Table of Contents
From shortly after birth to death, the skin and mucous membranes are home to a diverse microbial fauna. The average human body contains 1013 cells and harbors 1014 bacteria. This is the normal microbial population. The normal microbial fauna is stable. During certain times in a person’s life, specific genera may populate different body regions.
The normal flora microorganisms may help the host (by competing with pathogens like Salmonella spp. or by producing nutrients that the host can use), but they may also harm the host (by creating dental caries, abscesses or other infectious diseases), and may even exist as commensals (habiting the host long-term without causing any harm or benefit).
Although most elements of normal microbial life found on the skin, nails and eyes of humans are safe for healthy people, they can cause serious illness in those with compromised immune systems. Most investigators do not consider viruses and parasites to be part of the normal microbiological flora because they are not common and do not help the host.
What is Normal Human Microbiota/Normal Flora of Humans?
- The human microbiome is a collection of microbiota found in or on human tissues and biofluids. It also includes the anatomical locations where they reside. These include the skin, mammary and ovarian glands, lung, saliva and oral mucosas, conjunctiva and biliary tract.
- There are many types of microbiota in the human body, including bacteria, archaea and fungi as well as protists, viruses, and prototists.
- Although micro-animals are also able to live on the human body they are usually excluded from this definition.
- The term human microbiome can be used in genomics to describe the collective genomes of microorganisms. However, the term human mytagenome is the same.
- Many microorganisms colonize human cells, and they have approximately the same number of non-human cells that humans.
- Some microorganisms that colonize people are considered commensal. This means they co-exist with humans without harming them. Others have a mutualistic relationship to their human hosts.
- However, non-pathogenic microorganisms may cause harm to human hosts through the metabolites that they produce. Trimethylamine is one example. The human body then converts it via FMO3-mediated oxygenation to trimethylamine Noxide.
- Some microorganisms are useful for the human host. However, it is unclear what their role is. They are often referred to as normal flora and normal microbiota.
How Human get Normal Flora?
Many factors can influence the composition of the normal flora, such as genetics, age and sex, stress, nutrition, diet, and other lifestyle factors. The normal flora of the intestinal tract, oral cavity, or genitalia will be affected by three developmental changes: weaning, eruption, and cessation ovarian functions. The human bacterial flora is stable within these limits, so it’s possible to give a general description.
At the time of birth, the human is colonized by normal flora. The fetus is still sterile in utero. However, colonization begins when the mother’s milk breaks down and the birth process starts. After birth, the baby can be handled and fed in 48 hours. This will establish a normal flora on the skin and oral cavity.
A human adult has about 1012 bacteria in its skin, 1010 in its mouth and 1014 in its gastrointestinal tract. This number is much higher than the total number of eucaryotic cell in all tissues and organs that make up a human.
Types of Microorganisms found in the Human Body
Bacteria
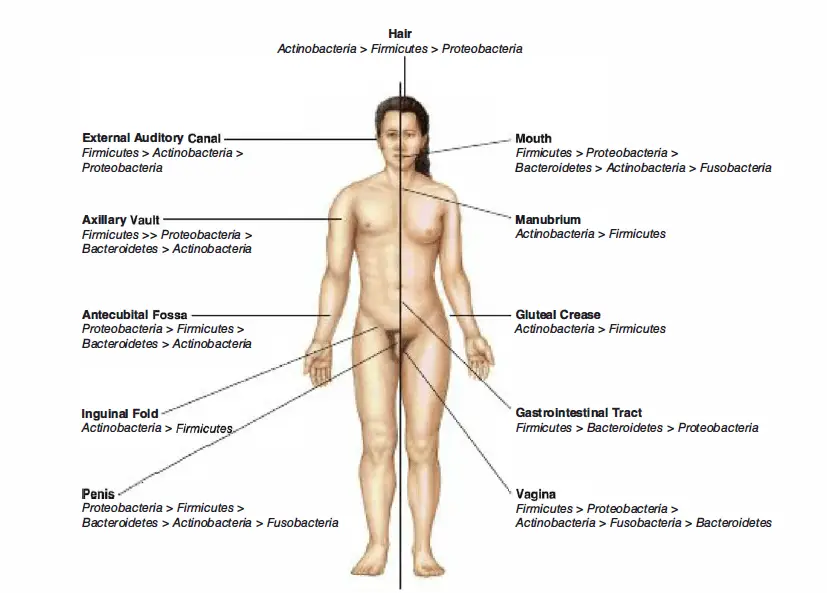
- Human Microbiome Project discovered that people have thousands of different bacterial types. Different body sites also have their own unique communities.
- The diversity of skin and genitalia sites was smaller than that of the mouth and gut. These areas showed the highest richness.
- There are many factors that can affect the bacterial makeup of a site on your body.
- Multiple subtypes of bacteria are found in the mouth. They prefer to live in distinct locations. Even enterotypes found in the human stomach, which were previously believed to be well-understood, come from a wide range of communities that have blurred taxon borders.
- There are 500-1000 species of bacteria that live in the human stomach, but they only belong to a handful of phyla. Firmicutes and Bacteroidetes dominate, but there are also Proteobacteria. Fusobacteria, Fusobacteria, Proteobacteria and Cyanobacteria.
- Many types of bacteria live in the mouth. They are part of a sticky substance called Plaque. Tooth decay is also caused by the same bacteria that secretes acids which dissolve tooth enamel.
