Table of Contents
What is Autonomic nervous system?
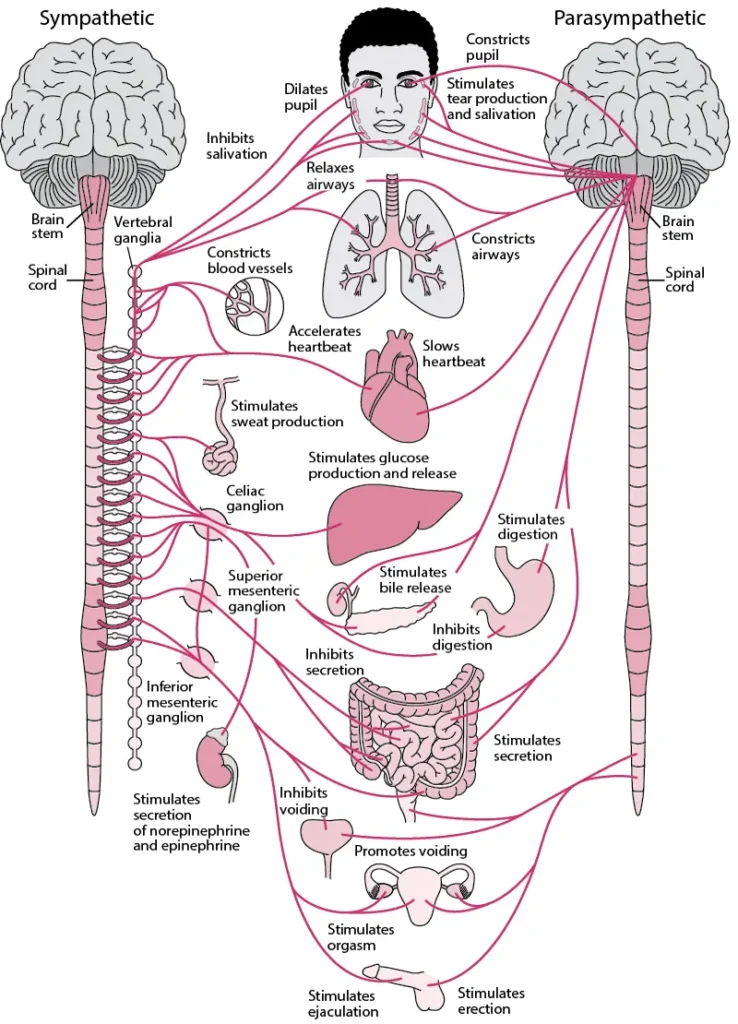
- The autonomic nervous system (ANS), also known as the vegetative nervous system, is a crucial division of the nervous system that regulates and controls the internal organs, smooth muscles, and glands in the body. Unlike the somatic nervous system, which is responsible for voluntary actions, the autonomic nervous system primarily operates unconsciously and autonomously, managing vital bodily functions such as heart rate, digestion, respiratory rate, pupil size, urination, and sexual arousal. Additionally, the ANS plays a central role in the fight-or-flight response, the body’s physiological reaction to stress or danger.
- The autonomic nervous system functions through integrated reflexes that involve the brainstem, spinal cord, and various organs. It oversees essential processes like respiration, cardiac regulation, vasomotor activity, and reflex actions such as coughing, sneezing, swallowing, and vomiting. These functions are further divided into subsystems and are interconnected with the peripheral nervous system. The hypothalamus, located just above the brainstem, acts as an integrator for autonomic functions, receiving regulatory input from the limbic system.
- Traditionally, the autonomic nervous system has been categorized into four branches: the sympathetic nervous system, parasympathetic nervous system, visceral sensory nervous system, and enteric nervous system. The sympathetic nervous system is often referred to as the “fight or flight” system, while the parasympathetic nervous system is known as the “rest and digest” or “feed and breed” system. These two systems often exhibit opposite actions, where one activates a physiological response while the other inhibits it. However, it is important to note that the “excitatory” and “inhibitory” categorizations are oversimplified, and the sympathetic and parasympathetic systems have complex interactions and exceptions, as observed in sexual arousal and orgasm.
- Within the autonomic nervous system, there are inhibitory and excitatory synapses between neurons. Additionally, a subset of neurons called non-noradrenergic, non-cholinergic transmitters uses nitric oxide as a neurotransmitter and plays a significant role in autonomic function, especially in the gut and lungs.
- While the autonomic nervous system is also referred to as the visceral nervous system and primarily carries non-somatic information to the central nervous system, it is still considered connected to the motor side. Although most autonomous functions are involuntary, they can work in conjunction with the somatic nervous system, which provides voluntary control.
- In summary, the autonomic nervous system is an integral part of the peripheral nervous system responsible for regulating involuntary physiological processes such as heart rate, blood pressure, respiration, digestion, and sexual arousal. It consists of the sympathetic, parasympathetic, and enteric divisions. The sympathetic division triggers the “fight or flight” response, while the parasympathetic division promotes the “rest and digest” processes. The enteric division independently regulates digestive functions. These divisions interact through complex neural pathways and utilize various neurotransmitters to orchestrate the harmonious functioning of the body’s internal processes.
Definition of Autonomic nervous system
The autonomic nervous system (ANS) is a division of the nervous system responsible for regulating involuntary bodily functions such as heart rate, digestion, respiration, and sexual arousal. It consists of the sympathetic, parasympathetic, and enteric divisions, which work together to maintain homeostasis and respond to stress or danger.
What Controls The Autonomic Nervous System?
The autonomic nervous system (ANS) is controlled by various factors, including external stimuli, internal signals, and specific neurotransmitters. The hypothalamus, located above the brain stem, plays a crucial role in regulating the ANS. It receives autonomic regulatory input from the limbic system, which is involved in memory, emotion, and fear. The hypothalamus integrates this input to exert control over the activities of the ANS.
