Table of Contents
What is Shiga toxin-producing Escherichia coli (STEC)?
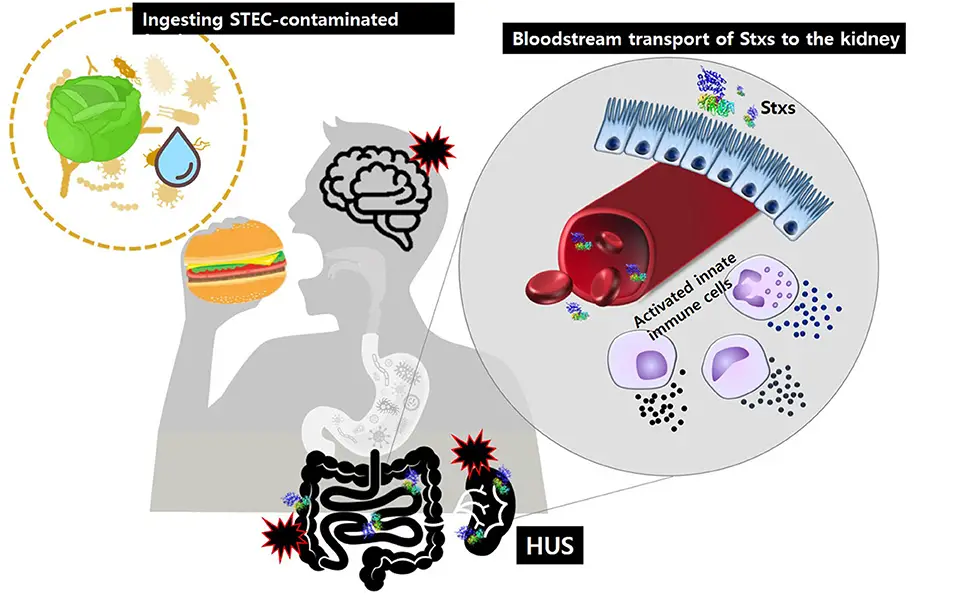
- Shiga toxin-producing Escherichia coli (STEC) is a group of bacteria known for their ability to produce Shiga toxin 1 (Stx1) or Shiga toxin 2 (Stx2). These bacteria are also referred to as verocytotoxin-producing E. coli (VTEC) or enterohemorrhagic E. coli (EHEC). STEC strains can cause bloody diarrhea in infected individuals and, in rare cases, can lead to a severe kidney disease called Hemolytic Uremic Syndrome.
- The most well-known serotype associated with human disease caused by STEC is O157:H7. However, it represents less than 50% of the responsible serotypes, and the prevalent serotypes may vary geographically. STEC infections are more common in industrialized countries compared to developing regions. These bacteria are considered zoonotic pathogens, with ruminants being recognized as the primary reservoir for human infections.
- The infective dose of STEC is remarkably low, with only a few organisms (<102 bacilli) required to initiate an infection. STEC strains are often associated with outbreaks of gastrointestinal illness worldwide, emphasizing the importance of monitoring and disease notification systems.
- STEC strains are categorized into different serogroups, with O157, O26, O111, O103, and O145 being frequently associated with severe cases. However, as detection and typing technologies improve, other serogroups are also being reported.
- STEC strains produce potent cytotoxins known as Shiga toxins or verocytotoxins. These toxins inhibit protein synthesis within eukaryotic cells and are responsible for the characteristic symptoms associated with STEC infections. Enterohemorrhagic E. coli (EHEC) is a subset of STEC strains that has been particularly linked to bloody diarrhea and hemolytic uremic syndrome (HUS) in industrialized countries. Although O157:H7 is the most common serotype causing severe disease, non-O157 EHEC strains, such as those belonging to serogroups O26, O111, O103, and O145, are increasingly being reported as causative agents.
- Understanding the characteristics and risks associated with STEC strains is crucial for effective surveillance, prevention, and management of infections caused by these bacteria.
Virulence factors
Virulence factors are key components that contribute to the pathogenicity of Shiga toxin-producing Escherichia coli (STEC). Here are some important virulence factors associated with STEC:
- Shiga toxins (Stx): Shiga toxins are considered the major virulence factors of STEC. They are cytotoxins that share structural similarities and have similar biological activities. There are two main groups of Shiga toxins: Stx1, which is similar to the toxin produced by Shigella dysenteriae type 1, and Stx2, which has less than 60% amino acid sequence similarity with Stx1. The genetic information for producing Stx1 and Stx2 is located in lambdoid prophages integrated in the STEC chromosome. Stx2 is particularly associated with severe human disease, and different variants of Stx2 with altered characteristics have been described.
