Table of Contents
What are Platelets (Thrombocytes)?
- Platelets, also known as thrombocytes, are blood components that play a vital part in hemostasis, or the process of halting bleeding when blood arteries are broken. Platelets are anucleated cells, which means they lack a nucleus, and are formed from megakaryocytic cells in the bone marrow. They are the second most numerous cells in the bloodstream, with concentrations ranging from 150-400 × 10^9/L.
- Platelets are most known for their role in blood clotting, but they also have non-hemostatic immunological roles. Platelets release a number of inflammatory mediators when triggered, making them a component of the innate immune response. Platelets can also function as effector cells by interacting with pathogens such as bacteria, viruses, fungi, and protozoans. Platelets release chemicals that attract macrophages, lymphocytes, and other immune cells, aiding in immunological responses.
- Platelets’ principal role is to induce blood coagulation. Platelets are typically in a dynamic state, ready to respond to any injury to blood vessels. Some platelets, however, remain dormant until a vessel is injured. Platelets are also involved in adaptive immune responses because they exhibit a variety of immunological receptors that can interact with immune cells such as vascular endothelial cells.
- Platelets do not have a nucleus, however they do contain nucleic acids such as mitochondrial DNA and RNA. They also have granules in their cytoplasm that can release numerous mediators when activated via exocytosis. Platelets share key traits with immune cells due to these qualities and their ability to interact with immune cells.
- Platelets, also known as thrombocytes, are only found in mammals; other animals, such as birds and amphibians, contain circulating intact mononuclear cells known as thrombocytes. Platelets are responsible in animals for clumping together in reaction to bleeding from blood vessel damage, resulting in the development of a blood clot. They migrate to the wound site and release ligands that attract more platelets, forming a cap that prevents blood flow from the tissue.
- Platelets contribute to hemostasis in a number of ways. They first bind to substances outside the injured endothelium. They then modify their structure, activate receptors, and release chemical messengers. Finally, they communicate with one another via receptor bridges, culminating in platelet aggregation. This process, known as primary hemostasis, is linked to the activation of the coagulation cascade, which results in fibrin deposition and linkage, known as secondary hemostasis. Platelets also help with wound healing and are involved in both innate and adaptive immune responses within blood vessels.
- Finally, platelets are anucleated cells generated from megakaryocytic bone marrow cells. They help to maintain hemostasis, start blood clotting, and have non-hemostatic immune actions. Platelets produce inflammatory mediators, interact with infections, and have an impact on immunological responses. Platelets have nucleic acids, granules, and immunological receptors despite the lack of a nucleus. They are necessary for preventing excessive bleeding and helping the body’s immune defenses.
Platelets (Thrombocytes) Definition
Platelets, also known as thrombocytes, are anucleated cells derived from megakaryocytic cells in the bone marrow. They are the second most abundant cells in the blood circulation and play a crucial role in maintaining hemostasis by initiating blood clotting. Platelets also have non-hemostatic immune functions and can release inflammatory mediators, interact with pathogens, and influence immune responses. Despite lacking a nucleus, platelets contain nucleic acids, granules, and immune receptors. They are essential for preventing excessive bleeding and contribute to the body’s immune defenses.
Characteristics of Platelets (Thrombocytes)
Platelets, also known as thrombocytes, possess several characteristic features that contribute to their vital functions within the body. Here are some key characteristics of platelets:
- Size and Shape: Platelets are relatively small compared to other blood cells, with an average diameter of 2-3 micrometers. They have a disc-shaped appearance, although their shape can rapidly change in response to external stimuli.
- Origin: Platelets are produced in the bone marrow from large precursor cells called megakaryocytes. These megakaryocytes release platelets into the bloodstream, where they circulate and fulfill their roles.
- Lifespan: Platelets have a limited lifespan, surviving in the circulation for about 7-10 days before being cleared by the body’s reticuloendothelial system.
- Hemostasis: One of the primary functions of platelets is to participate in hemostasis, the process of stopping bleeding after blood vessel injury. Platelets adhere to damaged blood vessel walls and aggregate, forming a plug that helps to halt bleeding.
- Inflammation: Platelets play a role in the body’s inflammatory response. They release various molecules, including cytokines and chemokines, which attract immune cells to the site of injury and contribute to the initiation and regulation of inflammation.
- Wound Healing: Platelets also contribute to wound healing. They release growth factors, such as platelet-derived growth factor (PDGF) and transforming growth factor-beta (TGF-β), which promote the formation of new blood vessels (angiogenesis) and aid in the repair of damaged tissues.
- Responsiveness: Platelets are highly responsive to different stimuli. They can change their shape, adhere to surfaces, aggregate, and release granules containing various substances in response to factors like changes in blood flow, exposure to drugs, and the presence of microorganisms.
- Abnormalities: Abnormal platelet function or count can lead to bleeding disorders or thrombotic disorders. Decreased platelet count (thrombocytopenia) or impaired platelet function can result in increased bleeding tendencies, while elevated platelet count (thrombocytosis) or hyperactive platelets may increase the risk of blood clots.