In addition to the influence of the hypothalamus, neurotransmitters play a significant role in facilitating communication within the autonomic nervous system. Three primary neurotransmitters are involved in regulating ANS functions:
- Acetylcholine: Found predominantly in the parasympathetic nervous system, acetylcholine has an inhibitory effect. It is responsible for transmitting signals that promote rest, relaxation, and digestion.
- Epinephrine (Adrenaline): Epinephrine is primarily associated with the sympathetic nervous system, which triggers the “fight or flight” response. It has a stimulating effect, preparing the body for intense physical activity and responses to stress or danger.
- Norepinephrine (Noradrenaline): Norepinephrine is also primarily found in the sympathetic nervous system. It acts as a neurotransmitter that has a stimulating effect, assisting in the body’s preparation for heightened activity, increased alertness, and stress response.
These neurotransmitters, along with other signaling molecules, facilitate the transmission of signals between neurons and contribute to the regulation of autonomic functions. The balance and interaction of these neurotransmitters within the autonomic nervous system are crucial for maintaining homeostasis and coordinating appropriate physiological responses in various situations.
Structure of Autonomic nervous system – Divisions Of The ANS
The structure of the autonomic nervous system (ANS) is characterized by its divisions, namely the sympathetic and parasympathetic nervous systems. Traditionally, the ANS was thought to be exclusively motor, but recent understanding has expanded to include sensory components as well.
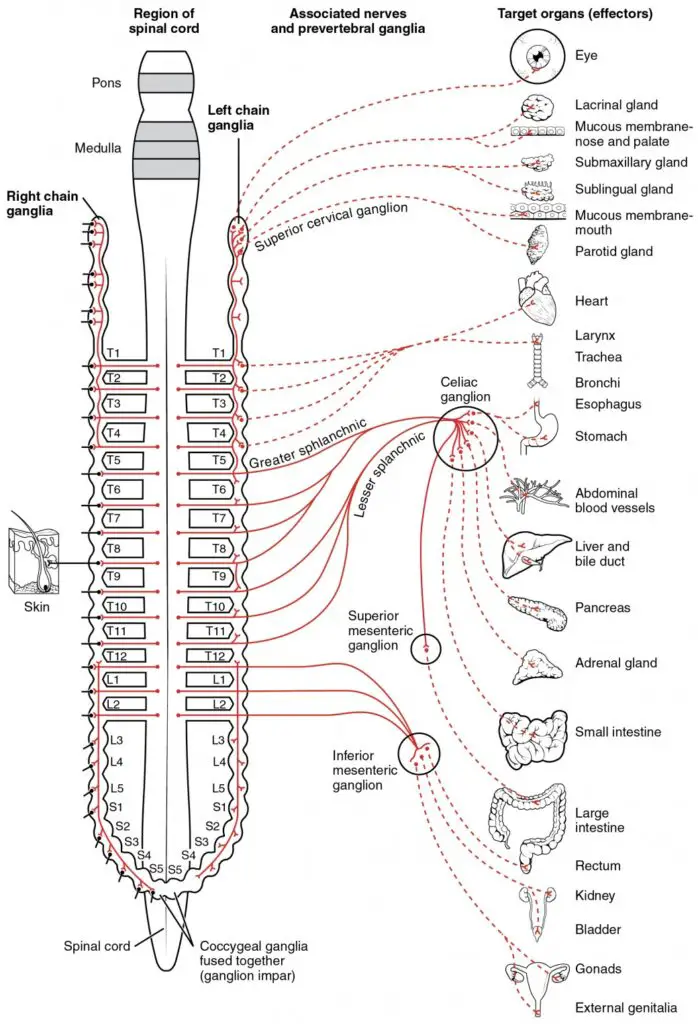
The sympathetic division of the ANS emerges from the spinal cord in the thoracic and lumbar regions, typically extending from T1 to L2-3. This division is responsible for preparing the body for intense physical activity or response to stress. It mobilizes energy resources, increases heart rate, dilates blood vessels, and redirects blood flow to the muscles. The sympathetic division is often associated with the “fight or flight” response.
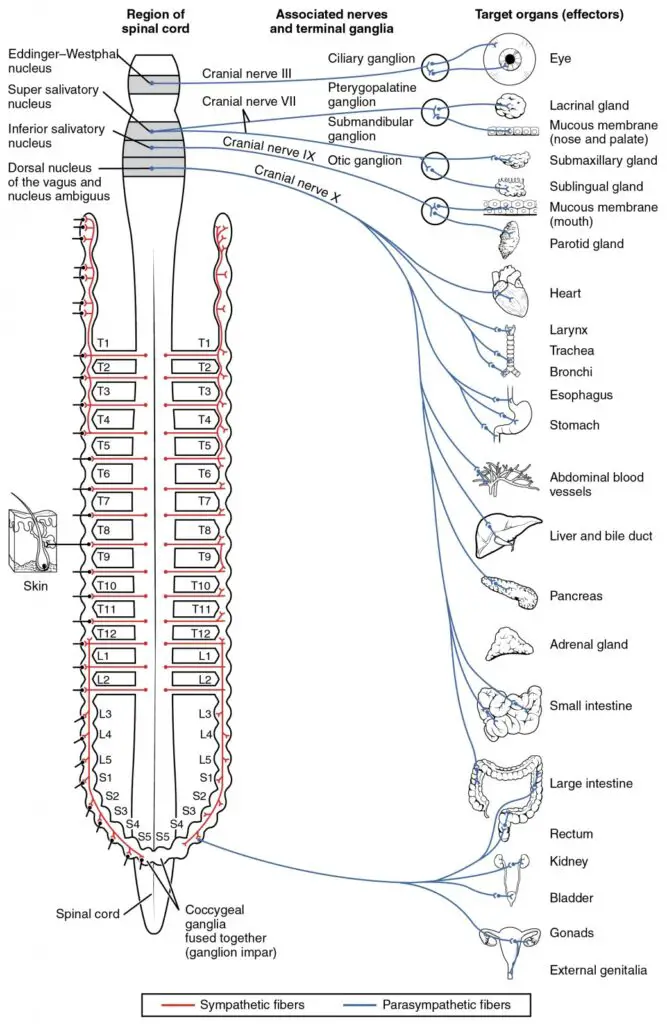
On the other hand, the parasympathetic division has craniosacral “outflow.” This means that the neurons of this division originate from the cranial nerves, specifically the oculomotor nerve (III), facial nerve (VII), glossopharyngeal nerve (IX), and vagus nerve (X). Additionally, the parasympathetic division has its origins in the sacral (S2-S4) spinal cord. The parasympathetic division is responsible for promoting relaxation, digestion, and other restorative functions. It slows heart rate, constricts blood vessels, stimulates digestion, and enhances activities that conserve energy.
