Table of Contents
What is Cartilage?
- Cartilage is a remarkable tissue that plays a crucial role in the human body. It is a type of connective tissue that provides structural support and protection for various parts of the body, including the joints, nose, airway, intervertebral discs of the spine, and the ear. Unlike other tissues, cartilage is avascular, meaning it lacks blood vessels, and its cells, called chondrocytes, receive nutrients and oxygen through diffusion from surrounding tissues.
- One of the defining characteristics of cartilage is its unique composition. It is composed primarily of water, making it pliable, but it is also incredibly tough and resilient. The main components of cartilage are collagen, proteoglycans, and other non-collagenous proteins. Collagen provides structural support and gives the tissue its tensile strength, while proteoglycans help retain water, giving cartilage its flexibility.
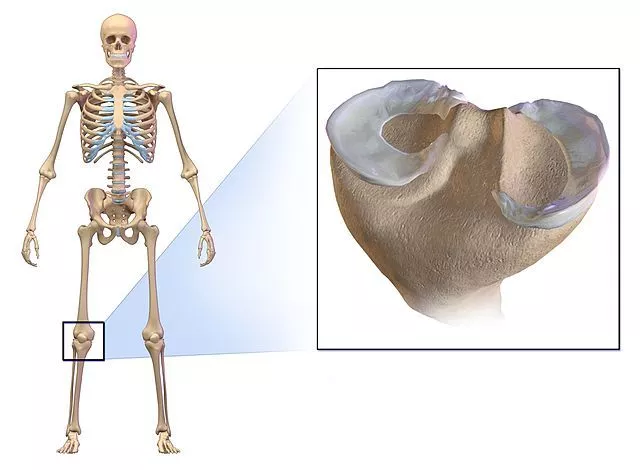
- Cartilage serves several important functions in the body. Firstly, it acts as a shock absorber, cushioning the joints and protecting them from excessive impact during movement. This function is particularly crucial in weight-bearing joints such as the knees and hips. Additionally, cartilage provides a smooth surface for the articulating bones to glide against each other, reducing friction and allowing for smooth joint movement.
- The structure of cartilage contributes to its unique properties. It consists of a dense network of collagen fibers embedded in a firm gelatinous ground substance, giving it a consistency similar to plastic. This structure allows cartilage to withstand compressive forces without breaking or becoming permanently deformed. While it is stiffer than most other connective tissues, it retains a degree of flexibility that exceeds that of bone, enabling it to bear weight while maintaining its shape.
- The neuromuscular supply of cartilage is limited compared to other tissues. As mentioned earlier, cartilage lacks blood vessels, which means it does not have a direct blood supply. Instead, nutrients and oxygen are obtained through diffusion from surrounding tissues and synovial fluid in the joints. This limited supply makes cartilage vulnerable to damage and slower to heal compared to other tissues.
- In conclusion, cartilage is a vital connective tissue in the human body, providing structural support, protection, and flexibility to various organs and joints. Its unique composition, structure, and types enable it to fulfill its functions effectively. While cartilage has remarkable properties, its avascular nature and limited neuromuscular supply make it susceptible to injury and slower healing. Understanding the function and characteristics of cartilage is crucial for maintaining its health and preventing or managing related clinical conditions.
Definition of Cartilage
Cartilage is a semi-rigid and flexible connective tissue found in various parts of the body, such as joints, nose, and ears. It is tough, yet pliable, and provides structural support, cushioning, and smooth surfaces for joint movement.
Location of Cartilage
- Cartilage is located in various regions throughout the human body, serving essential functions in each area. During embryonic development, cartilage acts as a precursor to bone formation. While some cartilage transforms into bone, a significant portion remains in specific locations, providing crucial support and protection.
- One primary location of cartilage is within the joints. It covers the articulating surfaces of bones, forming a smooth and resilient layer that allows for frictionless movement. In weight-bearing joints like the knees and hips, cartilage acts as a shock absorber, reducing the impact and protecting the bones from excessive wear and tear.
- Another prominent location of cartilage is in the nose. The nasal cartilage provides structural support, shaping the external appearance of the nose and maintaining its form. It also contributes to the flexibility required for facial expressions and plays a role in filtering and humidifying the air we breathe.
- Additionally, cartilage makes up a significant portion of the outer ear, known as the auricle or pinna. The elastic cartilage in the ear provides stability and flexibility, enabling us to perceive and localize sounds. It helps collect and direct sound waves into the ear canal, enhancing our ability to hear.
- Cartilage can also be found in other areas of the body, such as the respiratory tract. In the trachea and bronchi, it helps maintain the shape and openness of the airway, ensuring unobstructed airflow during breathing. This cartilage serves as a supportive framework, preventing collapse and facilitating efficient respiration.