- Medical Applications: Platelet transfusions can be used in the treatment of bleeding disorders, such as immune thrombocytopenic purpura (ITP) or platelet dysfunction. Conversely, medications that inhibit platelet aggregation, such as aspirin or antiplatelet drugs, are utilized to prevent abnormal blood clot formation and reduce the risk of conditions like heart attacks or strokes.
These characteristic features of platelets highlight their essential role in maintaining hemostasis, contributing to inflammation and wound healing, and their significance in various medical applications related to bleeding and clotting disorders.
Structure of Platelets (Thrombocytes)
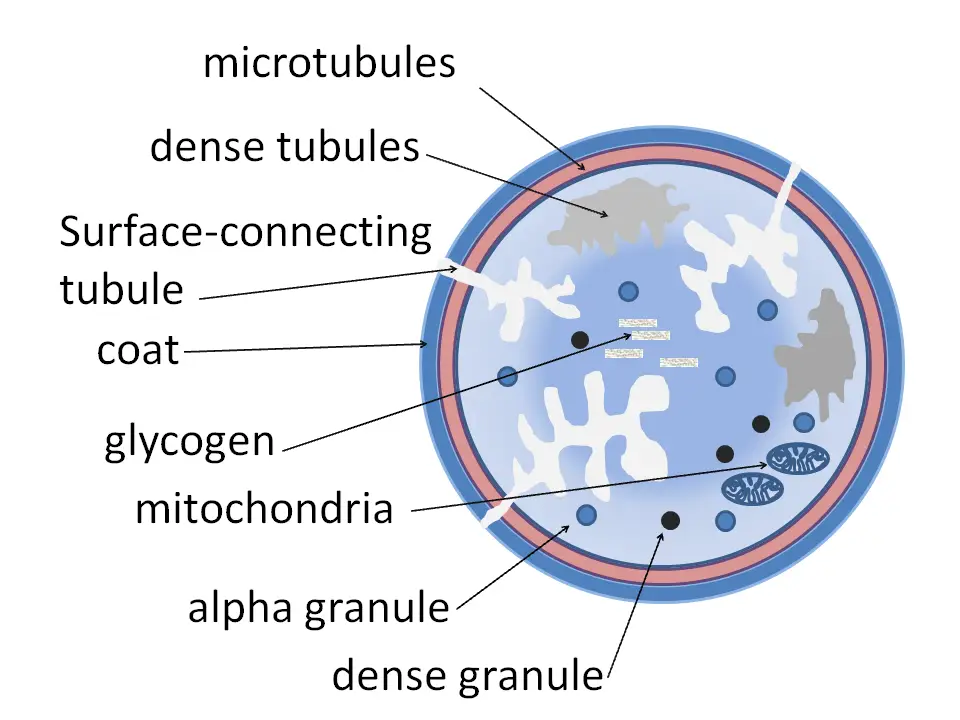
The structure of platelets, also known as thrombocytes, can be divided into different zones, each with specific components and functions:
- Peripheral Zone: This outermost zone of the platelet is rich in glycoproteins that play a crucial role in platelet adhesion, activation, and aggregation. Examples of these glycoproteins include GPIb/IX/V, GPVI, and GPIIb/IIIa. They are essential for interactions with other cells and molecules involved in hemostasis.
- Sol-gel Zone: The sol-gel zone is located beneath the peripheral zone and consists of microtubules and microfilaments. These structural elements allow platelets to maintain their characteristic discoid shape and provide stability to the cell.
- Organelle Zone: The organelle zone contains platelet granules, which are small membrane-bound compartments within the cytoplasm. There are two main types of granules in platelets:
- Alpha Granules: These granules are the largest and most abundant in platelets. They contain various clotting mediators, including factor V, factor VIII, fibrinogen, fibronectin, platelet-derived growth factor, and chemotactic agents. Alpha granules play a significant role in promoting blood clot formation and wound healing.
- Delta Granules (Dense Bodies): These granules are smaller and denser than alpha granules. They contain molecules such as ADP, calcium, and serotonin, which are platelet-activating mediators. The release of these substances contributes to platelet activation and the formation of a stable blood clot.
- Membranous Zone: The innermost zone of the platelet is the membranous zone. It contains membranes derived from the smooth endoplasmic reticulum of the megakaryocyte, the precursor cell of platelets. These membranes form a dense tubular system, which is connected to the surface platelet membrane. This tubular system is responsible for synthesizing thromboxane A2, a potent vasoconstrictor and platelet activator.
In terms of overall structure, platelets are small, anucleated cell fragments with a diameter of 1-3 µm. However, upon activation, their size can increase up to 6 µm. Although platelets lack many components of a typical cell, they contain cellular organelles such as RNA, ribosomes, mitochondria, and granules that are essential for their function.
The presence of granules is a distinguishing feature of platelets. Alpha granules, dense granules, and lysosomes are the three main types of granules found in platelets. Each type of granule has specific contents and plays a role in platelet function. Alpha granules are involved in hemostasis, while dense granules contain molecules that contribute to platelet activation. Lysosomes contain hydrolytic enzymes involved in various cellular processes.
Shape of Platelets
Platelets exhibit a distinctive shape that undergoes dynamic changes upon activation. Here are some key points about the shape of platelets:
- Inactive Shape: In their inactive state, platelets are biconvex discoid structures, resembling a lens or a flattened oval. They have a typical diameter of 2-3 µm, making them much smaller than other blood cells.