One unique aspect of the autonomic nervous system is its two-neuron efferent pathway. In this pathway, the preganglionic neuron originates from the “outflow” (craniosacral or thoracic-lumbar) and synapses onto the cell body of the postganglionic neuron. This synapse occurs in a ganglion located outside the central nervous system. The postganglionic neuron then extends to innervate the target organ or tissue. This sequential two-neuron pathway allows for complex and coordinated control of autonomic functions.
It is worth noting that recent advancements have shown that the ANS may also include sensory components, contributing to the regulation and integration of autonomic functions. These sensory components involve the transmission of information from the internal organs and tissues back to the central nervous system.
In summary, the structure of the autonomic nervous system is characterized by its divisions, the sympathetic and parasympathetic divisions. The sympathetic division arises from the thoracic and lumbar spinal cord, while the parasympathetic division has craniosacral origins. The two-neuron efferent pathway, consisting of preganglionic and postganglionic neurons, allows for precise control and coordination of autonomic functions.
1. Sympathetic Nervous System
- The sympathetic nervous system (SNS) plays a crucial role in the body’s response to emergencies and stressful situations. It is responsible for inhibiting bodily processes that are less important in such situations, such as digestion. For example, when the body is exposed to a hot room, the sympathetic system stimulates sweating as a response to regulate body temperature.
- One of the most noticeable functions of the sympathetic branch is its involvement in the fight-or-flight response. When faced with threatening or stressful conditions, the sympathetic system activates, triggering an automatic response. For instance, walking alone down a dark street can elicit this response, causing your pupils to dilate, heart rate to increase, and sweat to be produced.
- This stress response is initiated by the release of a large amount of the neurotransmitter epinephrine from the adrenal gland. Epinephrine stimulates the body’s automatic responses, preparing the individual to either escape from or confront dangerous situations.
- While the sympathetic nervous system has evolved to respond to life-threatening situations, it can also be triggered by modern-day stressors and mental health issues. Work-related stress, financial concerns, and relationship problems are examples of situations that can activate the sympathetic nervous system and produce a stress response. Individuals with anxiety disorders and phobias may experience high levels of epinephrine, leading to the same autonomic responses observed in life-threatening situations.
- The sympathetic nervous system is composed of cells with bodies located in the lateral grey column spanning from T1 to L2/3. These cell bodies are known as general visceral efferent (GVE) neurons and serve as preganglionic neurons. These preganglionic neurons can synapse with postganglionic neurons at various locations, including paravertebral ganglia, cervical ganglia, thoracic ganglia, rostral lumbar ganglia, caudal lumbar ganglia, sacral ganglia, prevertebral ganglia, and chromaffin cells of the adrenal medulla.
- Paravertebral ganglia, which run alongside the vertebral bodies, are found in the sympathetic chain and consist of three cervical, twelve thoracic, four lumbar, and five sacral ganglia. Prevertebral ganglia, including the celiac ganglion, aorticorenal ganglion, superior mesenteric ganglion, and inferior mesenteric ganglion, are part of the nervous plexuses surrounding the branches of the aorta.
- The sympathetic nervous system communicates with its target organs through postganglionic neurons originating from these ganglia. Nerves called splanchnic nerves transmit the signals to their respective target organs. These nerves include cervical cardiac nerves, thoracic visceral nerves, thoracic splanchnic nerves, lumbar splanchnic nerves, and sacral splanchnic nerves.
- The sympathetic nervous system follows a two-neuron pathway, except for its connection to the adrenal medulla. In this case, the presynaptic fibers directly synapse onto chromaffin cells in the adrenal medulla, which release epinephrine into the bloodstream.
- Postganglionic sympathetic neurons release norepinephrine (NE) that acts on adrenergic receptors in target tissues. The specific subtype of receptor, such as alpha-1, alpha-2, beta-1, beta-2, or beta-3, determines the affinity of NE for the receptor and influences the response in the target tissue.
- The sympathetic nervous system regulates various physiological functions. It controls blood vessels, primarily inducing vasoconstriction in most cases, except in certain vessels supplying the coronary arteries, skeletal muscles, and external genitalia where vasodilation occurs. Sympathetic activation also increases heart rate and contractile force, but excessive sympathetic activity can have detrimental effects on cardiac function in individuals with compromised health.
- Additionally, the sympathetic nervous system contributes to the regulation of the respiratory cycle by complementing the parasympathetic nervous system during inspiration, which results in the dilation of airways for proper airflow.
- The SNS also modulates the immune response by innervating immune organs such as the spleen, thymus, and lymph nodes. It can influence inflammation, with different receptor subtypes being expressed on cells of the innate and adaptive immune systems.