- Attaching and effacing adhesion (A/E): Many STEC strains, especially those belonging to the enterohemorrhagic E. coli (EHEC) group, colonize the intestinal mucosa and induce a characteristic histopathologic lesion known as attaching and effacing (A/E). This lesion involves cytoskeletal changes, effacement of microvilli, and intimate adherence between the bacteria and the epithelial cell membrane. The mechanism of A/E adhesion is genetically governed by a large pathogenicity island (PAI) called the Locus of Enterocyte Effacement (LEE).
- Other virulence factors: STEC strains possess additional virulence factors that contribute to their pathogenicity. The genomic analysis of STEC O157:H7, a prominent serotype associated with human disease, has revealed the presence of foreign DNA acquired through horizontal gene transfer. Some of these regions are considered putative pathogenicity islands (PAIs) because they carry virulence-associated genes and show characteristics distinct from the rest of the chromosome. One example is the PAI known as O#122, which is present in most EHEC and enteropathogenic E. coli (EPEC) strains. STEC O157 also carries a large virulence plasmid called pO157, which encodes proteins involved in pathogenesis. This plasmid harbors genes such as the enterohemolysin (hly) operon, katP (encoding a catalase-peroxidase), espP (encoding a serine protease), and toxB (a recently described virulence gene).
These virulence factors play crucial roles in the pathogenesis of STEC infections, contributing to the colonization and damage of the intestinal epithelium, as well as the systemic effects observed in severe cases. Understanding the mechanisms and characteristics of these virulence factors is important for developing strategies for diagnosis, prevention, and treatment of STEC infections.
What is Shiga toxin?
Shiga toxin is a family of related toxins produced by certain bacteria, including Shigella dysenteriae and specific serotypes of Escherichia coli, such as Shiga toxin-producing E. coli (STEC). The toxins are named after Kiyoshi Shiga, who first described the bacterial origin of dysentery caused by Shigella dysenteriae. Here are some key points about Shiga toxin:
- Types of Shiga Toxin:
- Shiga toxin has two major groups, Stx1 and Stx2, which are expressed by genes carried within the genome of lambdoid prophages.
- Stx1 is nearly identical to the toxin produced by Shigella dysenteriae, while Stx2 shares around 56% sequence identity with Stx1.
- These toxins are also known by various names such as Shiga-like toxins (SLT), verocytotoxins/verotoxins, and cytotoxins.
- Mode of Action:
- Shiga toxin binds to specific glycolipids on the host cell surface, primarily globotriaosylceramide (Gb3), through its pentameric B subunit.
- After binding, the A subunit of the toxin is internalized and cleaved into two parts.
- The A1 fragment then enters the host cell’s cytosol and targets the ribosome, where it cleaves a specific adenine nucleobase from the 28S RNA of the 60S subunit.
- This inhibits protein synthesis within the target cell, leading to cell damage and disruption of normal cellular functions.
- Pathogenic Effects:
- Shiga toxin primarily affects small blood vessels, such as those in the digestive tract, kidney, and lungs.
- It is associated with symptoms such as abdominal pain and watery diarrhea.
- In severe cases, particularly those caused by certain STEC strains, it can lead to hemorrhagic colitis, a condition characterized by bloody diarrhea and severe abdominal pain.
- Shiga toxin is also linked to the development of hemolytic-uremic syndrome (HUS), a potentially life-threatening condition characterized by acute kidney failure, thrombocytopenia (low platelet count), and microangiopathic hemolytic anemia.
- Receptors and Tissue Specificity:
- The toxin’s binding and toxic effects are mediated by the presence of specific receptors, particularly Gb3, on the surface of target cells.
- Tissues with a high concentration of Gb3 receptors include the intestinal villi, renal endothelial cells, and neurons.
- The binding of Shiga toxin to these receptors can lead to tissue damage and the characteristic symptoms associated with infection.
Understanding the structure, mode of action, and tissue specificity of Shiga toxin is crucial for comprehending its pathogenic effects and developing strategies for prevention and treatment of related infections.
Epidemiology of STEC infections
- Historical Trends:
- In the 1980s, most STEC O157 outbreaks were food-borne, with the main implicated food vehicles being inadequately cooked beef products and unpasteurized milk.