- Activated Shape: When platelets become activated in response to various stimuli, their shape changes. Activated platelets develop cell membrane projections that cover their surface, giving them a more irregular and spiky appearance.
- Approximation to Oblate Spheroids: The shape of platelets can be approximated as oblate spheroids, which are three-dimensional objects that are flattened along one axis. The ratio of their semi-axes can vary from 2 to 8. This approximation is useful for modeling the hydrodynamic and optical properties of a population of platelets and for determining the geometric parameters of individual platelets using flow cytometry.
- Biophysical Models: More advanced biophysical models have been developed to better understand the surface morphology and shape of platelets. These models take into account various factors and physical principles to obtain a more accurate representation of platelet geometry in both resting and activated states.
Understanding the shape of platelets is important as it influences their interactions with blood vessels, other cells, and molecules. The dynamic changes in shape upon activation enable platelets to perform their functions, including adhesion to damaged blood vessels, aggregation to form blood clots, and interactions with immune cells during the inflammatory response.
Development of Platelets
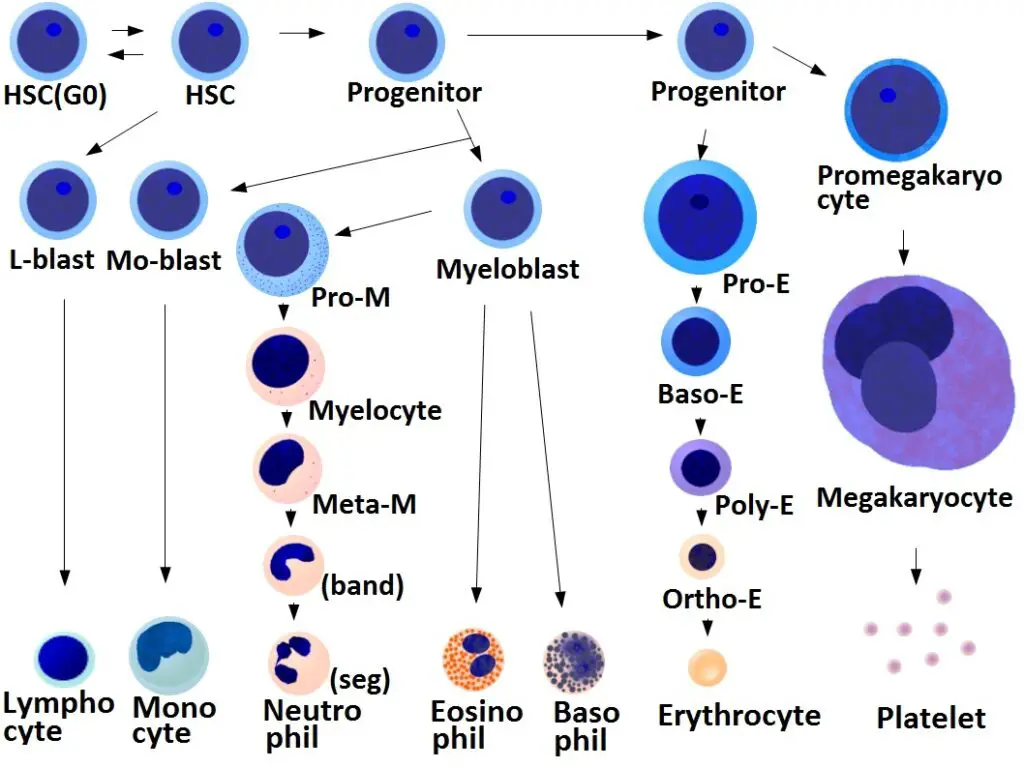
The development of platelets, also known as thrombocytes, involves several stages and regulatory mechanisms. Here are some key points about the development of platelets:
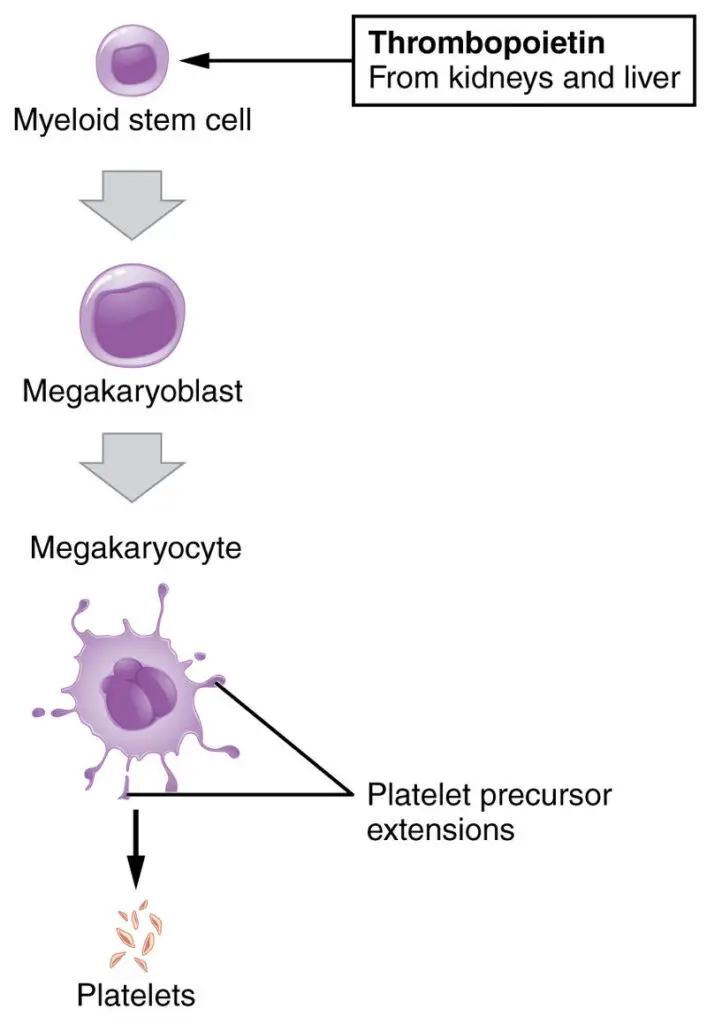
- Regulation by Thrombopoietin: The production of megakaryocytes and platelets is tightly regulated by a hormone called thrombopoietin. Thrombopoietin is primarily produced in the kidneys and liver. It acts on hematopoietic stem cells in the bone marrow, stimulating their differentiation into megakaryocyte progenitor cells.