- Most postganglionic sympathetic neurons release norepinephrine and additional peptides, such as neuropeptide Y or somatostatin. These peptides help modulate the response of the postsynaptic neuron to the primary neurotransmitter. Cholinergic sympathetic postganglionic neurons, found in sweat glands and precapillary resistance vessels in skeletal muscle, produce vasoactive intestinal polypeptide and acetylcholine. Calcitonin gene-related peptide, a potent vasodilator, has also been identified in paravertebral sympathetic neurons.
- Overall, the sympathetic nervous system is essential for the body’s response to emergencies and stress. It regulates various physiological processes, prepares the body for fight-or-flight responses, and modulates immune and inflammatory reactions. Understanding the intricacies of the sympathetic nervous system helps shed light on how the body adapts and responds to different situations.
Functions of Sympathetic nervous system
The sympathetic nervous system is responsible for promoting the “fight-or-flight” response in the body. It plays a crucial role in generating arousal, increasing energy levels, and inhibiting certain bodily functions such as digestion. Here are some key functions of the sympathetic nervous system:
- Diversion of Blood Flow: The sympathetic nervous system causes vasoconstriction, redirecting blood away from the gastrointestinal tract (GI) and skin. This redistribution of blood flow allows for enhanced blood supply to skeletal muscles and lungs, which is important during times of heightened activity or stress.
- Enhanced Blood Flow to Muscles and Lungs: By increasing blood flow to skeletal muscles and lungs, the sympathetic system ensures that these vital areas receive adequate oxygen and nutrients. Blood flow to skeletal muscles can increase by as much as 1200%, enabling increased physical performance.
- Bronchial Dilation: The sympathetic system stimulates the dilation of bronchioles in the lungs. This action is achieved through the release of epinephrine, also known as adrenaline, which circulates in the body. Bronchial dilation enhances alveolar oxygen exchange, allowing for improved respiratory function during periods of heightened activity.
- Increased Heart Rate and Contractility: The sympathetic system accelerates heart rate and enhances the contractility of cardiac cells (myocytes). This response ensures an increased blood supply to skeletal muscles, facilitating their optimal functioning during fight-or-flight situations.
- Pupillary Dilation and Improved Vision: Activation of the sympathetic system leads to the dilation of pupils and relaxation of the ciliary muscle in the lens of the eye. These actions allow more light to enter the eye, enhancing far vision and improving visual acuity.
- Vasodilation for Coronary Vessels: The sympathetic system provides vasodilation specifically for the coronary vessels of the heart. This ensures an adequate blood supply to the heart muscle, supporting its increased demand during times of heightened physical activity or stress.
- Sphincter Constriction: The sympathetic system causes constriction of the intestinal sphincters and the urinary sphincter. This action inhibits the movement of contents through the intestines (peristalsis) and contributes to the suppression of urinary excretion.
- Stimulation of Orgasm: The sympathetic system plays a role in stimulating orgasm, contributing to the physiological responses associated with sexual arousal and climax.
- Sudomotor Function: The sympathetic system innervates sweat glands through postganglionic sympathetic nerve fibers. This characteristic pattern of innervation allows clinicians and researchers to assess the functioning of the autonomic nervous system by conducting sudomotor function testing, which measures electrochemical skin conductance.
The functions of the sympathetic nervous system are vital for responding to stressful or threatening situations by preparing the body for action, optimizing physiological responses, and redirecting resources to support physical performance.
2. Parasympathetic Nervous System
- The parasympathetic nervous system is responsible for promoting relaxation and returning the body to a resting state after a stressful situation has passed. It works to maintain homeostasis by regulating various functions such as heart rate, muscle relaxation, and bladder control.
- The parasympathetic nervous system consists of preganglionic neurons located in the brainstem (Cranial Nerves III, VII, IX, X) or the sacral spinal cord (S2, S3, S4). These preganglionic neurons synapse with postganglionic neurons in specific locations, including parasympathetic ganglia of the head (such as ciliary, submandibular, pterygopalatine, and otic ganglia) and in or near the wall of target organs innervated by the Vagus (Cranial nerve X) or sacral nerves (S2, S3, S4).
- Postganglionic parasympathetic neurons, which originate from these ganglia, provide innervation to target organs. For example, parasympathetic splanchnic (visceral) nerves and the vagus nerve (CN X) innervate various thoracic and abdominal viscera, including the heart, lungs, liver, stomach, and colon.
- The vagus nerve is a major component of the parasympathetic nervous system, responsible for promoting “rest and digest” processes. It has multiple cell bodies in the medulla oblongata, including the dorsal nucleus, nucleus ambiguus, nucleus solitarius, and spinal trigeminal nucleus. The vagus nerve plays a crucial role in cardiac relaxation by reducing contractility in the atria and slowing conduction through the atrioventricular node. It also promotes salivation and enhances peristaltic and secretory activity in the digestive system. Additionally, the vagus nerve influences the respiratory cycle by contracting and stiffening the airways during expiration.
- The parasympathetic nervous system is involved in monitoring the body’s recovery and responding to foreign invaders. Sensory fibers of the vagus nerve innervate major organs and express receptors for key immune response molecules like interleukin-1. Activation of the parasympathetic nervous system through the vagus nerve can trigger the release of glucocorticoids and norepinephrine, which are involved in the inflammatory immune response.
- Postganglionic parasympathetic neurons release acetylcholine (ACh), which acts on muscarinic and nicotinic receptors. Different subunits of these receptors, such as M1, M2, M3, N1, and N2, mediate the effects of ACh. In addition to ACh, parasympathetic neurons also release peptides like vasoactive intestinal peptide (VIP), neuropeptide Y (NPY), and calcitonin gene-related peptide (CGRP).
- Understanding the parasympathetic nervous system provides insight into how the body promotes relaxation, maintains homeostasis, and modulates various physiological functions. It complements the sympathetic nervous system and together they ensure a balanced response to different situations and stimuli.