- Furthermore, cartilage is present in the intervertebral discs of the spine. These fibrocartilaginous structures act as shock absorbers between the vertebrae, allowing for movement, flexibility, and cushioning while preventing excessive stress on the spinal column. The presence of cartilage in the intervertebral discs contributes to the spine’s overall stability and protection.
- In summary, cartilage is distributed throughout the human body in specific locations. It covers the joints, supports the structure of the nose, comprises the majority of the outer ear, contributes to the airway’s shape, and forms the intervertebral discs in the spine. Understanding the location of cartilage helps us appreciate its vital role in providing support, protection, and flexibility in various regions of the body.
Characteristics of Cartilage
- Flexible and Resilient: Cartilage is a flexible and resilient connective tissue that can bend and withstand compressive forces without easily deforming or breaking.
- Semi-rigid Structure: Cartilage has a semi-rigid structure due to its extracellular matrix, which consists of collagen fibers and proteoglycans. This composition gives cartilage its strength and ability to maintain its shape.
- Avascular: Cartilage is avascular, meaning it lacks blood vessels. Nutrients and oxygen are obtained through diffusion from nearby blood vessels in the surrounding connective tissues.
- Low Cellularity: Cartilage has a low cell density. The main cells found in cartilage are chondrocytes, which are responsible for producing and maintaining the extracellular matrix.
- Lack of Nerves: Cartilage is aneural, meaning it does not contain nerves. Consequently, cartilage itself does not transmit pain signals. Discomfort or pain associated with cartilage injuries or conditions usually arise from adjacent tissues.
- Poor Regeneration Capacity: Cartilage has limited regenerative ability. The chondrocytes present in cartilage have a low rate of division, making the repair of cartilage injuries or damage challenging.
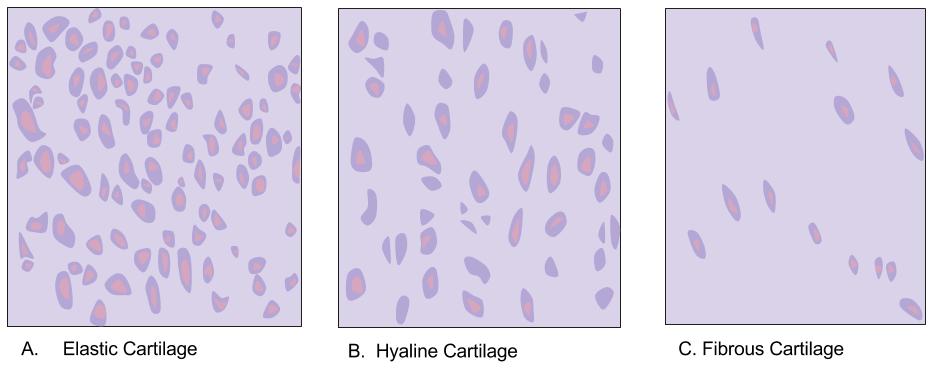
- Three Types: There are three main types of cartilage: a. Hyaline Cartilage: Found in joints, respiratory passages, and developing bones. It provides smooth surfaces for joint movement and flexibility. b. Elastic Cartilage: Present in the external ear, epiglottis, and eustachian tubes. It is more flexible than hyaline cartilage due to the presence of elastic fibers. c. Fibrocartilage: Located in areas that require additional support and shock absorption, such as the intervertebral discs and the menisci of the knee. It has a higher proportion of collagen fibers, making it more durable.
- Important for Joint Function: Cartilage plays a crucial role in joint function by providing a smooth surface for bone articulation, reducing friction, and absorbing shock during movement.
- Scaffold for Bone Development: During bone development, cartilage serves as a scaffold for the formation of the skeletal system. It is later replaced by bone through a process called endochondral ossification.
- Protects Tissues and Organs: Cartilage acts as a protective cushion between bones, preventing them from rubbing against each other and minimizing damage to surrounding tissues and organs.
- Aging and Degeneration: Cartilage can undergo degenerative changes with aging, leading to conditions such as osteoarthritis, where the cartilage gradually breaks down, causing pain and joint dysfunction.
Structure of Cartilage
Cartilage consists of 3 main elements:
- Specialised cells
- The extracellular matrix
- Collagen fibres
Cartilaginous tissue is protected and mechanically supported by a fibrous covering termed the perichondrium (which functions similarly to the periosteum in bone).
The Specialised Cells
- Cartilage consists of two main types of specialized cells: chondroblasts and chondrocytes. These cells play distinct roles in the development, maintenance, and repair of cartilaginous tissue.
- Chondroblasts are primarily found near the outer surface of the cartilage, beneath a layer called the perichondrium. They are responsible for synthesizing and secreting the extracellular matrix of the cartilage. The extracellular matrix is composed of collagen fibers, proteoglycans, and other non-collagenous proteins that provide structural support and flexibility to the tissue. As chondroblasts secrete the matrix, they become surrounded and trapped within it. This process leads to their transformation into mature chondrocytes.