- Megakaryocyte Production: Megakaryocytes are large, multinucleated cells that give rise to platelets. Each megakaryocyte can produce between 1,000 and 3,000 platelets during its lifetime. Megakaryocytes undergo maturation and development in the bone marrow.
- Platelet Production: Platelets are released from mature megakaryocytes through a process called platelet shedding or fragmentation. As megakaryocytes mature, they extend long proplatelet projections into the bone marrow sinusoids. These projections undergo fragmentation, resulting in the release of platelets into the bloodstream.
- Daily Platelet Production: In a healthy adult, approximately 10^11 (100 billion) platelets are produced daily. This high rate of platelet production ensures a sufficient supply of platelets in the circulation.
- Storage in the Spleen: Reserve platelets are stored in the spleen, a secondary lymphoid organ. These platelets remain in the spleen until they are needed. Splenic contraction, induced by the sympathetic nervous system, can release these stored platelets into circulation in response to various stimuli, such as injury or bleeding.
- Platelet Lifespan: Once in the circulation, platelets have an average lifespan of 8 to 9 days. The lifespan of individual platelets is regulated by the internal apoptotic pathway, which involves the activity of the Bcl-xL protein. After their lifespan, old platelets are cleared from the circulation through phagocytosis, primarily in the spleen and liver.
How do Platelets work against pathogens? (Immunity)
Platelets play an important role in the immune response against pathogens. Here’s how platelets work against pathogens in the context of immunity:
- Activation and Morphological Changes: When platelets are activated in response to different stimuli, they undergo morphological changes. They lose their round, spherical shape and develop an irregularly shaped appearance with pseudopodia. This change in shape allows them to interact with pathogens and immune cells more effectively.
- Granule Release: Activation of platelets triggers the fusion of storage granules in the cytoplasm with the cell membrane. This fusion leads to the release of a set of cytokines and the expression of surface molecules. These released molecules have various functions, including attracting immune cells to the site of infection, enhancing the immune response, and promoting inflammation.
- Increased Adhesion and Aggregation: Activation of platelets upregulates the affinity of adhesion molecules like GPIb-V-IX complexes. This increased affinity facilitates platelet adhesion and aggregation, which can help in trapping and immobilizing pathogens at the site of infection.
- Surface Receptors: Platelets express various surface receptors, including Toll-like receptors (TLRs), CD154 receptors, FcγRIIA, glycoprotein VI, and C-type lectin receptors. These receptors play a role in the activation of different immune cells and induce immune responses. For example, TLR4 activation in platelets can enhance neutrophil activation and the formation of neutrophil extracellular traps, which help prevent the spread of bacteria.
- Fibrinogen Binding: Platelets have receptors that bind to fibrinogen, a protein involved in blood clotting. This binding activates platelets and triggers the release of cytoplasmic granules, which contain molecules that can further contribute to the immune response against pathogens.
- Release of Inflammatory Molecules: The activation of platelets leads to the release of several molecules into the bloodstream. These molecules, such as cytokines and chemokines, have the ability to induce inflammation and other immune responses in the body. They can attract immune cells to the site of infection and promote an effective immune defense against pathogens.
By participating in immune responses, platelets contribute to the overall defense against pathogens and help in maintaining the balance between hemostasis and immunity. Their ability to interact with immune cells, release immune mediators, and induce inflammatory responses makes them an important component of the immune system’s arsenal against pathogens.
Disorders Related to High and Low Number of Platelets
Abnormalities in platelet count or function can lead to bleeding disorders or thrombotic disorders, which increase the risk of blood clots. Here are some examples of disorders related to high and low numbers of platelets:
- Thrombocytopenia: This is a condition in which the number of platelets in the blood is lower than normal. It can be caused by a range of factors, including bone marrow disorders, autoimmune diseases, infections, and certain medications. Thrombocytopenia can lead to excessive bleeding or bruising, and in severe cases, can be life-threatening.