Functions of Parasympathetic nervous system
The parasympathetic nervous system is responsible for promoting a “rest and digest” response in the body, facilitating a return to regular function and enhancing digestion. It plays a crucial role in promoting a state of relaxation and supporting various physiological processes. Here are some key functions of the parasympathetic nervous system:
- Increased Blood Flow to the GI Tract: The parasympathetic system dilates blood vessels leading to the gastrointestinal (GI) tract, promoting increased blood flow. This enhanced blood supply supports optimal digestion and nutrient absorption in the digestive organs.
- Constriction of Bronchioles: When the need for oxygen has diminished, the parasympathetic system constricts the bronchiolar diameter in the lungs. This action helps regulate respiratory function and maintains appropriate airflow during restful states.
- Cardiac Control: The parasympathetic system exerts dedicated control over the heart through branches of the vagus and thoracic spinal accessory nerves. These nerves slow down the heart rate and exert parasympathetic influence on the myocardium, contributing to overall cardiac regulation and maintaining a steady rhythm.
- Pupillary Constriction and Ciliary Muscle Contraction: Activation of the parasympathetic system leads to the constriction of the pupil (miosis) and contraction of the ciliary muscles in the eye. These actions facilitate accommodation, allowing the lens to focus on nearby objects and enabling closer vision.
- Stimulation of Salivary Glands and Peristalsis: The parasympathetic system stimulates salivary gland secretion, promoting the production of saliva. Additionally, it accelerates peristalsis, the wave-like muscular contractions that move food through the digestive tract. These actions support the breakdown and digestion of food and indirectly aid in the absorption of nutrients.
- Sexual Function: The parasympathetic system plays a significant role in sexual function. Peripheral nerves, such as the pelvic splanchnic nerves 2–4, are involved in the erection of genital tissues. They are also responsible for stimulating sexual arousal and facilitating the physiological responses associated with sexual activity.
The functions of the parasympathetic nervous system are crucial for promoting a state of relaxation, optimizing digestion, regulating cardiac activity, and supporting sexual function. It counterbalances the effects of the sympathetic nervous system, allowing the body to return to a resting state and maintain overall homeostasis.
3. Enteric Nervous System
- The enteric nervous system (ENS) is a division of the autonomic nervous system (ANS) that operates independently from the central nervous system (CNS). It is primarily located within the gastrointestinal tract, also known as the gut, and consists of a network of neurons responsible for controlling various motor functions and secreting enzymes within the digestive system.
- The ENS can function autonomously, but it can also be influenced by the sympathetic and parasympathetic nervous systems. It comprises sensory, motor, and interneurons that work together to regulate gastrointestinal activities.
- Communication between neurons in the enteric system occurs through the release of neurotransmitters such as dopamine, serotonin, and acetylcholine. These neurotransmitters play important roles in modulating the functions of the digestive system, including the control of local blood flow and immune responses.
- The enteric nervous system is composed of two ganglionated plexuses: the myenteric (Auerbach) plexus and the submucosal (Meissner) plexus. The myenteric plexus is located between the layers of smooth muscles in the gastrointestinal tract, while the submucosal plexus is situated within the submucosal layer. Although the ENS operates through local reflex activity, it often receives input from and provides feedback to the sympathetic and parasympathetic divisions of the ANS.
- The submucosal plexus controls the movement of water and electrolytes across the intestinal wall, while the myenteric plexus coordinates the contractility of the circular and longitudinal muscle cells, enabling peristalsis—the wave-like movement of the intestines that propels food through the digestive tract.
- Motility within the ENS is regulated through a reflex circuit involving the circular and longitudinal muscles. Interneurons facilitate communication between these muscles, mediating the reflex circuits. When a bolus, a mass of food, is present, the reflex circuit is activated, causing excitatory neurons in the circular muscle and inhibitory neurons in the longitudinal muscle to fire. This generates a narrow section of bowel proximal to the bolus, known as the propulsive segment. Simultaneously, excitatory neurons in the longitudinal muscle and inhibitory neurons in the circular muscle fire, creating the “receiving segment” of the bowel, allowing the bolus to move forward. This process repeats for each subsequent section of the bowel.
- The enteric nervous system shares several similarities with the CNS. Enteric neurons can be bipolar, pseudounipolar, or multipolar, and they communicate through excitatory and inhibitory neuromodulation. Like the CNS, the ENS utilizes over 30 neurotransmitters, with cholinergic and nitrergic transmitters being the most common.
- While much of the discussion has focused on the efferent functions of the ANS, the afferent fibers of the ENS play a crucial role in reflex activities that regulate various physiological processes, including heart rate and immune responses. Feedback from the ANS is typically processed at a subconscious level, leading to reflex actions in the visceral or somatic parts of the body. The conscious sensations originating from the viscera are often interpreted as diffuse pain or cramps, which can be associated with feelings of hunger, fullness, or nausea. These sensations are commonly triggered by sudden distention or contractions, chemical irritants, or pathological conditions like ischemia.
Functions of Enteric nervous system
The enteric nervous system (ENS), often referred to as the “Second Brain,” plays a crucial role in the functioning of the gastrointestinal system. It is a complex network of neurons and glial cells that spans the entire length of the digestive tract, from the esophagus to the anus. The ENS operates independently but also communicates with the central nervous system (CNS) to regulate various digestive processes. Let’s delve into the key functions of the enteric nervous system:
- Sensing chemical and mechanical changes in the gut: One of the primary functions of the ENS is to detect and interpret chemical and mechanical signals within the gut. Specialized sensory neurons present in the enteric plexuses are responsible for sensing changes such as the presence of food, nutrient levels, pH, and the mechanical stretching of the intestinal walls. This sensory information helps initiate appropriate responses to optimize digestion and absorption.