- Outbreaks associated with low pH products, such as fermented salami, mayonnaise, and yogurt, have been reported in the past decade. This highlights the ability of E. coli O157 to tolerate acidic pH and survive fermentation and drying processes.
- Waterborne outbreaks and outbreaks linked to other environmental exposures have also been increasingly reported. The dispersion of untreated manure in the environment can lead to contamination of various items, acting as secondary vehicles for human infections.
- Contamination of Fruits and Vegetables:
- There has been a growing recognition of STEC outbreaks associated with a wider range of fruits and vegetables. These outbreaks often occur due to fertilization with ruminants’ manure or contamination during harvesting or processing.
- Fruits and vegetables can become contaminated through contact with contaminated soil, water, or manure, highlighting the importance of proper hygiene practices during cultivation and processing.
The epidemiology of STEC infections has evolved over time, with a broader range of food sources and environmental exposures implicated in outbreaks. In addition to traditionally recognized sources like beef products and unpasteurized milk, low pH products, waterborne exposures, and contaminated fruits and vegetables have emerged as potential vehicles for STEC transmission. These observations emphasize the need for comprehensive food safety measures, including proper food handling, processing, and hygiene practices throughout the food production and distribution chain.
Shiga Toxin-Producing Escherichia coli (STEC) Infection
STEC (Shiga toxin-producing Escherichia coli) can cause a range of diseases, varying from mild uncomplicated diarrhea to more severe conditions such as hemorrhagic colitis and Hemolytic Uremic Syndrome (HUS). The severity of the disease is often associated with the STEC O157:H7 serotype, although other serotypes can also cause severe illness.
- Mild Uncomplicated Diarrhea: STEC infections can result in mild cases of diarrhea characterized by loose or watery stools, abdominal discomfort, and sometimes low-grade fever. In these cases, the illness is self-limiting and typically resolves within a few days without complications.
- Hemorrhagic Colitis: Hemorrhagic colitis is a more severe manifestation of STEC infection. It is characterized by bloody diarrhea, abdominal pain, and cramping. The presence of blood in the stools distinguishes it from uncomplicated diarrhea. Hemorrhagic colitis can be accompanied by symptoms such as nausea, vomiting, and low-grade fever. While most cases resolve without complications, medical attention may be required for supportive care and monitoring.
- Hemolytic Uremic Syndrome (HUS): Hemolytic Uremic Syndrome is a rare but potentially life-threatening complication associated with some STEC infections, particularly those caused by the O157:H7 serotype. HUS primarily affects young children and can lead to acute kidney injury, hemolytic anemia (destruction of red blood cells), and low platelet count. It is characterized by the triad of microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury. HUS requires immediate medical attention and hospitalization for management and supportive care.
Risk Factors and Transmission Routes
Risk Factors and the Mode of Transmission of STEC:
- Seasonal Variation: STEC disease is more commonly reported during the warm months, suggesting a seasonal pattern. This may be attributed to factors such as increased consumption of fresh produce, changes in food handling practices, and higher bacterial load in the environment during warmer weather. However, STEC infections can occur year-round.
- Age: The highest incidence of STEC disease occurs in children younger than 5 years. This age group is considered particularly vulnerable to severe complications, such as Hemolytic Uremic Syndrome (HUS), associated with certain STEC strains.
- Consumption of Contaminated Food and Beverages: The primary mode of transmission of STEC is through the ingestion of contaminated food and beverages. The most common sources of infection include:
- a. Undercooked Ground Beef and Meat Products: Consumption of undercooked ground beef or other meat products, such as hamburgers, is a significant risk factor for STEC infection. Improper cooking temperatures may not effectively kill the bacteria, leading to transmission when consumed.
- b. Water: Contaminated water sources, such as drinking water or recreational water, can be a mode of transmission for STEC. Water contaminated with fecal matter, including water from streams, lakes, and wells, can contain the bacteria.
- c. Unpasteurized Milk or Fruit Juices: Consumption of unpasteurized milk or fruit juices, such as cider made from contaminated apples, can introduce STEC into the body. Raw milk and unpasteurized products can harbor bacteria and pose a risk of infection.
- d. Uncooked Vegetables and Fruits: Raw or undercooked vegetables, including leafy greens like spinach, and fruits can be contaminated with STEC, primarily through contact with feces from animals or contaminated irrigation water.
- Person-to-Person Transmission: STEC can also spread from person to person, especially in settings where proper hygiene practices are lacking. Close contact with an infected individual, particularly with fecal matter, can lead to secondary transmission of the bacteria.