- Idiopathic thrombocytopenic purpura (ITP): This is a type of autoimmune disorder in which the body produces antibodies that attack and destroy platelets. It can result in low platelet counts and can cause excessive bruising and bleeding.
- Thrombocytosis: This is a condition in which the number of platelets in the blood is higher than normal. It can be caused by a range of factors, including cancer, infections, and certain medications. Thrombocytosis can increase the risk of blood clots, which can lead to serious health problems such as stroke or heart attack.
- Hemophilia: This is a genetic disorder in which the blood does not clot properly, leading to excessive bleeding. It is caused by a deficiency of certain clotting factors, which can include platelets.
- Von Willebrand disease: This is a genetic disorder in which the body does not produce enough of a protein called von Willebrand factor, which is needed for proper blood clotting. It can lead to excessive bleeding or bruising.
- Disseminated intravascular coagulation (DIC): This is a serious medical condition in which the body’s clotting system becomes overactive, leading to the formation of small blood clots throughout the body. This can result in a depletion of platelets, leading to bleeding disorders.
Treatment for platelet disorders may involve medications to stimulate or suppress platelet production, blood transfusions, or other medical interventions to manage the underlying cause of the disorder.
Causes of low platelet count – What is the most common cause of low platelet count?
There are several potential causes of low platelet count, a condition known as thrombocytopenia. Some common causes include:
- Decreased production of platelets: This can occur due to bone marrow disorders, such as aplastic anemia, leukemia, myelodysplastic syndromes, or infections that affect the bone marrow.
- Increased destruction of platelets: Certain conditions can lead to increased destruction or removal of platelets from the bloodstream. Examples include immune thrombocytopenic purpura (ITP), where the immune system mistakenly targets and destroys platelets, and thrombotic thrombocytopenic purpura (TTP), a rare blood disorder characterized by the formation of blood clots in small blood vessels.
- Medications and treatments: Some medications can cause a decrease in platelet count as a side effect. Examples include certain antibiotics, diuretics, chemotherapy drugs, and anticonvulsants. Radiation therapy and certain surgical procedures can also affect platelet production or function.
- Viral or bacterial infections: Infections such as hepatitis C, HIV, Epstein-Barr virus (EBV), and dengue fever can cause a temporary decrease in platelet count.
- Nutritional deficiencies: Deficiencies in certain vitamins, such as vitamin B12 or folate, can affect the production of platelets.
- Alcohol consumption: Chronic alcohol abuse can suppress bone marrow function, leading to decreased platelet production.
- Autoimmune disorders: Autoimmune diseases, such as systemic lupus erythematosus (SLE) or rheumatoid arthritis, can cause immune-mediated destruction of platelets.
- Genetic disorders: Rare genetic disorders, such as Wiskott-Aldrich syndrome or May-Hegglin anomaly, can cause low platelet count.
- Certain medications: Some medications, such as heparin (a blood thinner), can induce a condition called heparin-induced thrombocytopenia (HIT), where platelet counts decrease due to an immune reaction to the medication.
- Pregnancy: Some pregnant women may develop gestational thrombocytopenia, which is a temporary decrease in platelet count during pregnancy.
Causes of high platelet count
A high platelet count, also known as thrombocytosis, can be caused by various factors. Here are some common causes:
- Primary thrombocytosis: This is a condition in which the bone marrow produces too many platelets without an underlying cause. It is often caused by mutations in the cells that produce platelets. Primary thrombocytosis is usually benign but can increase the risk of blood clots.
- Secondary thrombocytosis: This type of thrombocytosis occurs as a result of an underlying condition or cause. It can be caused by various factors, including:
- a. Infections: Certain infections, such as tuberculosis, pneumonia, or inflammatory disorders, can cause an increase in platelet production.
- b. Inflammation: Chronic inflammatory conditions like rheumatoid arthritis, inflammatory bowel disease, or vasculitis can lead to thrombocytosis.
- c. Iron deficiency anemia: When the body lacks sufficient iron, it can cause an increase in platelet production as a compensatory mechanism.
- d. Surgical removal of the spleen: The spleen helps regulate platelet levels in the body. After spleen removal, platelet count may increase.
- e. Cancer: Some cancers, such as lung, ovarian, or gastrointestinal cancers, can cause thrombocytosis. The abnormal growth of cancer cells can stimulate the bone marrow to produce more platelets.
- f. Blood loss or trauma: Following significant blood loss or physical trauma, the body may produce more platelets to aid in clotting and healing.
- g. Medications: Certain medications, including corticosteroids, epinephrine, or birth control pills, can lead to an increase in platelet count.
- Essential thrombocythemia: This is a rare bone marrow disorder characterized by the overproduction of platelets. The cause of essential thrombocythemia is not well understood, but it is thought to involve genetic mutations in the bone marrow cells.
It’s important to note that a high platelet count doesn’t always indicate a serious underlying condition. However, if you have concerns about your platelet count, it is best to consult a healthcare professional for an accurate diagnosis and appropriate management.