- Regulating secretions in the gut: The enteric nervous system controls the secretory activities of the gastrointestinal tract. It influences the release of various substances such as digestive enzymes, acid, mucus, and hormones necessary for proper digestion. Through intricate neural circuits, the ENS coordinates the secretion of these substances at specific locations and times, ensuring efficient breakdown and absorption of nutrients.
- Controlling peristalsis and other movements: Peristalsis refers to the coordinated muscular contractions that propel food along the digestive tract. The ENS orchestrates this essential movement, regulating the sequential contraction and relaxation of the smooth muscles in the intestinal walls. In addition to peristalsis, the enteric nervous system also controls other gut movements, such as mixing and segmental contractions, which aid in the digestion and absorption processes.
- Modulating blood flow and nutrient absorption: The enteric nervous system plays a role in regulating blood flow to the gastrointestinal tract. It can adjust blood vessel diameter and blood flow rates in response to various stimuli, ensuring an adequate supply of oxygen and nutrients to the digestive organs. Additionally, the ENS influences the rate of nutrient absorption across the intestinal epithelium, thereby contributing to the overall efficiency of the digestive process.
- Immune regulation and gut-brain communication: Research suggests that the enteric nervous system interacts closely with the immune system in the gut. It can modulate immune responses, influencing the activity of immune cells and the release of inflammatory mediators. Furthermore, the ENS communicates bidirectionally with the central nervous system, allowing for a constant exchange of information between the gut and the brain. This gut-brain communication may impact aspects of behavior, mood, and overall well-being.
The enteric nervous system’s multifaceted functions highlight its critical role in maintaining digestive homeostasis. It operates independently, capable of orchestrating complex processes within the gastrointestinal tract. Simultaneously, it communicates with the central nervous system to ensure coordination and integration with the rest of the body. Understanding the intricacies of the enteric nervous system enhances our knowledge of gastrointestinal disorders and opens up potential avenues for therapeutic interventions targeting this fascinating “Second Brain.”
Sensory neurons
- Sensory neurons play a crucial role in the transmission of sensory information from various parts of the body to the central nervous system (CNS), allowing us to perceive and respond to our environment. Within the autonomic nervous system (ANS), sensory neurons form the sensory arm, which monitors and relays important information related to visceral functions and sensory perception.
- Primary visceral sensory neurons are located in the peripheral nervous system (PNS) and are found in cranial sensory ganglia, including the geniculate, petrosal, and nodose ganglia. These ganglia are associated with cranial nerves VII, IX, and X, respectively. The primary function of these sensory neurons is to monitor and transmit information regarding vital physiological parameters such as carbon dioxide and oxygen levels, blood sugar levels, arterial pressure, and the chemical composition of the stomach and gut contents.
- Additionally, these sensory neurons are responsible for conveying the senses of taste and smell, which are conscious perceptions unlike many other functions of the autonomic nervous system. The carotid body, a cluster of chemosensors located at the bifurcation of the carotid artery and innervated by the petrosal (IXth) ganglion, directly senses blood oxygen and carbon dioxide levels.
- The primary sensory neurons project or synapse onto “second order” visceral sensory neurons located in the medulla oblongata. These second-order neurons form the nucleus of the solitary tract (nTS), which integrates and processes all visceral information received from the primary sensory neurons. The nTS also receives input from the nearby chemosensory center known as the area postrema. The area postrema is responsible for detecting toxins in the blood and cerebrospinal fluid, playing a crucial role in chemically induced vomiting and the formation of conditional taste aversion.
- The continuous flow of visceral sensory information from these neurons provides unconscious modulation of the activity of motor neurons within the autonomic nervous system. This modulation ensures that the ANS can appropriately respond and regulate various physiological processes to maintain homeostasis.
- In summary, sensory neurons within the autonomic nervous system’s sensory arm monitor and transmit vital information regarding visceral functions, taste, and smell. They synapse with second-order neurons in the medulla oblongata, forming the nucleus of the solitary tract. This integration of sensory information plays a crucial role in the unconscious modulation of autonomic motor neurons, allowing for appropriate physiological responses to maintain overall bodily homeostasis.
Motor neurons
- Motor neurons within the autonomic nervous system play a critical role in transmitting signals from the central nervous system to the effector organs, allowing for the regulation and control of various bodily functions. These motor neurons are located in specific clusters called autonomic ganglia, with distinct distributions in the parasympathetic and sympathetic branches.
- In the parasympathetic branch, the motor neurons are situated in autonomic ganglia located near or within the target organs they innervate. This close proximity allows for short postganglionic connections to the target tissues, facilitating precise and localized control. The ganglia of the parasympathetic branch can be found in various locations depending on the specific target organs involved.
- On the other hand, the motor neurons of the sympathetic branch are located in autonomic ganglia positioned close to the spinal cord. These sympathetic ganglia are organized into two main chains: the pre-vertebral and pre-aortic chains. The pre-vertebral ganglia are situated anterior to the vertebral column, near the abdominal aorta, while the pre-aortic ganglia are located anterior to the aorta in the abdominal cavity. The arrangement of sympathetic ganglia near the spinal cord allows for efficient coordination of responses throughout the body.
- The activity of the autonomic ganglionic neurons, both in the parasympathetic and sympathetic branches, is modulated by preganglionic neurons present in the central nervous system. Preganglionic sympathetic neurons are located in the spinal cord at the thoracic and upper lumbar levels. These neurons project their axons to the sympathetic ganglia, where they synapse with the postganglionic neurons that then innervate target tissues.
- Preganglionic parasympathetic neurons, on the other hand, are found in the medulla oblongata. Within the medulla, they form visceral motor nuclei responsible for controlling various parasympathetic functions. Specific nuclei involved include the dorsal motor nucleus of the vagus nerve, the nucleus ambiguus, the salivatory nuclei, and nuclei located in the sacral region of the spinal cord. The axons of these preganglionic parasympathetic neurons travel within the cranial nerves or the sacral spinal nerves to reach their respective autonomic ganglia, where they synapse with postganglionic neurons that then innervate target organs.