- Low Infectious Dose: Ingesting even a small number of STEC bacteria, often fewer than 100, can be sufficient to cause illness in susceptible individuals. This highlights the importance of proper food safety measures, including thorough cooking, practicing good hygiene, and avoiding consumption of high-risk foods.
Toxins and Pathogenic Mechanisms
Toxins and Pathogenesis of Shiga toxin-producing Escherichia coli (STEC):
- Shiga Toxin Structure: There are two main types of Shiga toxins produced by STEC, known as Stx1 and Stx2. Stx1 is essentially identical to the Shiga toxin produced by Shigella dysenteriae, while Stx2 has 60% homology to Stx1. Both toxins are acquired by lysogenic bacteriophages, which are viruses that infect bacteria.
- Toxin Composition: Each Shiga toxin consists of one A subunit and five B subunits. The B subunits are responsible for binding to a specific glycolipid receptor called globotriaosylceramide (Gb3) on the surface of host cells.
- Target Cells: Intestinal villi and renal endothelial cells have a high concentration of Gb3 receptors, making them particularly susceptible to the binding of Shiga toxins produced by STEC.
- Mechanism of Action: Once the Shiga toxins are internalized into host cells, the A subunit is cleaved into two molecules. The A1 fragment of the toxin then binds to 28S ribosomal RNA (rRNA) within the host cell, resulting in the inhibition of protein synthesis. This disruption of protein synthesis leads to cell damage and dysfunction.
- Pathogenicity: STEC strains that produce both Shiga toxins and possess attaching and effacing (A/E) activity are generally more pathogenic than strains producing only one Shiga toxin. The A/E activity is mediated by the Locus of Enterocyte Effacement (LEE) pathogenicity island, which enables intimate attachment of the bacteria to host cells, resulting in characteristic histopathological changes.
- Hemolytic Uremic Syndrome (HUS): HUS, a severe complication associated with some STEC infections, has been particularly associated with the production of Stx2. Stx2 has been shown to have a destructive effect on glomerular endothelial cells in the kidneys. This damage triggers platelet activation, thrombin deposition, and a cascade of events that lead to decreased glomerular filtration and acute renal failure.
- Inflammatory Response: Shiga toxins also stimulate the expression of inflammatory cytokines such as tumor necrosis factor (TNF)-γ and interleukin (IL)-6. This leads to the upregulation of Gb3 receptors on host cells, enhancing the binding and internalization of Shiga toxins, thereby exacerbating the cellular damage and inflammatory response.
Clinical Manifestations and Potential Complications
Clinical Features and Complications of Shiga toxin-producing Escherichia coli (STEC) infections:
- Disease Spectrum: STEC infections can manifest with a range of clinical features, from mild uncomplicated diarrhea to more severe conditions such as hemorrhagic colitis and complications like Hemolytic Uremic Syndrome (HUS).
- Incubation Period: After an incubation period of approximately 3 to 4 days, patients typically develop diarrhea accompanied by abdominal pain.
- Diarrhea and Abdominal Pain: Initially, patients experience non-bloody diarrhea along with abdominal pain. Vomiting may be observed in about half of the patients, but a high fever is generally absent during the early stages.
- Progression to Bloody Diarrhea: Within 2 days of the onset of symptoms, approximately 30% to 65% of patients progress to a more severe form of the disease characterized by bloody diarrhea and intense abdominal pain.
- Hemolytic Uremic Syndrome (HUS): HUS is a serious complication that can occur in approximately 5% to 10% of infected children younger than 10 years. HUS is characterized by acute renal failure, thrombocytopenia (low platelet count), and microangiopathic hemolytic anemia (destruction of red blood cells in small blood vessels).
- Signs and Symptoms of HUS: In individuals with HUS, the following signs and symptoms may be observed:
- Decreased urination: HUS can lead to reduced urine output or oliguria.
- Swelling of limbs: Edema, characterized by swelling of the limbs and other body parts, can occur.
- High blood pressure: Hypertension may be present in individuals with HUS.
- Jaundice: The skin and the whites of the eyes may develop a yellowish discoloration.
- Neurological symptoms: Some individuals with HUS may experience seizures (fits) or other neurological symptoms.
- Bleeding into the skin: Petechiae, purpura, or other signs of bleeding into the skin can occur.
Complications Associated with STEC Infection
Complications of Shiga toxin-producing Escherichia coli (STEC) infections:
- Uncomplicated Disease: In cases of uncomplicated STEC infection, symptoms typically resolve within 4 to 10 days in most untreated patients. With appropriate supportive care and hydration, the majority of individuals recover without long-term complications.