What is the Normal platelet count in Blood? – Platelets normal range
The normal platelet count for adults typically ranges from 150,000 to 450,000 platelets per microliter (μL) of blood. However, the exact normal range may vary slightly depending on the specific laboratory and reference values used.
It’s worth noting that platelet counts can fluctuate due to various factors, such as recent illness, medication use, or temporary changes in the body. If your platelet count falls slightly below or above the normal range, it may not necessarily indicate a health concern. However, if your platelet count consistently falls outside the normal range, it is important to consult a healthcare professional for further evaluation and appropriate management.
The normal range for platelet count in adults is typically considered to be between 150,000 and 450,000 platelets per microliter (μL) of blood. However, it’s important to note that the specific reference range may vary slightly depending on the laboratory and the methodology used to measure platelet count.
Here is a breakdown of the platelet count reference ranges commonly used:
- Normal range: 150,000 to 450,000 platelets/μL
- Mild thrombocytopenia: Platelet count between 100,000 and 150,000 platelets/μL
- Moderate thrombocytopenia: Platelet count between 50,000 and 100,000 platelets/μL
- Severe thrombocytopenia: Platelet count below 50,000 platelets/μL
It’s important to remember that these reference ranges are approximate and may vary based on individual factors and the specific laboratory’s standards. If you have concerns about your platelet count, it’s best to consult with a healthcare professional who can interpret your results in the context of your overall health and medical history.
How to increase platelet count?
Here are some general suggestions that may help increase platelet count:
- Eat a balanced diet: Ensure that your diet includes a variety of nutrient-rich foods, such as fruits, vegetables, whole grains, lean proteins, and healthy fats. Certain nutrients, such as vitamin K, vitamin B-12, folate, and iron, are essential for proper platelet production.
- Avoid alcohol and tobacco: Both alcohol and tobacco use can suppress platelet production and impair their function. Minimizing or avoiding these substances can be beneficial.
- Stay hydrated: Drinking an adequate amount of water can help maintain proper blood volume and circulation, which is important for platelet function.
- Avoid medications that can lower platelet count: Certain medications, such as certain antibiotics, anticonvulsants, and diuretics, can cause a decrease in platelet count. Consult with your healthcare provider about any medications you are taking and their potential impact on platelet levels.
- Manage underlying medical conditions: If your low platelet count is related to an underlying medical condition, it’s important to manage that condition effectively. Follow your healthcare provider’s recommendations and treatment plans.
- Consider medical treatments: In some cases, medical interventions may be necessary to increase platelet count. This can include medications, such as corticosteroids or immune globulin, or procedures like platelet transfusion or bone marrow stimulation.
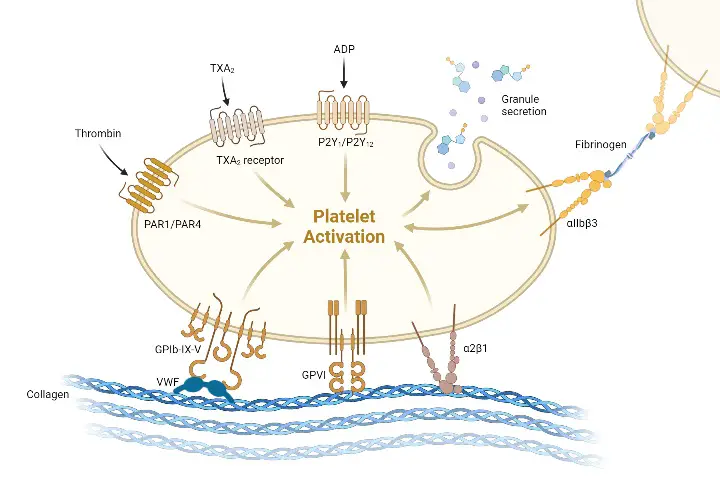
Platelet receptors
Platelets, also known as thrombocytes, have several different types of receptors on their surface that play a critical role in the process of hemostasis. These receptors allow platelets to sense changes in the local environment and to respond appropriately to injuries or other stimuli. Here are some of the main types of platelet receptors:
- Adhesion receptors: Platelets use adhesion receptors, such as integrins and glycoproteins, to adhere to the damaged blood vessel wall and to other platelets, forming a platelet plug.
- Activation receptors: Platelets also have activation receptors, such as P2Y12 and thromboxane A2 receptor, that respond to signals from other cells or from the damaged tissue, triggering a series of intracellular signaling pathways that lead to platelet activation and aggregation.
- Fc receptors: Platelets have Fc receptors, which allow them to bind to and phagocytose antibody-coated cells and other particles, removing them from the circulation.
- Toll-like receptors (TLRs): Platelets also have Toll-like receptors, which recognize and respond to pathogen-associated molecular patterns (PAMPs) and danger-associated molecular patterns (DAMPs), activating the platelets and contributing to the immune response.
- Clearance receptors: Platelets have clearance receptors, such as the thrombopoietin receptor, that regulate platelet production and clearance from the circulation.
- Protease-activated receptors (PARs): Platelets also have protease-activated receptors, which are activated by thrombin and other proteases that are generated during the coagulation cascade. PARs play a key role in platelet activation and aggregation.