- In summary, motor neurons within the autonomic nervous system are located in autonomic ganglia, with parasympathetic ganglia positioned near target organs and sympathetic ganglia close to the spinal cord. Preganglionic neurons originating in the central nervous system send signals to these ganglia, which in turn transmit postganglionic signals to the effector organs. This intricate arrangement allows for the regulation and coordination of autonomic functions throughout the body.
Autonomic Dysfunction
Autonomic dysfunction, also known as dysautonomia, is a condition characterized by improper functioning of the autonomic nervous system (ANS). The causes of autonomic dysfunction can vary, with diabetes being the most common cause in developed countries. Other factors contributing to autonomic dysfunction include hereditary reasons, aging, Parkinson’s disease, cancer, chronic fatigue syndrome, head or neck nerve damage, alcohol and drug abuse, and infections.
If an individual suspects they may have issues with their ANS, they may experience one or more of the following symptoms:
- Abnormally high or low blood pressure: Autonomic dysfunction can lead to fluctuations in blood pressure, resulting in hypertension or hypotension.
- Lack of pupillary response: The pupils may not properly dilate or constrict in response to changes in light.
- Severe anxiety or depression: Autonomic dysfunction can be associated with mood disorders such as anxiety and depression.
- Digestive issues: Problems with digestion, including constipation or diarrhea, may arise due to autonomic dysfunction.
- Breathing difficulties: Autonomic dysfunction can affect respiratory functions, leading to breathing problems.
- Excessive or insufficient sweating: Sweating may be either excessive or reduced, depending on the type of autonomic dysfunction.
- Tachycardia (abnormally fast heart rate): The heart rate may become rapid and irregular.
- Incontinence issues: Autonomic dysfunction can affect bladder and bowel control, resulting in incontinence problems.
- Aches and pains: Individuals with autonomic dysfunction may experience generalized body aches or specific pain in certain areas.
- Light-headedness: Feeling dizzy or light-headed is a common symptom of autonomic dysfunction.
- Fainting or near-fainting episodes: Some individuals may experience syncope or near-syncope due to inadequate blood flow to the brain.
Autonomic neuropathy refers to the damage of autonomic nerves, affecting either the sympathetic or parasympathetic nerves, or both. Symptoms of autonomic neuropathy include a fixed heart rate, constipation, abnormal sweating, decreased pupil size, and absent or delayed light reflexes.
There are several disorders associated with autonomic dysfunction, including:
- Acute autonomic paralysis: Typically linked to spinal cord injury, this condition results in uncontrolled hypertension.
- Multiple system atrophy: This rare condition causes progressive damage to nerve cells, leading to dysfunction in various body systems.
- Pure autonomic failure: This disorder involves dysfunction of multiple processes controlled by the autonomic nervous system.
- Familial dysautonomia (Riley-Day syndrome): A hereditary condition in which nerve fibers do not function properly, causing difficulties in sensation and coordination of limbs, as well as challenges in feeling pain, temperature, and pressure.
Autonomic dysfunction can significantly impact an individual’s quality of life, as it affects various bodily functions necessary for maintaining homeostasis. Management of the condition typically involves treating the underlying cause, symptomatic relief, and lifestyle adjustments to minimize the impact of symptoms.
Diagnosis and Treatment of Autonomic Dysfunction
Diagnosing and treating autonomic dysfunction requires a comprehensive approach tailored to the individual’s specific symptoms and underlying causes. Here is an overview of the diagnostic methods and treatment options commonly employed:
Diagnostic Tests:
- Electrocardiogram (ECG): Measures the electrical activity of the heart to assess abnormal heart rhythms or arrhythmias.
- Blood pressure monitoring: Measures blood pressure levels to determine if they are abnormally high or low.
- Sweat tests: Evaluates sweat gland function by measuring sweat volume in response to stimuli using electrodes.
- Pupillary light reflex tests: Assess the sensitivity of the pupils to changes in light and their ability to respond appropriately.
In addition to these physical examinations, the diagnostic process for autonomic dysfunction often involves a series of tests to identify the underlying condition causing the dysfunction.
Treatment Approaches:
- Treating the underlying cause: If autonomic dysfunction is secondary to an underlying condition such as diabetes, managing and controlling the primary disease can help improve ANS function. For example, controlling blood sugar levels in diabetes can mitigate autonomic neuropathy.
- Lifestyle modifications: Adopting certain lifestyle changes can be beneficial in managing autonomic dysfunction. These may include regular exercise, dietary modifications, reducing caffeine intake, managing stress, and ensuring an adequate intake of essential vitamins and minerals.
- Medications: Drug therapies can be prescribed to alleviate symptoms and manage autonomic dysfunction. Depending on the specific symptoms and underlying condition, various medications may be utilized. For example:
- Blood pressure-lowering medications: To regulate blood pressure and manage hypertension.
- Non-steroidal anti-inflammatory drugs (NSAIDs): To control pain, especially in conditions like fibromyalgia.
- Antidepressants and anti-anxiety medications: These can help rebalance the ANS and manage symptoms of anxiety and depression.
- Symptomatic management: Depending on the individual’s symptoms, specific interventions may be recommended to alleviate discomfort or improve daily functioning. This can include therapies such as physical therapy, occupational therapy, or speech therapy, depending on the affected systems.
- Supportive care: In some cases, managing autonomic dysfunction may involve providing supportive care to address specific symptoms. For example, using compression stockings to alleviate orthostatic hypotension (low blood pressure upon standing) or using assistive devices for mobility difficulties.