- As cartilage continues to grow, chondrocytes play a crucial role in maintaining its integrity. These specialized cells are housed within small spaces called lacunae, which can be thought of as tiny lakes or pits within the extracellular matrix. Chondrocytes are responsible for maintaining the cartilaginous matrix by producing new components and regulating its composition. They play a vital role in balancing the synthesis and degradation of the extracellular matrix, ensuring the proper function and stability of the cartilage.
- While chondroblasts are mainly involved in the formation of new cartilaginous tissue, chondrocytes are responsible for its ongoing maintenance. Chondrocytes actively monitor and respond to mechanical and biochemical signals, adjusting their activity to preserve the structural integrity and functionality of the cartilage. Through their metabolic activity, chondrocytes contribute to the turnover and repair of the extracellular matrix, allowing the cartilage to adapt and heal in response to injury or normal wear and tear.
- The balance between chondroblast activity and chondrocyte maintenance is essential for the overall health and function of cartilage. Disruptions in this balance can lead to cartilage degeneration and the development of conditions such as osteoarthritis, where the breakdown of the extracellular matrix exceeds its repair.
- In summary, chondroblasts and chondrocytes are the main types of specialized cells found in cartilage. Chondroblasts secrete the extracellular matrix, becoming entrapped within it and transforming into chondrocytes. Chondrocytes, located within lacunae, maintain the cartilage by regulating the composition of the extracellular matrix and participating in its turnover and repair. The coordinated activity of these cell types is crucial for the development, maintenance, and repair of cartilaginous tissues in the body.
The Extracellular Matrix
- The extracellular matrix (ECM) is a crucial component of cartilage, providing structural support, flexibility, and resistance to compressive forces. It is composed of three main elements: aggrecans, water, and collagen fibers along with other constituents.
- Aggrecans, which make up about 10% of the ECM, are a type of proteoglycan. Proteoglycans consist of carbohydrates called glycosaminoglycans (GAGs) attached to a protein core. In the case of aggrecans, they form large aggregates with hyaluronic acid, a long-chain carbohydrate. These aggregates have a negative charge, which allows them to attract and bind water molecules. The presence of aggrecans and the associated water content give cartilage its characteristic resilience and ability to withstand compressive forces.
- Water comprises approximately 75% of the ECM. The ability of the aggrecan aggregates to attract and retain water molecules creates a gel-like environment within the cartilage. This water-rich gel provides lubrication, shock absorption, and diffusion of nutrients and waste products throughout the tissue. The high water content also contributes to the flexibility and pliability of cartilage.
- Collagen fibers and other constituents make up the remaining 15% of the ECM. Collagen fibers are responsible for providing the cartilage with high tensile strength. They form a dense network throughout the tissue, creating a scaffold that helps maintain the structural integrity of the cartilage. The arrangement and orientation of collagen fibers contribute to the tissue’s resistance to stretching and tearing.
- In addition to collagen fibers, the ECM may contain other constituents, including elastic fibers. Elastic fibers provide elasticity and flexibility to cartilage, allowing it to deform and recoil without permanent damage. The ratio of collagen fibers to elastic fibers in cartilage varies depending on its specific function. For example, in weight-bearing cartilage, such as that found in the knees and hips, collagen fibers predominate to provide greater tensile strength. In contrast, cartilage in the outer ear requires more elasticity and flexibility, so the proportion of elastic fibers is higher.
- The intricate composition of the extracellular matrix in cartilage, with its aggrecans, water, collagen fibers, and other constituents, ensures the tissue’s unique properties. It provides strength, flexibility, shock absorption, and lubrication, enabling cartilage to perform its essential functions in the body.
Cartilage Growth and Repair
- Growth of Cartilage: a. Appositional growth: Chondroblasts produce new matrix along the surface of the inner cellular layer of the perichondrium. b. Interstitial growth: Chondrocytes divide and produce new matrix from within the cartilage during childhood and adolescence.
- Blood Supply: a. Cartilage is avascular, lacking a direct blood supply. b. Nutrients are obtained through diffusion from nearby capillaries in the perichondrium. c. The absence of a blood supply restricts cartilage thickness and slows cell turnover.
- Nervous Supply: a. Cartilage is aneural, meaning it does not contain nerves. b. Pain associated with cartilage pathology usually arises from irritation of surrounding tissues.
- Repair of Cartilage: a. Cartilage damage can occur due to overuse or direct injury. b. Challenges in cartilage repair: i. Chondrocytes are fixed in lacunae and cannot migrate to repair damaged areas. ii. Cartilage is avascular, leading to slow deposition of new cartilage. c. Damaged hyaline cartilage is often replaced with fibrocartilage, which is less suited for the original cartilage’s function at that site.
