. Carbon dioxide is carried from the body’s tissues to the lungs, where it is expelled during exhalation.
- Gas Exchange: The organs of the respiratory system oversee the exchange of gases between the bloodstream and the external environment. Oxygen from inhaled air diffuses into the bloodstream, while carbon dioxide moves from the bloodstream into the lungs to be exhaled.
- Passageway: The respiratory system provides passageways that allow air to reach the lungs. This includes the nasal cavity, pharynx, larynx, trachea, bronchi, and bronchioles, which form a network of air-conducting channels.
- Humidifier: The respiratory system helps to purify, humidify, and warm incoming air. As air passes through the nasal cavity, it is filtered to remove dust and other particles. The respiratory system also adds moisture and heat to the air, ensuring that it reaches the delicate tissues of the respiratory tract in an optimal condition.
In addition to these primary functions, the respiratory system has other roles:
- Creating Sounds: The respiratory system, particularly the structures of the upper respiratory tract, such as the larynx, plays a vital role in producing sounds used for speech and communication.
- Olfactory Senses: The nose and associated olfactory nerves within the respiratory system are involved in sensing smells. Animals, including humans, use their olfactory senses for various functions, such as digestion, hunting, recognition, and mating.
- Immunity: The respiratory system plays a role in the immune response by protecting the body against the invasion of pathogens. Epithelial cells in the respiratory tract secrete antibodies, enzymes, and peptides to fend off pathogens. The respiratory system’s coughing and sneezing mechanisms help remove bacteria and viruses trapped in mucus.
- Blood Clot Removal, Hormone Activation, and Regulation: Cells within the respiratory tract can assist in removing blood clots in pulmonary blood vessels. They can also activate hormones and modify substances circulating in the blood. Additionally, the respiratory system helps in making incoming air warm and moist to protect the delicate inner respiratory passages.
- Surfactant Production: Epithelial cells of the lungs produce surfactant, which aids in easier inhalation and exhalation. Adequate production of surfactant is crucial for the viability of pre-term births.
Overall, the respiratory system serves essential functions that contribute to oxygen supply, waste removal, gas exchange, immune defense, and other physiological processes in the human body.
FAQ
What is the respiratory system?
The respiratory system is a complex network of organs and tissues involved in the process of respiration, which includes the intake of oxygen and the removal of carbon dioxide from the body.
What are the main organs of the respiratory system?
The main organs of the respiratory system are the lungs, trachea (windpipe), bronchi, bronchioles, alveoli, and diaphragm.
How does air enter the respiratory system?
Air enters the respiratory system through the nose or mouth. It then passes through the pharynx, larynx, and trachea before reaching the bronchi and eventually the lungs.
What are the functions of the lungs?
The lungs are responsible for the exchange of oxygen and carbon dioxide. Oxygen is taken up by the bloodstream and transported to the body’s cells, while carbon dioxide, a waste product, is removed from the cells and expelled through exhalation.
What are alveoli and their role in respiration?
Alveoli are tiny air sacs located at the ends of the bronchioles in the lungs. They are surrounded by blood capillaries and are the primary site of gas exchange. Oxygen diffuses into the bloodstream from the alveoli, while carbon dioxide moves from the bloodstream into the alveoli to be exhaled.
How does the diaphragm contribute to breathing?
The diaphragm is a dome-shaped muscle located at the base of the chest cavity. During inhalation, the diaphragm contracts and moves downward, increasing the volume of the chest cavity and allowing air to enter the lungs. During exhalation, the diaphragm relaxes and moves upward, helping to expel air from the lungs.
What is the role of the bronchial tree in the respiratory system?
The bronchial tree refers to the branching network of bronchi and bronchioles in the lungs. It helps in the distribution of air to different regions of the lungs and ensures that air reaches the alveoli for efficient gas exchange.
How is the respiratory system controlled?
The respiratory system is primarily controlled by the medulla and pons in the brainstem. These neural centers regulate the rate and depth of breathing based on various factors such as oxygen and carbon dioxide levels, pH balance, physical activity, and emotional stimuli.
What is the role of mucus and cilia in the respiratory system?
Mucus, produced by goblet cells, helps to trap foreign particles, dust, and microorganisms in the respiratory tract, preventing them from reaching the lungs. Cilia, tiny hair-like structures lining the airways, move in coordinated waves to propel the trapped particles and mucus upward, where they can be coughed out or swallowed.
How does smoking affect the respiratory system?
Smoking damages the respiratory system in several ways. It irritates and inflames the airways, leading to chronic bronchitis and emphysema. Smoking also increases the risk of lung cancer and reduces lung function, making it harder to breathe. Additionally, it impairs the function of cilia and increases mucus production, further compromising the respiratory system’s defenses.