- Hemolytic Uremic Syndrome (HUS): HUS is a severe complication associated with some STEC infections, particularly in children. It is characterized by acute renal failure, thrombocytopenia (low platelet count), and microangiopathic hemolytic anemia (destruction of red blood cells in small blood vessels). HUS can lead to significant morbidity and potentially fatal outcomes.
- Mortality in HUS: In patients with HUS, the mortality rate ranges from 3% to 5%. Despite advances in medical care, HUS can sometimes progress rapidly and result in life-threatening complications.
- Long-Term Sequelae: Even in survivors of HUS, long-term complications can arise. As many as 30% of HUS patients may experience severe sequelae, which can include:
- Renal Impairment: HUS can cause long-lasting damage to the kidneys, leading to chronic kidney disease or kidney failure. Some individuals may require long-term renal replacement therapies, such as dialysis or kidney transplantation.
- Hypertension: High blood pressure (hypertension) can develop as a consequence of kidney damage caused by HUS.
- Central Nervous System (CNS) Manifestations: HUS can affect the central nervous system, resulting in various neurological manifestations. This can include seizures, stroke, cognitive impairment, and other neurological deficits.
It’s important to recognize that while most individuals recover from STEC infections without long-term complications, the risk of severe complications and adverse outcomes is higher in those who develop HUS. Prompt medical evaluation, appropriate management, and close monitoring are crucial in identifying and addressing complications associated with STEC infections, particularly in cases where HUS is suspected or diagnosed.
Diagnosis of STEC Infection
Diagnosis of Shiga toxin-producing Escherichia coli (STEC) infections:
- Sorbitol MacConkey Agar: This selective agar medium can be used to differentiate STEC (particularly EHEC) from other types of E. coli. EHEC strains do not ferment sorbitol and, as a result, produce pale colonies on Sorbitol MacConkey agar, while other E. coli strains typically produce pink colonies.
- Rainbow Agar: Rainbow agar is a specialized medium that aids in the detection of STEC O157 strains. These strains appear as black colonies on Rainbow agar since they are negative for the enzyme beta-glucuronidase.
- Toxin Detection:
- a. Demonstration of Cytotoxicity in Vero Cell Lines: The gold standard method for toxin detection is the demonstration of cytotoxicity in Vero cell lines. This involves exposing Vero cells to patient stool samples or bacterial isolates and observing the presence of cytotoxic effects caused by the release of Shiga toxins.
- b. Fecal Toxin Detection by ELISA or Rapid Tests: Enzyme-linked immunosorbent assays (ELISA) or rapid tests can be used to directly detect the presence of Shiga toxins in fecal samples. These tests are based on the specific binding of antibodies to the toxins, allowing for their identification and quantification.
- c. PCR Differentiation of Toxin Genes: Polymerase chain reaction (PCR) can be employed to differentiate the genes coding for Stx1 and Stx2, the two main types of Shiga toxins. This molecular technique can provide specific information about the presence and type of toxin genes present in STEC strains.
Prevention of STEC Infection
Prevention of Shiga toxin-producing Escherichia coli (STEC) infection:
- Personal Hygiene:
- Do not prepare food for others while experiencing diarrhea.
- Wash hands thoroughly with soap and water after using the toilet and changing diapers. It is also important to wash the hands of diapered children.
- Caregiver Hygiene:
- When caring for someone with diarrhea, wash hands with plenty of soap and water after cleaning the bathroom, assisting with toilet use, or changing diapers, soiled clothes, or sheets. It is crucial to wash the hands of the person being cared for as well.
- Safe Food Handling:
- Always refrigerate meat promptly. Do not leave raw meat at room temperature for an extended period.
- Ensure all ground beef and hamburger are cooked thoroughly, reaching a temperature of 155ºF (68ºC) for at least 15-16 seconds or until juices run clear and no pink color is visible. Avoid consuming raw or undercooked meat.
- Practice proper hygiene by washing hands, cutting boards, and utensils thoroughly between handling raw meat or poultry and other food items.
- Keep raw foods that will be consumed raw separate from food products from animals. Thoroughly wash these foods before eating.
- Safe Beverage Consumption:
- Drink only pasteurized milk, juice, and cider. Pasteurization helps eliminate harmful bacteria, including STEC.