Types of Cartilage
There are 3 types of cartilage
- Hyaline
- Elastic
- Fibro-cartilage
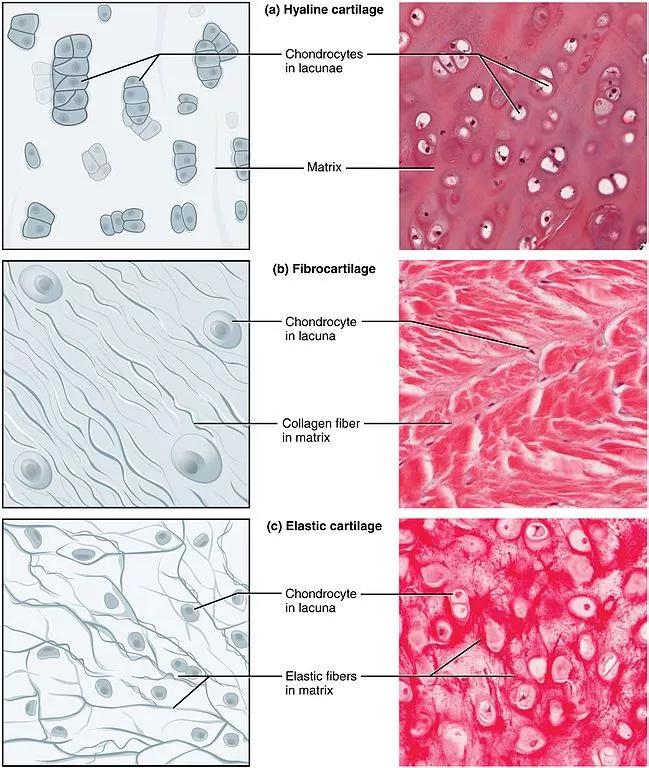
1. Hyaline cartilage
- Common and Weakest Type: Hyaline cartilage is the most common form of cartilage in the body, but it is also the weakest type.
- Composition: It mainly consists of collagen (type II) with relatively few elastic fibers. It is surrounded by a perichondrium, a layer of connective tissue.
- Precursor for Bone: Hyaline cartilage serves as a precursor for bone formation. It is found in the epiphyseal growth plates of children, where bone growth occurs.
- Locations: Hyaline cartilage is found in various parts of the body, including the ribs, nose, larynx, and trachea.
- Articular Cartilage: It is a specialized type of hyaline cartilage found on the surface of bones in synovial joints. It has a unique structure organized into specific zones.
- Chondrocyte Organization: In articular cartilage, chondrocytes at the surface are flattened, while in deeper layers, they are stacked in columns within a calcified matrix, increasing their resistance to compressive forces.
- Lack of Perichondrium: Unlike other hyaline cartilage, articular cartilage does not have an overlying perichondrium. Instead, it is covered by the synovial membrane.
- Appearance: Hyaline cartilage is translucent, blueish-white, and shiny, giving it a glass-like appearance.
- Thickness and Vascularization: Hyaline cartilage is usually thin, ranging from 2 to 4 mm, as it lacks blood vessels. Nutrients and oxygen are obtained through diffusion.
- Embryonic Form: Hyaline cartilage represents the embryonic form of cartilage.
- Collagen Fibers: The collagen fibers in hyaline cartilage are primarily type II, extremely thin, and not visible under a microscope due to their refractory properties similar to the matrix itself.
2. Elastic Cartilage
- Composition: Elastic cartilage contains collagen and an abundance of elastic fibers. Chondrocytes, the cartilage cells, are present within a threadlike network formed by the elastic fibers.
- Resilient and Flexible: Elastic cartilage is highly resilient and flexible. It can deform and then return to its original shape without permanent damage.
- Locations: It is found in structures that commonly undergo deformation, such as the outer ear (auricle or pinna), larynx, and epiglottis.
- Perichondrium: Similar to hyaline cartilage, elastic cartilage also has a perichondrium, a layer of connective tissue that surrounds and supports the cartilage.
- Specific Anatomical Sites: Elastic cartilage is primarily present in the external ear (auricle or pinna), the Eustachian tube, and the epiglottis.
- Structural Role: Elastic cartilage serves a purely structural role in the body. It provides flexibility and resilience due to a combination of elastic fibers and type II collagen fibers.
- Color and Microscopic Appearance: Elastic cartilage appears yellow in color. Under a microscope, it lacks the organized structure seen in fibrocartilage.
- Importance of Shape Retention: The presence of elastic cartilage in certain anatomical structures, such as the outer ear, is essential for maintaining their shape and allowing them to spring back after deformation.
- Function in the Larynx and Epiglottis: In the larynx, elastic cartilage contributes to the elasticity and support of vocal folds. In the epiglottis, it assists in the closing of the airway during swallowing.