- Most of the genitalia microflora is made up of different species. Although Lactobacillus acidophilus was thought to be the most prevalent of these species, it was later shown that L. iners was actually the most widespread, followed by L. crispyatus.
- L. gasseri, L. delbruekii, and L. jensenii are all lactobacilli that can be found in the genitalia. Infections such as candidiasis and bacterial vaginosis can result from disruptions in the genitalia flora.
Archaea
- Although archaea can be found in the human intestine, their numbers are smaller than the many bacteria species.
- The dominant group is the methanogens, especially Methanobrevibacter Smithii and Methanosphaera Stadtmanae.
- However, methanogen colonization is not always easy to detect. Only about half of all humans are able to detect these organisms.
- Although no archaeal pathogens have been identified as of 2007, some methanogens have been linked to periodontal disease.
Fungi
- The human gut is home to fungi, including yeasts.
- Candida species are the most studied of all because they can be pathogenic in immunocompromised patients and healthy hosts.
- Malassezia species of yeasts also live on the skin and consume oils from the sebaceous gills.
Viruses
- Many body sites are colonized by viruses, particularly bacterial viruses (bacteriophages). Colonized areas include the skin, [gut, lungs and oral cavity.
- Some diseases have been linked to virus communities, but they are not just bacterial communities.
Classification of Normal Human Microbiota/Normal Flora
There are present two types of Human microbiome/Normal Flora such as;
- Resident flora
- Transient flora
1. Residents flora
- It is composed of organisms that are frequently present in a specific area, and when disturbed they reestablish themselves like E.coli.
- Comonsals are microorganisms that live on human skin. The physiologic factors that influence their growth, such as temperature, humidity, and the presence or absence of certain nutrients or inhibitory substances, are key to their success.
Role of Resident Flora
- The role of the resident flora in certain areas is crucial for maintaining health and normal function.
- The intestinal flora helps in the absorption and synthesize of vitamin K.
- The resident flora on mucous membranes as well as skin may protect against colonization by pathogens.
- The environment and other parts of the body can fill the gap left by the normal flora. These organisms act as opportunists, and could become pathogens.
- However, some members of the normal flora can also produce disease and, if they are removed from their environment and allowed to enter the bloodstream or tissues, they may become pathogenic. Streptococci from the viridans group, the most common resident organisms in the upper respiratory tract, can be introduced into the bloodstream after tooth extractions or tonsillectomy. They may settle on prosthetic or deformed heart valves, causing infection. With minor trauma, such as dental scaling or vigorous brushing, small numbers may be present in the bloodstream.
- Bacteroides is the most common resident bacteria. If they are introduced into the peritoneal cavity free of other bacteria or the pelvic tissues as a result trauma, they can cause suppuration or bacteremia.
- There are many more examples. But the point is that microbes from the normal resident flora can be harmless and beneficial in their normal locations in the host.
- If they are introduced in large numbers to foreign countries and predisposing factors exist, they could cause disease.
Advantages of Resident Flora
- They stop or suppress the entry pathogens.
- They synthesize vitamins, including Vit.-K as well as several B Group vitamins.
- Antibodies are produced by normal flora. These Antibodies can cross react with pathogens that have similar or shared antigens. This raises the immunity status of the host to the invading disease.
- Some pathogens can be affected by colonies caused by normal flora organisms.
- Endotoxins may be released by natural flora to aid the body’s defense mechanisms.
Disadvantages of resident flora
- They can become pathogenic if the immunity is lower.
- They could be pathogens in other issues (other than their usual habitat). Urinary tract infection (UTI) may be caused by normal intestinal flora.
- Because of their presence in the body and similarity to pathogens, normal flora can cause confusion when diagnosing.
2. Transient flora
- It is composed of non-pathogenic as well as potentially pathogenic bacteria.
- They can be removed by mechanical means such as Pneumococcus or Meningococcus.
- The host includes members of the normal flora, such as saprophytes and commensals, as well as facultative pathogens, true pathogens, and even some pathogens.