- C-type lectin receptors: Platelets have C-type lectin receptors, which recognize and bind to carbohydrates on the surface of pathogens, contributing to the immune response.
- CD40 ligand (CD40L) receptors: Platelets express CD40L, which binds to CD40 on the surface of immune cells, activating them and contributing to the immune response.
The different types of platelet receptors allow platelets to respond to a wide range of signals and to coordinate their responses with other cells in the body. Dysregulation of platelet receptors can lead to bleeding disorders or thrombotic disorders, increasing the risk of bleeding or blood clots. Understanding the role of platelet receptors is important for developing new therapies for platelet-related disorders.
Hemostasis Mechanism
Hemostasis is a complex process involving multiple steps that aim to stop acute bleeding and maintain vascular integrity. The process of hemostasis can be divided into three main steps: adhesion, activation, and aggregation. Let’s explore each step:
- Adhesion: In the first step of hemostasis, platelets adhere to the damaged site of the blood vessel. The intact endothelial lining normally prevents platelet adhesion by releasing substances like nitric oxide, prostacyclin, and CD39. However, when the endothelial layer is disrupted due to injury, subendothelial collagen is exposed. Platelets bind to collagen through receptors like GP1b-IX-V and GPVI, and they also bind to von Willebrand factor (VWF) that is present in the subendothelial matrix. This adhesion process anchors platelets to the site of injury.
- Activation: Once platelets adhere to the damaged vessel wall, they undergo activation. Activation is triggered by various signals, including the binding of collagen to GPVI receptors and the release of tissue factor, which initiates the extrinsic coagulation cascade. Activation leads to a series of intracellular signaling events, resulting in changes in platelet morphology and function. Platelet activation involves calcium mobilization, which plays a crucial role in platelet conformational change and degranulation. Thrombin, a potent platelet activator, is generated during the coagulation cascade and further enhances platelet activation.
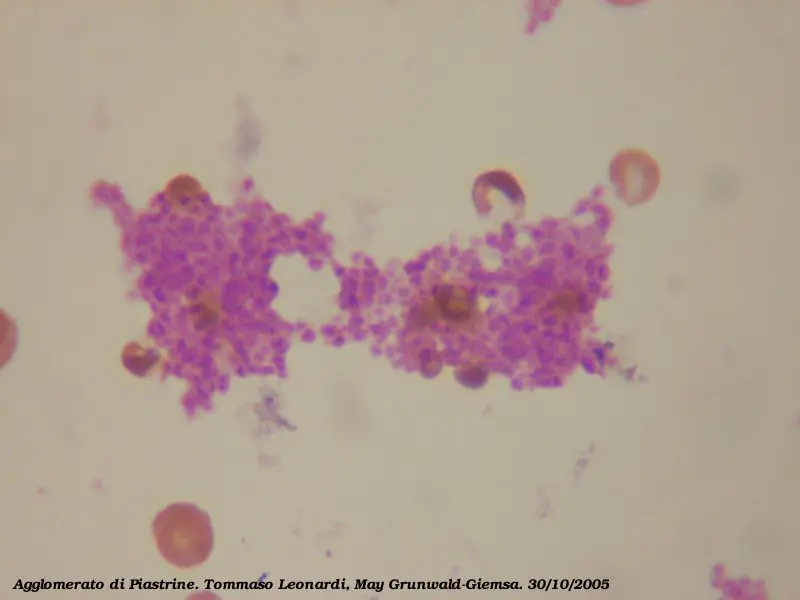
- Aggregation: The final step in hemostasis is platelet aggregation, where activated platelets form aggregates and clump together to form a platelet plug. Platelet aggregation is primarily mediated by the binding of fibrinogen to the activated form of GPIIb/IIIa receptors on platelet surfaces. This binding bridges adjacent platelets, allowing them to adhere to each other and form stable aggregates. Additionally, platelet granule secretion occurs during aggregation. Platelet granules contain various substances, such as ADP, calcium, serotonin, and growth factors, which further contribute to platelet activation and recruitment of more platelets to the site of injury.
It is important to note that the steps of hemostasis described above occur simultaneously and in coordination with the coagulation cascade. The formation of a stable platelet plug is reinforced by the deposition of fibrin, which is generated through the activation of clotting factors in the coagulation cascade.
In summary, hemostasis involves a sequence of events that include platelet adhesion, activation, and aggregation. These steps are critical for the formation of a platelet plug and the prevention of excessive bleeding. The interplay between platelets, the endothelium, and the coagulation system ensures the maintenance of vascular integrity and efficient wound healing.
Functions of Platelets (Thrombocytes)
Platelets, also known as thrombocytes, serve various functions in the body. Here are some key functions of platelets:
- Hemostasis: Platelets play a crucial role in hemostasis, the process that stops bleeding after blood vessel injury. They form a platelet plug at the site of injury, sealing the damaged blood vessel and preventing excessive blood loss. Platelets aggregate with each other and with the damaged vessel wall, initiating the coagulation cascade, which leads to the formation of a blood clot.
- Immune Response: Platelets are among the first cells to detect tissue damage and the presence of microbial pathogens. They express pattern recognition receptors, such as Toll-like receptors (TLRs), which enable them to recognize pathogen-associated molecular patterns. This recognition helps to initiate an immune response and activate other immune cells to fight against pathogens.