It’s important to note that the treatment approach for autonomic dysfunction is highly individualized and may require a multidisciplinary approach involving specialists from various fields such as neurology, cardiology, gastroenterology, and psychology. The treatment plan should be tailored to address the specific symptoms, underlying causes, and overall health of the individual. Regular follow-up visits with healthcare professionals are essential to monitor progress and adjust the treatment plan as needed.
Functions of Autonomic nervous system (ANS)
The autonomic nervous system (ANS) is a vital component of the peripheral nervous system responsible for regulating various bodily functions necessary for maintaining homeostasis. It operates largely involuntarily, controlling actions such as salivation, sweating, pupil size changes, heart rate management, crying, and hormone secretion. In recent years, the ANS has also been associated with emotions, with its activation observed during responses to positive and negative emotional experiences.
Here are some key functions of the autonomic nervous system:
- Mechanism for the fight-or-flight response: The sympathetic division of the ANS is responsible for activating the fight-or-flight response in situations that require immediate action. It prepares the body for intense physical activity or potential danger by increasing heart rate, dilating the bronchioles, and constricting blood vessels in certain areas while increasing blood pressure.
- Regulation of blood pressure: The ANS helps regulate blood pressure by controlling the constriction or dilation of blood vessels. The sympathetic division constricts blood vessels in visceral areas, increasing blood pressure, while the parasympathetic division generally has little effect on blood vessel diameter.
- Heart rate regulation: The autonomic nervous system plays a crucial role in controlling heart rate. The parasympathetic division decreases heart rate, while the sympathetic division increases it. These divisions work in a dynamic balance to maintain the heart rate within the appropriate range.
- Secretion of bodily fluids: The ANS influences the secretion of various bodily fluids, including saliva, sweat, and urine. The parasympathetic division stimulates the production of saliva and tears, while the sympathetic division can activate sweat glands to produce perspiration.
- Breathing: The autonomic nervous system contributes to the regulation of respiration. While the parasympathetic division constricts bronchioles, the sympathetic division dilates them, enabling efficient oxygen intake and carbon dioxide removal.
- Body temperature regulation: The ANS helps regulate body temperature. When the body is too hot, the sympathetic division can cause sweat glands to produce perspiration, which aids in cooling. Conversely, in cold conditions, the sympathetic division reduces blood flow to the skin to conserve heat.
- Pupillary responses: The autonomic nervous system controls the size of the pupils in response to varying lighting conditions. The parasympathetic division stimulates the constrictor muscles, leading to pupil constriction, while the sympathetic division stimulates the dilator muscle, causing pupil dilation.
- Regulation of metabolism: The ANS influences metabolic processes in the body. The sympathetic division can stimulate the release of glucose from the liver into the bloodstream, providing a source of energy during times of increased activity or stress.
The autonomic nervous system consists of two main divisions, the sympathetic and parasympathetic divisions, which typically work in a complementary rather than antagonistic manner. The sympathetic division is often associated with the “fight or flight” response, while the parasympathetic division is associated with the “rest and digest” or “feed and breed” response. However, both divisions continuously modulate vital functions to achieve homeostasis, even in situations not directly related to fight or rest scenarios.
Understanding the functions of the autonomic nervous system provides insights into how the body maintains balance and responds to various internal and external stimuli. Its intricate control over bodily processes allows for efficient adaptation and survival in ever-changing environments.
FAQ
What is the autonomic nervous system (ANS)?
The autonomic nervous system is a division of the peripheral nervous system that controls involuntary bodily functions, such as heart rate, digestion, respiration, and glandular activity.
What are the main components of the autonomic nervous system?
The autonomic nervous system consists of two main divisions: the sympathetic nervous system and the parasympathetic nervous system. These divisions work in opposition to regulate different bodily functions.
What is the role of the sympathetic nervous system?
The sympathetic nervous system is responsible for the “fight or flight” response, preparing the body for action in response to stress or danger. It increases heart rate, dilates pupils, and diverts blood flow to vital organs.
What is the role of the parasympathetic nervous system?
The parasympathetic nervous system is often referred to as the “rest and digest” system. It promotes relaxation, conserves energy, and regulates activities such as digestion, urination, and sexual arousal.
How does the autonomic nervous system regulate heart rate and blood pressure?
The autonomic nervous system controls heart rate and blood pressure through a balance of sympathetic and parasympathetic activity. The sympathetic system increases heart rate and raises blood pressure, while the parasympathetic system slows heart rate and decreases blood pressure.
Can the autonomic nervous system be affected by diseases or disorders?
Yes, various conditions can disrupt the functioning of the autonomic nervous system, leading to autonomic dysfunction or dysautonomia. These conditions can include diabetes, Parkinson’s disease, multiple system atrophy, and certain autoimmune disorders.
What are the symptoms of autonomic dysfunction?
Autonomic dysfunction can cause a range of symptoms, including abnormal blood pressure, heart rate fluctuations, digestive issues, temperature regulation problems, excessive sweating, dizziness, fainting, and fatigue.
How is autonomic dysfunction diagnosed?
Diagnosis of autonomic dysfunction involves a combination of medical history evaluation, physical examination, and specialized tests. These tests may include autonomic reflex testing, tilt table testing, sweat testing, and heart rate variability analysis.
Can autonomic dysfunction be treated?
Treatment for autonomic dysfunction aims to manage symptoms and improve quality of life. Depending on the underlying cause, treatment options may include lifestyle modifications, medication to regulate blood pressure or heart rate, physical therapy, and dietary changes.
Can lifestyle changes help improve autonomic function?
Yes, certain lifestyle changes can have a positive impact on autonomic function. Regular exercise, stress management techniques, maintaining a balanced diet, staying hydrated, and getting adequate sleep can all contribute to better autonomic regulation. It’s important to consult with a healthcare professional for personalized advice and guidance.



Baie insiggewend. Dankie! Ek gaan die hele artikel sorgvuldig lees. Effe moeiliker vir ‘n leek om al die biologiese terme te ken.