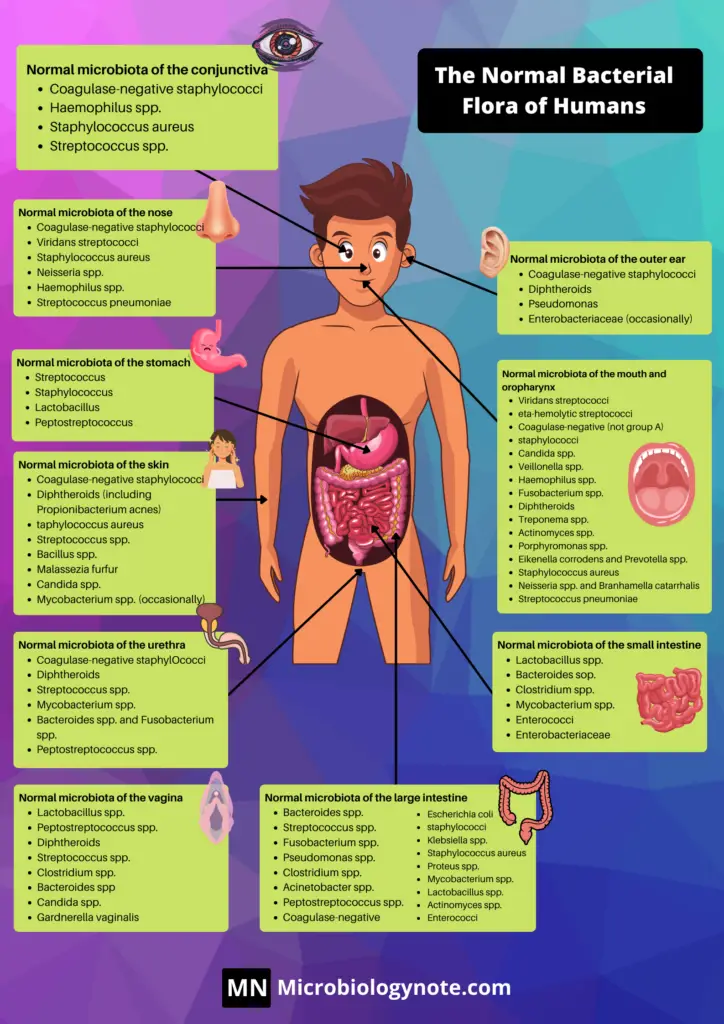
A. Normal Flora of the Skin
- The skin is constantly in contact with and exposed to the environment. This makes it more likely for the skin to harbor transient microorganisms.
- Anaerobic and aerobic diphtheroid bacteriailli are the predominant microorganisms in the skin.
- An adult human’s skin area is approximately 2 meters. Anatomical location can affect the composition and density of the skin’s normal flora.
- For the removal of non-resident microorganisms, it is important to have a low pH and fatty acids in your skin secretions.
- Normal skin is found in 102-104 organisms/sq. cm.
- The sweat glands contain most of the bacteria found on the skin.
- Gram-positive cocci are skin microbes that can be found in the epidermis’ superficial layers and upper hair follicles. (Staphylococcus epidermidis, Micrococcus. Corynebacteria like Propionibacterium.
- They are nonpathogenic and generally considered commensal. However, they have been given mutualistic and parasitic roles. Staphylococci, propionibacteria and others produce fatty acids that prevent the growth of yeast and fungi on the skin. Propionibacterium acnes can become trapped in the hair follicle and cause inflammation and even acne.
- Individuals who have nasal carriers may find potentially dangerous Staphylococcus Aureus on their hands and faces. Because the bacteria can infect the nasal membranes, the hands and face are susceptible to being inoculated. These individuals could inoculate themselves with the bacteria or spread it to others.
- Staph.epidermidis, Diphtheroids and Diphtheroids can be found on the skin’s surface. Peptococcus and Strept.viridens are less common.
B. Normal flora of Conjunctiva
- Although a variety of bacteria can be grown from normal conjunctivas, the numbers of organisms are usually very small.
- Staphylococcus epidermidis, certain coryneforms (“Propionibacterium acnes”) are the dominant. Staphylococcus aureus, some streptococci, Haemophilus sp. Neisseria species. Occasionally, they are found.
- Continuous secretion from the lachrymal cells keeps the conjunctiva moist and healthy.
- Every few seconds, blinking cleans the conjunctiva mechanically washing out foreign objects and bacteria.
- Lysozyme and lachrymal secretions (tears), also contain bactericidal compounds.
- Without special mechanisms for attachment to epithelial surfaces or the ability to resist attack by Lysozyme, there is very little chance that microorganisms can colonize the conjunctiva.
- Pathogens that infect the conjunctiva include Neisseria gonorrhoeae and Chlamydia trachomatis. Neisseria gonorrhoeae or Chlamydia transdermalis are believed to be capable of attaching to the conjunctival epithelium.
- Babies born after birth may be more susceptible to bacterial attachment. To prevent infection, silver nitrate and antibiotics may be administered to the newborn after the birth canal has passed.
C. Normal Flora of the Respiratory Tract
- Numerous bacterial species are found in the upper respiratory tract (nasopharynx).
- The nares (or nostrils) are constantly heavily colonized with Staphylococcus epidermidis, corynebacteria, but also, in about 20% of the population, with Staphylococcus Aureus. This is the main carrier site for this important pathogen.
- Healthy sinuses are, however, sterile.
- Streptococci and other Gram-negative cocci are common in the pharynx (throat).
- Sometimes, pathogens like Streptococcus pneumoniae or Streptococcus pseudogenes, Haemophilus Influenzae and Neisseria meningitidis can colonize the pharynx.
- Because of the effective cleansing action of ciliated epithelium, which line the tract, the lower respiratory tract (trachea and bronchi) is almost free from microorganisms.
- Any bacteria that reaches the lower respiratory tract is swept up by the action mucociliary blanket. This blanket lines the bronchi and can be removed by coughing, sneezing or swallowing.
- The respiratory tract epithelium can become damaged in cases of bronchitis and viral pneumonia. This could make the person more susceptible to infection with pathogens like H. influenzae and S. pneumoniae.
D. Normal Flora of the Urogenital Tract
- The normal sterility of urine is due to the fact that it is flushed with urine once every several hours. This makes it difficult for microorganisms to gain access and establish themselves.
- According to urine cultures, the flora in the anterior urethra suggests that it may be home to a consistent normal flora including Enterococcus foecalis, Staphylococcus epidermidis and some alpha-hemolytic streptococci. However, they are few and far between. Some enteric bacteria, such as E. coli and Proteus, may also be found in the uterus. Some enteric bacteria (e.g. E.coli, Proteus, and Corynebacteria) may be found in the anterior urethra.