- Secretion of Mediators: When activated, platelets release a variety of mediators, including cytokines, chemokines, and growth factors. These substances play a role in the recruitment and activation of immune cells, such as macrophages, neutrophils, and dendritic cells. Platelet-derived growth factors promote tissue repair and the formation of new blood vessels.
- Inflammation Modulation: Platelets can influence the inflammatory response by releasing mediators that attract immune cells to the site of injury or infection. They also interact with endothelial cells and immune cells, contributing to the regulation of inflammation in organs like the lungs, skin, and kidneys.
- Removal of Damaged Cells: Platelets participate in the clearance of damaged cells from the circulation. They can phagocytose and remove old or damaged red blood cells, white blood cells, and other cellular debris, assisting in the maintenance of a healthy blood environment.
- Prevention of Infection: Platelets possess antimicrobial peptides that help to prevent the growth and spread of bacteria and other microorganisms in the bloodstream. This antimicrobial activity contributes to the body’s defense against infections.
- Maintenance of Blood Vessel Integrity: Platelets secrete substances that promote the maintenance and repair of the blood vessel wall. These substances help to regulate the permeability of blood vessels, preventing leakage of fluid into surrounding tissues.
- Thrombus Formation: While thrombus formation is primarily a protective mechanism, in certain medical conditions, platelets can contribute to the formation of blood clots (thrombi) within blood vessels. These clots can obstruct blood flow and lead to serious complications if not properly regulated.
These functions highlight the vital role that platelets play in maintaining hemostasis, regulating immune responses, and preserving the integrity of the circulatory system.
FAQ
What are platelets?
Platelets, also called thrombocytes, are small, disc-shaped blood cells that play a key role in hemostasis, or the process of blood clotting. They are formed in the bone marrow from precursor cells called megakaryocytes.
How are platelets produced in the body?
Platelets are produced in the bone marrow from megakaryocytes, which are large, multinucleated cells that undergo cytoplasmic fragmentation to release platelets into the bloodstream.
What is the function of platelets in hemostasis?
Platelets play a critical role in hemostasis by forming a plug at the site of vascular injury, sealing the breach and preventing further blood loss. They also secrete a variety of factors that promote coagulation and wound healing.
How are platelets activated in response to injury or damage?
Platelets are activated in response to a variety of signals, including damage to the blood vessel wall, exposure to collagen or other extracellular matrix proteins, and signaling molecules such as thrombin and ADP. Activation triggers a series of intracellular signaling pathways that lead to platelet aggregation and the formation of a stable clot.
What are some common disorders related to platelets, such as thrombocytopenia or thrombocythemia?
Thrombocytopenia is a condition characterized by a low platelet count, which can lead to an increased risk of bleeding. Thrombocythemia is a condition characterized by a high platelet count, which can increase the risk of blood clots and other complications.
How are platelets counted in a laboratory test, and what is a normal platelet count?
Platelets are typically counted using a machine that measures the number and size of cells in a blood sample. A normal platelet count ranges from 150,000 to 450,000 platelets per microliter of blood.
How are platelets transfused to patients with low platelet counts or bleeding disorders?
Platelets can be collected from donated blood and transfused to patients with low platelet counts or bleeding disorders. They can be transfused as whole blood or as a component of blood products such as platelet concentrates or fresh frozen plasma.
What medications can affect platelet function or count, and how do they work?
Medications such as aspirin, clopidogrel, and heparin can affect platelet function or count by inhibiting platelet activation or aggregation. These medications are often used to prevent blood clots in patients at high risk of thrombosis.
How do platelets interact with other cells in the body, such as endothelial cells, leukocytes, and red blood cells?
Platelets interact with other cells in the body through a variety of receptors and signaling molecules. They can adhere to and activate endothelial cells, promote leukocyte recruitment and activation, and modulate red blood cell function.
What are some current research areas in platelet biology and platelet-related disorders?
Current research in platelet biology is focused on understanding the complex signaling pathways and interactions between platelets and other cells in the body. Researchers are also investigating new therapies for platelet-related disorders, including novel antiplatelet agents and platelet transfusion strategies.
References
- Nikolić, L., Vukovic-Suvajdzic, N., Bugarinovic, S., & Plećaš, D. (2016). Platelets (thrombocytes): The other recognized functions.
- Boilard, E., & Nigrovic, P. A. (2017). Platelets. Kelley and Firestein’s Textbook of Rheumatology, 264–273.e3. doi:10.1016/b978-0-323-31696-5.00016-4
- Darnell, C. M., & Sacher, R. A. (2014). Platelet Disorders. Pathobiology of Human Disease, 1553–1561. doi:10.1016/b978-0-12-386456-7.07909-0
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/what-are-platelets-and-why-are-they-important
- https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=160&ContentID=36
- https://www.wikilectures.eu/w/Thrombocytes
- https://www.ouhsc.edu/platelets/platelets/platelets%20intro.html
- https://microbenotes.com/platelets-thrombocytes/
- https://scindeks-clanci.ceon.rs/data/pdf/2334-9492/2016/2334-94921603447N.pdf