- Elastic Fibers: The abundant elastic fibers within elastic cartilage allow for its characteristic flexibility, providing the ability to bend and stretch without permanent damage.
3. Fibro-Cartilage
- Strength and Location: Fibrocartilage is the strongest type of cartilage. It is found in structures such as joint capsules, tendon insertions, ligaments, and intervertebral disks.
- Composition: Fibrocartilage consists of alternating layers of hyaline matrix and dense collagen fibers.
- Reinforcement: Thick layers of collagen fibers within fibrocartilage are oriented in the direction of pressure applied, further enhancing its strength and reinforcement.
- Absence of Perichondrium: Fibrocartilage does not always have a perichondrium, a connective tissue layer that surrounds other types of cartilage. Instead, it is often directly connected to hyaline cartilage, tendons, or ligaments.
- Locations: Fibrocartilage is found at sites where tendons and ligaments meet bone, such as the pubic symphysis, menisci (knee), sternoclavicular joint, and the annulus fibrosus in the intervertebral discs.
- Strength and Pliability: Fibrocartilage exhibits both strength and pliability, allowing it to withstand significant pressure and provide support to the joints and areas prone to mechanical stress.
- Collagen Fiber Orientation: Collagen fiber bundles in fibrocartilage run parallel to each other, enabling limited stretch and contributing to its resilience.
- White Appearance: Due to the abundance of collagen fibers, fibrocartilage appears white in color.
- Composition: Fibrocartilage is composed of both type II and type I collagen fibers, providing a combination of structural support and tensile strength.
- Function: Fibrocartilage acts as a shock absorber, providing stability and cushioning to the joints and facilitating smooth movement.
- Lack of Elastic Fibers: Unlike elastic cartilage, fibrocartilage does not contain abundant elastic fibers and is therefore less flexible.
- Healing and Repair: Fibrocartilage has limited regenerative capacity, and injuries or damage to this tissue type often heal through the formation of scar tissue, which is composed of dense connective tissue rather than the original fibrocartilage structure.
The Main Ingredients of Cartilage
Cartilage, a specialized form of connective tissue, consists of various components that contribute to its structure and function. The main ingredients of cartilage include chondrocytes, chondroblasts, and the extracellular matrix.
Chondrocytes and chondroblasts are the primary cells responsible for the formation and maintenance of cartilage. Chondrocytes are mature cartilage cells that reside within cavities called lacunae within the cartilage matrix. They play a crucial role in maintaining the integrity and function of cartilage. Chondroblasts, on the other hand, are immature cartilage cells that actively produce and secrete the components of the extracellular matrix.
The extracellular matrix is a complex mixture of proteins, carbohydrates, and water that surrounds the chondrocytes. It provides structural support, flexibility, and resilience to cartilage. The matrix consists of collagen fibers, proteoglycans, and water.
Collagen fibers are the most abundant protein in cartilage and give it tensile strength. They provide a framework for the cartilage and contribute to its overall structure and durability. The type of collagen found in cartilage is mainly type II collagen, although other types, such as type IX and type XI collagen, are also present.
Proteoglycans are large molecules made up of proteins and carbohydrates. They are responsible for the gel-like consistency of the cartilage matrix. Proteoglycans consist of a protein core to which long chains of sugar molecules called glycosaminoglycans (GAGs) are attached. GAGs attract and hold water molecules, which helps to maintain the hydration and cushioning properties of cartilage.
Water is another essential component of cartilage. It occupies a significant portion of the extracellular matrix and provides lubrication and shock absorption properties to the tissue. Water content in cartilage can vary depending on factors such as age, health, and the specific type of cartilage.
In addition to chondrocytes, chondroblasts, collagen fibers, proteoglycans, and water, cartilage also contains a layer of connective tissue called the perichondrium. The perichondrium surrounds most cartilage sites and consists of two layers: an outer layer containing collagen-producing fibroblasts and an inner layer housing chondroblasts.
During development, cartilage serves as a precursor to bone. Ossification, or the process of bone formation, gradually replaces cartilage with bone. This process begins during embryonic life and continues into early childhood. Cartilage growth occurs through two mechanisms: interstitial growth and appositional growth. In interstitial growth, chondrocytes within the existing cartilage divide and produce more matrix. In appositional growth, chondroblasts in the perichondrium add fresh layers of matrix to the surface of existing cartilage.
Overall, the main ingredients of cartilage, including chondrocytes, chondroblasts, collagen fibers, proteoglycans, water, and the perichondrium, work together to provide cartilage with its unique properties of strength, flexibility, and resilience.
Chondroblasts
- Chondroblasts are a specialized type of cells involved in the formation and maintenance of cartilage. They play a crucial role in producing the elements of the extracellular matrix (ECM), which provides the structure and functionality to cartilage.