- Soon after birth, the genitalia is colonized with corynebacteria (Staphylococci), streptococci and E.coli.
- The genitalia epithelium is a reservoir of glycogen that is produced by circulating estrogens during reproductive life.
- Doderlein’s Bacillus is dominant, and can metabolize glycogen to lactate.
- All other bacteria, except for this lactobacillus, are not able to colonize due to the lactic acid and other metabolic products. The resulting low pH of the genitalia epithelium prevents establishment by most other bacteria as well as the potentially-pathogenic yeast, Candida albicans. This is an excellent example of the protective effects of normal bacterial flora on their human hosts.
E. Normal Flora of the Oral Cavity
- The mouth is a good place for many bacteria because it contains nutrients, epithelial matter, and secretions.
- Streptococci and lactobacilli are oral bacteria. There is also a large number of anaerobes including bacteroides.
- With age comes a series of ecological situations at the mouth, which corresponds to changes in the normal flora.
- The oral cavity at birth is made up of only the soft tissues of the mouth, cheeks, tongue, and palate. These tissues are kept moist through the secretions from the salivary glands.
- The oral cavity at birth is sterile, but quickly colonizes from the environment. This is especially true for the mother during the first feeding.
- Streptococcus salivarius, which is the dominant species, may account for 98% of total oral flora up to the appearance of teeth (6 – 9 month in humans).
- Colonization by S. sanguis and S. mutans can be initiated when the teeth are first erupted. To colonize, these bacteria need a nondesquamating (nonepithelial), surface. They will survive as long as there are teeth.
- Other strains are more firmly attached to the cheeks and gums, but not the teeth.
- The habitat for anaerobic species is enhanced by the creation of the gingival crevice (supporting structures for the teeth).
- As the population ages, the complexity of oral flora increases. In particular, bacteroides as well as spirochetes are more common around puberty.
- The host provides nutrients and habitat, which clearly benefits the normal bacterial flora in the oral cavity. The host may also benefit.
- Normal flora tends to occupy colonization sites, making it harder for non-indigenous microorganisms to establish themselves.
- The oral flora also contributes to host nutrition by synthesising vitamins and immunity by inducing low levels secretory and circulating antibodies that could cross-react with pathogens.
- The oral bacteria also exerts microbial antagonism by producing inhibitory substances, such as peroxides, fatty acids and bacteriocins, against nonindigenous organisms.
- However, oral flora is the most common cause of many oral diseases in humans. This includes abscesses and gingivitis as well as dental caries and periodontal disease.
- Abscesses can occur in the brain, lung, and alveolar bones if oral bacteria is allowed to enter deeper tissues. These infections are usually caused by a mixture of bacteria, with Bacteroides melaninogenicus playing a predominant role.
- Oral streptococci can be introduced to wounds caused by dental treatment or manipulation. They may attach to the heart valves and cause subacute bacterial infection.
F. Normal Flora of the Gastrointestinal Tract
- More extensive research has been done on the bacteria in the GI tract of animals than any other location.
- There are differences in the composition of different animal species and within an animal specie.
- There are many factors that influence the composition of the flora in humans. These include age, diet, culture, and antibiotic use. This can greatly alter the composition of the intestinal fauna.
- Adult humans have only bacteria in their upper GI tract. Due to the acidity of the gastric juices, only a small number of bacteria (mainly acid-tolerant Lactobacilli), can be cultured from normal stomach.
- The proximal small intestinale is home to a very sparse Gram positive flora. It consists mainly of Enterococcus foecalis and lactobacilli. The fluid in this region contains approximately 105-107 bacteria.
- The distal portion of the small intestine has higher levels of bacteria (108/ml), and more species including coliforms (E. coli, relatives) and Bacteroides in addition to lactobacilli, enterococci, and coliforms.
- The flora found in the colon (large intestine) is qualitatively identical to that found within feces.
- The colon has a population of bacteria that can reach levels of 1011/ml of feces.
- Coliforms are more common, and although enterococci and clostridia can be found frequently, the dominant species are anaerobic Bacteroides (Bifidobacterium biifidum).
- These organisms could outnumber E. coli in the range of 1,000:1 to 10,000. Sometimes large numbers of anaerobic and methanogens, up to 1010/gm, may be found in the colon of human beings.
How Gastrointestinal Tract gets its Normal Flora
The entire intestinal tract at birth is sterile. However, bacteria can enter the infant’s system through the first food. The infant’s food source will determine the initial colonizing bacteria. Breast-fed infants have more than 90% of total intestinal bacteria. Enterobacteriaceae, enterococci, and staphylococci are both present in small amounts, but they are often found. Clostridium, bacteroides and staphylococci are virtually absent.
Bifidobacteria is not prevalent in bottle-fed infants. Breast-fed infants can be switched to cow’s milk, solid food or a diet that includes bifidobacteria. The bifidobacteria will then become more common with enterics, bacteria, enterococci lactobacilli, bacteroides and clostridium. Human milk apparently contains a growth factor which enriches for the growth of bifidobacteria. These bacteria also play an important role in preventing colonization by non-indigenous or pathogenic species.
Composition of Gastrointestinal Tract Normal Flora
- The composition of the flora in the gastrointestinal tract is variable along the tract (at the longitudinal levels) as well as across the tract at the horizontal levels. This is where bacteria attaches to the epithelium, while others are found in the lumen.
- It is common to see a close association between certain bacteria in the intestinal ecosystem, and specific cells or tissues (evidence for tissue tropism or specific adherence).
- Gram-positive bacteria such as streptococci or lactobacilli are believed to stick to the gastrointestinal epithelium by attaching to certain receptors on epithelial cells.
- Gram-negative bacteria, such as enterics, may attach to epithelial cells by binding to specific fimbriae.
Role of Gastrointestinal Tract Normal Flora
The intestinal tract is where we see the most impact of the bacterial flora upon their host. Because of their high mass and large numbers, this is why they are so effective at affecting the host. The presence of bacteria in the human GI tract has been shown to increase vitamin production and contribute to nutrition and digestion. Their most important effects include their ability protect the host against infection and to stimulate the growth and activity of immunological tissues.
Some bacteria found in the colon, such as Bacteroides, can cause cancer. Bacteroides have been shown to produce carcinogenic metabolites, which may increase the risk of colon cancer. Poor nutrition and antibiotic-induced changes in the GI flora can lead to shifts in population and colonization by nonresidents, which can then lead to gastrointestinal disease.
Beneficial Effects of the Normal Flora/Advantages of Normal Flora
Microbiologists have made experimental comparisons of “germ-free”, which are animals that aren’t colonized by microbes, and “normal flora” animals. These experiments show the effects of normal flora on conventional animals. A lack of exposure to normal flora is thought to cause some characteristics in germ-free animals, including vitamin deficiencies, particularly vitamin K, and vitamin B12, an increased susceptibility for infectious disease, a weak immune system, and a lack of natural antibodies or natural immunity to bacterial infections.
Beneficial Effects are;
- Normal flora can synthesize and excrete vitamins that are more than their needs. These vitamins can then be absorbed by the host as nutrients. Enteric bacteria in humans produces Vitamin K and Vitamin B12 while lactic acid bacteria makes certain B-vitamins. Vitamin K may not be available in sufficient quantities for animals that are sterile.
- Normal flora can prevent pathogens from colonizing by competing for nutrients or attachment sites. This is their most important benefit, as it has been shown in the oral cavity and the intestine as well the skin and genitalia epithelium. Infected animals that are not contaminated by germs can infected with 10 Salmonella bacteria. The infectious dose for animals that are contaminated with the bacteria is close to 106 cells.
- Normal flora can antagonize bacteria by producing substances that inhibit or kill non-indigenous species. There are many substances produced by intestinal bacteria, ranging from non-specific fatty acids and peroxides up to highly specific bacteriocins that inhibit or kill other bacteria.
- Normal flora can stimulate certain tissues development in the GI tract, such as the caecum or certain lymphatic tissues (Peyer’s patches). The caecum in germ-free animals has a thicker, thinner-walled and more fluid-filled structure than that of conventional animals. Based on their ability to receive immunological stimulation, germ-free animals’ intestinal lymphatic tissues are less developed than those of conventional animals.
- Natural antibodies are produced by normal flora. The normal flora act as antigens in animals, triggering an immune response, including an antibody-mediated immune response (AMI). Antibodies produced against normal flora can cross-react with pathogens and prevent invasion or infection. Natural antibodies are antibodies that are produced against the antigenic components in the normal flora. These antibodies are not found in germ-free animals.
Harmful Effects of the Normal Flora
The following are some examples of harmful effects from the normal flora. Some of these effects have been observed in studies using germ-free animals. The effects of the normal flora on humans are not significant, except for two.
- Bacterial collaboration between a member the normal flora or a potential pathogen. This is when one organism helps another organism grow or survive. Examples of this include a member from the normal flora providing a vitamin or other growth factor to a pathogen in order for them to grow. Cross-feeding is a common practice among microbes. Another example of synergism is when “staph protected infections” are treated. This happens when a penicillin resistant staphylococcus, which is part of normal flora, shares its drug resistance avec pathogens that would otherwise be susceptible to the drug.
- Competitor for nutrients Bacteria must absorb nutrients from the host to meet their own nutritional needs. They convert them into other metabolisable substances, but some nutrients may be lost to their host. Animals that are sterile have been shown to grow faster and more efficiently than those with germs. The reason antibiotics are added to the diet of poultry, cows, and swine is that they grow faster and can be sold earlier. This practice can lead to the spread and development of antibiotic resistance in farm animals as well as humans.
- Induction of low-grade toxemia. Minute amounts of bacterial toxic substances (e.g. The circulation may contain small amounts of bacterial toxins (e.g. endotoxin). These small amounts of bacterial antibiotics stimulate the formation natural antibodies.
- Normal flora could be agents of disease. Endogenous disease can be caused by members of the normal flora if they get into a tissue or site that is not controlled or tolerated. Disease can result from many of the normal flora, which may include members of the normal flora that have gained access to compromised tissues.
- Transfer to susceptible hosts. Some pathogens that infect humans are also members of the normal flora and can be transferred to others. This includes pathogens in the upper respiratory tract, such as Streptococcus pneumoniae and Neisseria meningitidis.