- During embryonic development, chondroblasts start their activity by secreting the initial components of the ECM. These components include hyaluronic acid, chondroitin sulfate, collagen fibers, and water. Hyaluronic acid and chondroitin sulfate are types of glycosaminoglycans (GAGs), which are large sugar molecules that help to attract and retain water, providing hydration and lubrication to the cartilage tissue. Collagen fibers, mainly type II collagen, are secreted by chondroblasts and form a network that gives cartilage its strength and structure.
- As chondroblasts continue to produce and secrete these ECM components, they become surrounded by the newly formed matrix. At this point, they become immobilized and undergo a change in their cellular state, transforming into chondrocytes. Chondrocytes are the mature, fully differentiated cells within the cartilage tissue. They reside within cavities called lacunae, which are spaces within the ECM.
- Once chondroblasts become chondrocytes, they continue to contribute to the maintenance and repair of cartilage. Although chondrocytes are no longer actively producing new ECM components, they are responsible for maintaining the balance between ECM synthesis and degradation. They monitor the integrity and quality of the cartilage tissue and can regulate the production of enzymes that break down the ECM when necessary for remodeling or repair processes.
- Chondrocytes also communicate with neighboring cells and respond to various signals in the surrounding environment. They can sense mechanical forces, such as compression or tension, and adjust their activity accordingly. This cellular responsiveness helps to maintain the structural integrity and functional properties of cartilage.
- It’s important to note that while chondroblasts primarily exist during the developmental stages and early growth, chondrocytes are the predominant cell type in mature cartilage. However, chondrocytes can revert to a more active state under certain conditions, such as injury or disease, and regain some characteristics of chondroblasts, including increased ECM production.
- In summary, chondroblasts are the active cells responsible for the initial formation of the extracellular matrix in cartilage. They produce hyaluronic acid, chondroitin sulfate, collagen fibers, and water, which contribute to the structure, hydration, and strength of the cartilage tissue. Once surrounded by the matrix, chondroblasts become chondrocytes and continue to maintain and regulate the ECM composition throughout the lifespan of the cartilage.
Chondrocytes
- Chondrocytes are a specialized type of cells that are derived from chondroblasts and play a crucial role in the maintenance and regulation of cartilage tissue. Once chondroblasts become surrounded by the matrix they produce, they transition into the immobile form known as chondrocytes. These cells are housed within cavities called lacunae, and each lacuna can contain one or more chondrocytes.
- The functions of chondrocytes vary depending on the type of cartilage in which they are located. In articular cartilage, which is found in the joints, chondrocytes contribute to the smooth movement and articulation of the joint. They help maintain the structural integrity and lubrication of the joint surface, which allows for pain-free movement and shock absorption.
- In growth plates, which are regions of cartilage located near the ends of long bones, chondrocytes play a critical role in regulating bone growth. They are responsible for the elongation and expansion of the bone during the growth phase of development. Chondrocytes in the growth plate undergo a process called proliferation and differentiation, leading to the production of new cartilage matrix and the subsequent conversion of cartilage to bone.
- While chondroblasts are primarily involved in the production of the extracellular matrix (ECM), chondrocytes are responsible for maintaining the existing ECM. They continuously monitor the quality and integrity of the cartilage tissue, ensuring its proper function and stability. Chondrocytes can sense mechanical forces and respond to changes in their environment by adjusting their activity and ECM production accordingly.
- Compared to chondroblasts, chondrocytes are a less active form of the same cell type. They have a lower metabolic rate and reduced capacity for ECM synthesis. However, chondrocytes can still exhibit some level of ECM production under certain conditions, such as during tissue repair or in response to pathological changes.
- In summary, chondrocytes are the mature and immobile form of chondroblasts. They reside within lacunae, enclosed by the matrix they produce. Chondrocytes have specific roles depending on the type of cartilage they are found in, such as facilitating joint articulation in articular cartilage and regulating bone growth in growth plates. While chondroblasts are primarily involved in ECM synthesis, chondrocytes maintain the existing ECM and ensure the proper functioning of the cartilage tissue.
Fibroblasts
- Fibroblasts are a type of cell found in various types of connective tissue, including cartilage. Their primary function is to synthesize and maintain the extracellular matrix (ECM) of the tissue.
- In cartilage, fibroblasts play an important role in producing type I collagen, which is the most abundant type of collagen in the human body. Type I collagen provides strength and structural support to tissues. While chondrocytes are the primary cells responsible for producing the ECM components in cartilage, fibroblasts contribute to the synthesis of type I collagen, which can be found in certain regions or circumstances within the cartilage tissue.