Associations Between Humans and the Normal Flora
- E. Coli is the most well-known bacteria that frequently associates with humans. It is an invariably present component of the human digestive tract.
- Although E. E. coli is among the most researched of all organisms, and even though we have the exact place and the sequence of 488 genes that make up its genome, we do not know the full extent of its ecological interaction with humans.
- In reality, little is available about human-human interactions and their flora however, it is believed that they be active interactions and not interactions that are based on mutual disinterest.
- Both bacteria and hosts are believed to benefit from one another and these associations are mostly mutualistic.
- The normal flora receive from their host a continuous intake of nutrients and a stable environment and also protection and transportation. The host gains from normal flora nutrition as well as digestive advantages, a boost of the growth and development of the immune system and defense against infection and colonization from pathogenic microbes.
- While the majority of the activities of normal flora are beneficial to their hosts, some of the flora that are normal (live at the cost for their hosts) while some are pathogenic (capable to cause diseases).
- The causes of diseases that arise from the normal flora of their hosts could be referred to as endogenous illnesses.
- Most bacterial infections that are endogenous are opportunistic diseases, which means that the organism has to have a specific opportunity to weaken or fall within the host’s defenses to be able to be infected. One example of an opportunistic illness is chronic bronchitis for smokers in which normal flora bacteria can be able to enter the weak lung.
- Sometimes, the connection between a part of the normal flora and its host is difficult to decipher. This type of relationship where there is no obvious gain or harm to both organisms during their relationship is known as an acomensal relationship.
- A lot from the natural flora species that aren’t prevalent in their natural habitats, they are present in small quantities, are thought of being commensal.
- If, however, a presumptive relation between two individuals is investigated more deeply it is possible that mutualistic or parasitic characteristics are often observed.
Tissue specificity
- The majority of bacteria in the normal flora tend to infect specific tissues but not others.
- It is believed that this “tissue specificity” is usually due to the properties of the bacteria and the host. In general, specific bacteria are able to colonize specific tissues using one or more of these methods.
Tissue tropism
- Tissue tropism refers to the predisposition of bacteria of certain tissues to grow.
- One theory for the phenomenon of tissue tropism can be that the host supplies crucial nutrition and factors for growth to the bacterium as well as oxygen pH, temperature, and oxygen to allow growth.
Specific adherence
- The majority of bacteria are able to colonize the specific site or tissue because they are able to adhere to the site or tissue in a certain way which involves interaction between their two surfaces.
- Specific adhesion involves biochemical interactions between surface components of bacterial (ligands and adhesins) and molecular receptors on host cells.
- The bacterial components that make up adhesins are the molecular components of the capsules of their fimbriae or cell walls.
- Human tissues or cells are typically glycoprotein molecules that are located on the host cell’s or the surface of the tissue.
| Bacterium | Bacterial adhesin | Attachment site |
| Streptococcus pyogenes | Cell-bound protein (M-protein) | Pharyngeal epithelium |
| Streptococcus mutans | Cell- bound protein (Glycosyl transferase) | Pellicle of tooth |
| Streptococcus salivarius | Lipoteichoic acid | Buccal epithelium of tongue |
| Streptococcus pneumoniae | Cell-bound protein (choline-binding protein) | Mucosal epithelium |
| Staphylococcus aureus | Cell-bound protein | Mucosal epithelium |
| Neisseria gonorrhoeae | N-methylphenyl- alanine pili | Urethral/cervical epithelium |
| Enterotoxigenic E. coli | Type-1 fimbriae | Intestinal epithelium |
| Uropathogenic E. coli | P-pili (pap) | Upper urinary tract |
| Bordetella pertussis | Fimbriae (“filamentous hemagglutinin”) | Respiratory epithelium |
| Vibrio cholerae | N-methylphenylalanine pili | Intestinal epithelium |
| Treponema pallidum | Peptide in outer membrane | Mucosal epithelium |
| Mycoplasma | Membrane protein | Respiratory epithelium |
| Chlamydia | Unknown | Conjunctival or urethral epithelium |
Biofilm formation
- Certain indigenous bacteria can build biofilms on the tissue surface or are able to infiltrate the biofilm created by a different bacterial species.
- Biofilms can be a mix of microbes. One microbe is responsible for maintaining the biofilm, and it could be dominant.
- The biofilm of the classic type that includes elements that comprise the normal flora that inhabits dental cavities is development by dental plaque teeth.
- Plaque is a naturally-constructed biofilm, in which the consortia of bacteria may reach a thickness of 300-500 cells on the surfaces of the teeth. These buildups expose the teeth and the gingival tissues to high levels of bacterial metabolites. These cause dental diseases.
Disease carried out by the normal bacterial flora
The most frequent and economically-important condition in humans resulting from interactions with our normal flora is probably dental caries. Dental caries, dental plaque gingivitis, periodontal disease and gingivitis are the result of actions that are initiated that are carried out by normal bacteria flora.
1. Dental plaque
- Plaque on the teeth, or dental the substance that adheres to teeth comprises bacteria (60-70 percent that make up the plaque) and salivary polymers and bacterial extracellular substances.
- Plaque is a naturally-constructed biofilm, in which the consortia of bacteria may reach a thickness of 300-500 cells on the surfaces of the teeth. These deposits expose the gingival tissues and the teeth to high levels of bacterial metabolites that can cause dental problems.
- The predominant bacterial species that cause dental plaque is Streptococcus singuis and Streptococcus mutans. Both of which are thought to be to be the primary cause of plaque.
- The formation of plaque is triggered by the weak attachment of Streptococcal cells with salivary glycoproteins, forming one that is located on teeth. This is followed by more secure attachment through extracellular sticky polymers made of glucose (glucans) that are made by bacteria from food sugars (principally sucrose).
- A surface of the cells from Streptococcus mutans, glycosyl Transferase is responsible for the initial attachment of bacteria cells to the tooth’s surface. Additionally, it aids in the conversion of sucrose into the dextran polymers (glucans) that form plaque.
2. Dental Caries
The cause of dental Caries causes the breakdown of dentin, enamel or cementum of the teeth due to the bacterial activity. Caries start by direct desineralization of the enamel of teeth caused by the lactic acid as well as other organic acids that build up in the dental plaque. The lactic acid bacteria that live in the plaque make lactic acid through fermenting sugars and other carbs within the food of the patient. Streptococcus Mutans and Streptococcus sanguis are the most frequently have been linked to the development of dental caries, however other bacteria that produce lactic acid are likely involved too. The organisms typically colonize the occlusal fissures as well as contacts between teeth. This is in line with the amount of decay that occurs on these surfaces.
Streptococcus Mutans, in particular, is characterized by a variety of biochemical and physiological characteristics that are implicated in the development in the development of oral caries.
- It is a common element of the normal oral flora and fauna of humans that is found in large quantities. It easily colonizes the surfaces of teeth and salivary components (mucins glycoproteins) create a thin film on the tooth known as the enamel pellicle. Mucins that are adsorbed have been thought to act as molecular receptors to molecules on the cell surface of the bacterial.
- It’s a cell-bound protein glycosyl transferase that functions as an adhesin that binds to the tooth as well to polymerize sugars into glucans , which leads in the development of plaque.
- It creates lactic acid through the consumption of carbohydrate in diets that reduces the enamel of teeth. S. Mutans is a major producer of acid than other streptococci.
- It stores polysaccharides that are made from sugars in the diet that are used as reserve carbon sources and energy sources for production of the acid lactic. The extracellular glucans produced by S. Mutans are in reality, capsular bacterial polysaccharides which function as carbohydrates reserves. They also produce intracellular polysaccharides made from sugars, which are stored inside cells, and later metabolized into the acid lactic.
Streptococcus Mutans is believed to play a role in the onset of dental caries since it causes an infection of the surfaces of teeth plaque formation, as well as localized desineralization of the tooth’s enamel. However, it isn’t the sole reason for dental decay. Following the initial weakening of enamel different oral bacteria can get access to inside the tooth. Lactobacilli and Actinomyces as well as diverse proteolytic bacteria are typically present in human carious dental cementum and dentin. This indicates that these are second invaders and help in the progression of lesions.
3. Periodontal Diseases
- Periodontal diseases are bacterial infections that impact teeth’s supporting structure teeth (gingiva cementum, alveolar bone and the periodontal membrane).
- The most frequent type, gingivitis, is an inflammation condition that affects the gums. It is caused by accumulations of bacterial plaque within the gums.
- The increased population of Actinomyces has been observed, and have been suggested to be the reason.
- Conditions that are restricted to the gums typically don’t cause tooth loss however, there are more serious forms of diseases that affect the periodontal membrane and alveolar bone that can cause tooth loss.
- Bacteria present in the lesions is extremely complex, consisting of Gram-positive organisms (including streptococci and actinomyces) in addition to Gram-negative bacteria (including Spirochetes and Bacteroides).
- The mechanisms behind the destruction of tissues in periodontal diseases aren’t well-defined, but endotoxins, hydrolytic enzymes as well as other toxic bacteria metabolites of bacterial origin appear to be the culprits.
References
- https://nios.ac.in/media/documents/dmlt/Microbiology/Lesson-07.pdf
- http://www.textbookofbacteriology.net/normalflora_3.html
- https://www.researchgate.net/publication/282362814_The_Human_Microbiota_Composition_Functions_and_Therapeutic_Potential
- https://www.slideshare.net/doctorrao/normal-human-flora
- https://en.wikipedia.org/wiki/Human_microbiome
- file:///D:/Blog%20Image/J.ENG.2017.01.008.pdf
- https://www.ncbi.nlm.nih.gov/books/NBK7617/
- The Human Microbiota in Health and Disease, Baohong Wang, Mingfei Yao, Longxian Lv, Zongxin Ling, Lanjuan Li* http://dx.doi.org/10.1016/J.ENG.2017.01.008
MCQ related to Normal Microbiota
Which statement regarding normal microbiota of the human respiratory system is FALSE?
a. The upper respiratory tract is mostly sterile.(Ans)
b. The ciliary escalator in the bronchial tubes keeps the lower respiratory tract nearly sterile.
c. Potentially pathogenic microorganisms are present in nonsterile portions of the respiratory tract but usually do not cause disease.
d. The trachea normally may contain a few bacteria.
Which of the following is NOT caused by infection of the upper respiratory tract?
a. diphtheria
b. scarlet fever
c. streptococcal pharyngitis
d. whooping cough(Ans)
Which of the following situations is NOT a way in which a baby acquires normal microbiota?
a. microbes cross the placenta during pregnancy.(Ans)
b. microorganisms grow in the respiratory tract after the baby’s first breath.
c. microbes enter the nose and mouth when the baby is in the birth canal.
d. The baby acquires the residential microbiota in the colon after the first meal.