- Interestingly, fibroblasts have the ability to transform into chondrocytes under specific conditions. This process, known as fibroblast-to-chondrocyte transformation or chondrogenesis, occurs during certain stages of development or in response to tissue repair and regeneration. When exposed to specific signals and microenvironments, fibroblasts can undergo a series of molecular changes that lead to their differentiation into chondrocytes. This transformation allows fibroblasts to contribute to the formation and repair of cartilage tissue.
- The fibroblast-to-chondrocyte transformation involves changes in gene expression, cell morphology, and the production of ECM components specific to chondrocytes. Once transformed into chondrocytes, these cells can actively participate in the synthesis of cartilage-specific ECM molecules, such as type II collagen and proteoglycans, which are critical for the structural integrity and function of cartilage.
- It’s important to note that fibroblasts and chondrocytes are distinct cell types with different functions in cartilage. Fibroblasts primarily produce type I collagen and are not as abundant in mature cartilage as chondrocytes. Chondrocytes, on the other hand, are the specialized cells responsible for maintaining the cartilage matrix and regulating its homeostasis.
- In summary, fibroblasts are found in various connective tissues, including cartilage, where they contribute to the production of type I collagen. Under specific conditions, fibroblasts can transform into chondrocytes, allowing them to participate in the synthesis and maintenance of cartilage-specific ECM components. This fibroblast-to-chondrocyte transformation plays a significant role in cartilage development, repair, and regeneration processes.
Extracellular Matrix
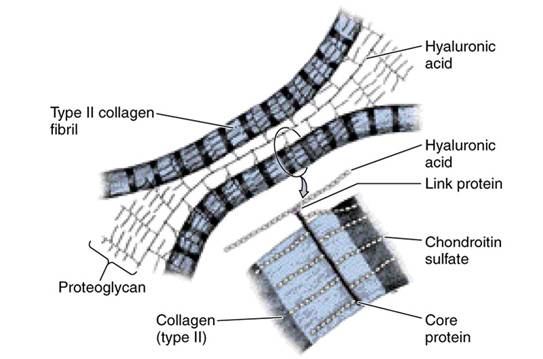
- The extracellular matrix (ECM) in cartilage is composed of three characteristic elements: collagen, proteoglycans, and noncollagenous proteins.
- There is a higher proportion of matrix compared to cells in cartilage due to the low oxygen environment and lack of vasculature, limiting cell numbers and metabolic activity.
- Cartilage tissue has little to no new growth, contributing to degenerative joint pain in the elderly, although slow growth can still occur, resulting in larger ears and noses in older individuals.
- Collagen is a protein-based matrix that provides form and strength to cartilage tissue. Type II collagen is the primary type found in cartilage, often accompanied by FACIT XIV collagen, which determines fiber diameter.
- Proteoglycans are large molecules in the ECM that bind with water, offering flexibility and cushioning. They bond to hyaluronic acid through link proteins, with Aggrecan (chondroitin sulphate proteoglycan 1) being a prominent example.
- Proteoglycans possess negative charges and a large surface area, allowing them to bind significant amounts of water. This creates high osmotic pressure, enhances load-bearing capacity, and contributes to the gel-like consistency of the ECM.
- Noncollagenous proteins, although fewer in number, are involved in maintaining and organizing the cartilage structure at a macromolecular level.
- The ECM provides structural integrity, mechanical support, flexibility, and cushioning to the cartilage tissue, playing a vital role in its normal functioning.
- Limited cell numbers and slow growth in cartilage contribute to its reduced regenerative capacity and susceptibility to degenerative conditions like osteoarthritis.
Function of Cartilage
- Supportive Framework: Cartilage provides a supportive framework for the walls of the airways, including the nose, trachea, larynx, and bronchi, preventing them from collapsing.
- Articular Surfaces: Cartilage forms the smooth articular surfaces of bones, allowing for frictionless movement and facilitating joint function.
- Template for Skeletal Development: During the embryonic stage, cartilage functions as a template for the majority of the skeleton. Hyaline cartilage serves as a precursor to bone formation and ossifies to form the fetal skeleton.
- Support and Precursor to Bone: Cartilage provides support in the embryo and serves as a precursor to bone formation through endochondral ossification.
- Facial Movement and Lightweight Support: Cartilage allows for facial movement and provides a lightweight supportive structure in the external ear, tip of the nose, and septum.
- Shock Absorption and Cushioning: Cartilage acts as a shock absorber, cushioning areas where bones meet, preventing abrasion, and reducing damage.
- Joint Function and Flexibility: Cartilage enables joints to move smoothly and flexibly. It allows bending and adjustment of bone positions relative to each other.
- Protection for Organs and Spinal Cord: Cartilage provides structure and protection for organs such as the ear and nose. It also protects the spinal cord and prevents bones from rubbing together.
- Cushioning for the Skeletal System: Cartilage provides cushioning for the skeletal system, helping to distribute forces and reduce impact on bones.