Which of the following situations might cause normal microbiota to become opportunistic pathogens?
treatment of a cancer patient with radiation
Which statement regarding normal microbiota of the urinary and reproductive systems is true?
a. Normal urine has a high level of normal, nonpathogenic microbes.
b. Pregnancy and menopause are associated with higher rates of urinary tract infections. (Ans)
c. Candida albicans is the predominant bacterium in the genitalia.
d. The male urethra is usually highly contaminated with microbes.
Women and men typically have the same normal microbiota in their reproductive systems.
a. True
b. False (Ans)
Normal microbiota provide protection from infection in each of the following ways EXCEPT
A) they produce antibacterial chemicals.
B) they compete with pathogens for nutrients.
C) they make the chemical environment unsuitable for nonresident bacteria.
D) they produce lysozyme.(Ans)
E) they change the pH of the environment.
Which of the following would NOT be a likely member of the normal microbiota of the skin surface?
a. obligate anaerobe (Ans)
b. lipophile
c. acidophile
d. halophile
Microorganisms that are members of the normal microbiota are also known to cause disease.
a. True (Ans)
b. False
Normal microbiota may cause disease if they are introduced into an unusual site in the body.
a. True (Ans)
b. False
Which statement about protective mechanisms employed by normal microbiota is false?
a. Normal microbiota consume nutrients.
b. Normal microbiota stimulate the second line of defense.
c. Normal microbiota spreading to locations where they are not normally found to prevent colonization from pathogens. (Ans)
d. Normal microbiota alter the pH of their environment.
How do normal microbiota and transient microbiota differ
Normal microbiota is always present on or in the body. Transient microbiota is not always present and most of the time is pathogenic.
Under normal circumstances, the microbiota of the skin is kept in check by
A. a pH above 8.
B. a slightly acidic pH. (Ans)
C. phagocytic activity.
D. excessive moisture.
All of the following are normal microbiota of the skin except
A) Streptococcus.(Ans)
B) Micrococcus.
C) Staphylococcus.
Which of the following can result when antibiotic therapy disrupts the normal microbiota?
A) anaphylactic shock
B) black hairy tongue
C) pseudomembranous colitis
D) both pseudomembranous colitis and thrush (Ans)
Why is Mannitol salt agar used as a selective medium for normal skin microbiota?
Mannitol salt agar is used as a selective medium for normal skin microbiota because most bacteria on the skin are salt-tolerated and will grow on an MSA plate.
Normal microbiota are typically found in and on all the following body locations except the
Blood (ans)
Normal microbiota may cause disease if conditions change in the body.
a. true (ans)
b. false
Most of the normal microbiota of the digestive system are found in the
a. large intestine (Ans)
b. mouth
c. small intestine
d. stomach
e. stomach and small intestine
Normal microbiota of the adult genitalia consist primarily of
A) Lactobacillus. (Ans)
B) Streptococcus.
C) Mycobacterium.
D) Neisseria.
E) Candida.
Which statement correctly describes the normal microbiota of the skin?
a. The skin’s normal microbiota are capable of growth at elevated salt concentrations. (Ans)
b. Most microorganisms that grow on the skin are sensitive to drying.
c. Vigorous washing will eliminate all skin bacteria.
d. On superficial skin surfaces, certain anaerobic bacteria produce fatty acids from oil gland secretions.
Normal microbiota play a number of essential roles, including:
Preventing disease by competing with disease causing microbes, helping degrade foods that would otherwise be indigestible, promoting immune system development and causing disease.
Is there Normal Microbiota present in the Lower respiratory system?
Typically there are no microorganisms present.
which of these would NOT describe characteristics of the normal microbiota of the skin?
a. gram-negative (Ans)
b. gram-positive
which is not a characteristic of the normal microbiota?
a. are often called the normal flora
b. live within our bodies
c. live on our bodies
d. may benefit the human host
e. regularly associated with disease symptoms (Ans)
Normal skin microbiota are able to grow on the skin because they can thrive in the presence of
A) sebum.
B) salt.
C) keratin.
D) sebum and salt. (Ans)
E) sebum, salt, and keratin.
Normal microbiota provide protection from infection in each of the following ways EXCEPT
A) they produce antibacterial chemicals.
B) they compete with pathogens for nutrients.
C) they make the chemical environment unsuitable for nonresident bacteria.
D) they produce lysozyme. (Ans)
E) they change the pH of the environment
Normal microbiota helps to __ colonization of pathogenic organisms.
-accelerate
-maintain
-prevent (Ans)
-promote
Both human pathogens and normal microbiota are typically classified as:
a. mesophiles (Ans)
b. psychrophiles
c. thermophiles
d. hyperthermophiles
Which of the following is true about the normal microbiota of the nervous system?
A) Only transient microbiota are present.
B) There are no normal microbiota. (Ans)
C) Normal microbiota are present in the central nervous system only.
D) Normal microbiota are present in the peripheral nervous system only.
E) None of the above.
Normal skin microbiota are able to grow on the skin because of their resistance to:
-sebum, salt, and keratin.
-sebum and salt. (Ans)
-salt.
-sebum.
-keratin.