- Bone Repair: In bone repair, cartilage plays a role by providing a template for ossification, assisting in the healing of broken sections of bone.
- Joint Stability: Cartilage holds articular joints together, contributing to joint stability and preventing bones from rubbing against each other.
- Elastic Framework: Cartilage acts as an elastic framework, allowing bones to adjust their positions relative to one another and accommodating movements within the body.
Diseases Affecting Cartilage
- Chondrodystrophies: Group of diseases characterized by the disturbance of growth and ossification of cartilage.
- Osteoarthritis: Degenerative joint disease where the articular cartilage thins and wears away, leading to reduced motion and pain. It is commonly associated with “bone against bone” within the joint. Treatment options include joint replacement and symptom management.
- Traumatic Rupture or Detachment: Injury to the knee can damage the cartilage, specifically the meniscus, requiring knee cartilage replacement therapy.
- Achondroplasia: Genetic condition resulting in reduced proliferation of chondrocytes in the epiphyseal plate of long bones during infancy and childhood, leading to dwarfism.
- Costochondritis: Inflammation of the cartilage in the ribs, causing chest pain.
- Spinal Disc Herniation: Compression of an intervertebral disc leads to rupture and herniation, often resulting in back pain and compression of adjacent nerves.
- Relapsing Polychondritis: Autoimmune destruction of cartilage, primarily affecting the nose and ears, leading to disfiguration and potential respiratory complications.
- Cartilage Tumors: Tumors composed of cartilage tissue can be benign (chondroma) or malignant (chondrosarcoma), typically appearing in bones rather than pre-existing cartilage.
- Matrix as a Barrier: The cartilage matrix acts as a barrier, preventing the entry of lymphocytes and diffusion of immunoglobulins. This property allows for cartilage transplantation between individuals without tissue rejection concerns.
FAQ
What is cartilage?
Cartilage is a flexible connective tissue found in various parts of the body, including joints, ears, nose, and the respiratory system. It provides structural support, cushioning, and smooth articulation between bones.
What are the types of cartilage?
There are three main types of cartilage: hyaline cartilage, elastic cartilage, and fibrocartilage. Hyaline cartilage is the most common type, found in joints and the respiratory system. Elastic cartilage is present in the outer ear and epiglottis. Fibrocartilage is found in areas subjected to heavy pressure, such as the intervertebral discs and knee menisci.
How does cartilage differ from bone?
Cartilage is a type of connective tissue that is more flexible and avascular compared to bone. It is composed of cells called chondrocytes embedded in an extracellular matrix, while bone contains cells called osteocytes within a mineralized matrix. Cartilage lacks blood vessels and nerves, while bone has a rich vascular and nerve supply.
What is the function of cartilage?
Cartilage serves multiple functions, including providing a smooth surface for joint movement, absorbing shock, distributing load, and maintaining the shape and structure of body parts like the nose and ears.
Can cartilage repair itself?
Cartilage has limited regenerative capacity due to its avascular nature. While it can undergo some repair, the process is slow and often incomplete. Injuries to cartilage may require medical intervention for proper healing.
What causes cartilage damage?
Cartilage damage can result from traumatic injuries, such as sports-related impacts or accidents. It can also occur due to degenerative conditions like osteoarthritis, where the cartilage gradually wears away over time.
How is cartilage damage diagnosed?
Medical professionals may use various diagnostic methods to assess cartilage damage, including physical examination, imaging techniques like X-rays, MRI scans, and arthroscopy (a minimally invasive procedure that allows direct visualization of joint structures).
What are the treatment options for cartilage damage?
Treatment for cartilage damage depends on the extent and location of the injury. Options may include conservative measures like rest, physical therapy, pain management, or surgical interventions such as cartilage repair, transplantation, or joint replacement.
Can cartilage be replaced or regenerated?
Scientists are researching various methods to regenerate or replace damaged cartilage, including tissue engineering techniques, stem cell therapies, and the use of biomaterials. These approaches aim to enhance cartilage repair and restore its function.
How can I maintain healthy cartilage?
To promote cartilage health, it is essential to maintain a balanced diet rich in nutrients like vitamins C and D, engage in regular low-impact exercise to strengthen supporting muscles, avoid excessive stress on joints, and practice good posture. Additionally, maintaining a healthy weight can reduce the burden on weight-bearing joints.
References
- https://dhingcollegeonline.co.in/attendence/classnotes/files/1607191316.pdf
- https://classnotes123.com/differentiate-between-bone-and-cartilage-with-respect-to-structure-functions-and-location/
- https://biologydictionary.net/cartilage/#cartilage-function
- https://teachmephysiology.com/histology/tissue-structure/cartilage/
- https://www.kenhub.com/en/library/anatomy/cartilage
- https://infinitylearn.com/surge/biology/cartilage/