- Prevention of Fecal-Oral Transmission:
- Avoid engaging in sexual practices that can permit fecal-oral transmission of pathogens. Latex barrier protection, such as condoms, should be used during sexual activity to prevent the spread of STEC and other pathogens to sexual partners.
Adhering to these preventive measures can significantly reduce the risk of STEC infection. It is essential to practice good personal and caregiver hygiene, handle and cook food properly, consume pasteurized beverages, and take precautions to prevent fecal-oral transmission. These measures help protect individuals and prevent the spread of STEC to others.
Treatment Approaches for STEC Infection
- Symptomatic Management: In most cases of uncomplicated STEC infection, symptoms resolve on their own within 4 to 10 days without specific treatment. Supportive care measures are typically employed to manage symptoms and promote recovery. This includes rest, adequate hydration, and maintaining a balanced diet.
- Antibiotic Use: Antibiotic therapy is generally not recommended for STEC infections, as it may not significantly impact the course of the disease and can potentially worsen the outcome. The use of antibiotics can lead to an increased release of Shiga toxins from the bacteria, which can exacerbate the symptoms and increase the risk of complications.
- Monitoring for Hemolytic Uremic Syndrome (HUS): HUS is a severe complication associated with some STEC infections, particularly in children. Close monitoring is essential to promptly identify the development of HUS.
- Management of HUS: If HUS develops, the following aspects require careful monitoring and correction:
- Fluid Status: Maintaining appropriate fluid balance is crucial in HUS management. Fluid intake and output should be monitored, and intravenous fluids may be administered if necessary.
- Electrolyte Disturbances: Imbalances in electrolyte levels, such as potassium and sodium, should be addressed and corrected as needed.
- Acid-Base Abnormalities: Acid-base balance should be monitored and managed appropriately to maintain normal pH levels.
- Blood Pressure: Blood pressure should be closely monitored and managed to prevent complications associated with hypertension.
- Red Blood Cell (RBC) Transfusions: In cases of severe anemia or significant blood loss, red blood cell transfusions may be required.
- Dialysis: Approximately 50% of HUS patients may require dialysis, a treatment modality that helps remove waste products and excess fluids from the blood when the kidneys are not functioning properly.
- Avoidance of Antiperistaltic Agents: The use of antiperistaltic agents, such as diphenoxylate/atropine, is generally not recommended in STEC infections. These medications can slow down intestinal motility, potentially increasing the risk of systemic complications.
Treatment of STEC infections primarily focuses on supportive care, close monitoring, and management of complications if they arise. It is essential to follow medical guidance and seek appropriate medical attention for individualized treatment recommendations based on the severity of the infection and the presence of complications.
FAQ
What is Shiga toxin-producing Escherichia coli (STEC)?
STEC refers to strains of Escherichia coli bacteria that are capable of producing Shiga toxins. These toxins can cause illness in humans, ranging from mild gastrointestinal symptoms to more severe conditions such as hemorrhagic colitis and hemolytic uremic syndrome (HUS).
How is STEC transmitted to humans?
The primary route of transmission is through the ingestion of contaminated food or water. Undercooked ground beef, unpasteurized dairy products, raw fruits and vegetables, and contaminated water sources are common sources of STEC infection. Person-to-person transmission can also occur, especially in settings where proper hygiene practices are not followed.
What are the symptoms of STEC infection?
STEC infection can cause a range of symptoms, including abdominal pain, diarrhea (which may be watery or bloody), nausea, vomiting, and in some cases, fever. The severity of symptoms can vary, with some individuals experiencing mild illness while others develop more severe complications.
What is hemorrhagic colitis?
Hemorrhagic colitis is a condition characterized by bloody diarrhea, severe abdominal pain, and cramping. It is a common manifestation of STEC infection and is caused by the damage to the lining of the colon due to the production of Shiga toxins.
What is hemolytic uremic syndrome (HUS)?
Hemolytic uremic syndrome (HUS) is a severe complication associated with STEC infection, particularly with certain strains such as E. coli O157:H7. It is characterized by the destruction of red blood cells, acute kidney failure, and low platelet count. HUS can be life-threatening, especially in young children and the elderly.
How is STEC infection diagnosed?
Laboratory diagnosis of STEC infection involves testing stool samples for the presence of the bacteria and their toxins. Techniques such as culture, enzyme immunoassays, and molecular methods like polymerase chain reaction (PCR) are used to identify and confirm the presence of STEC in clinical samples.
Is there a specific treatment for STEC infection?
There is no specific treatment for STEC infection. In most cases, the illness is self-limiting, and supportive care is provided to manage symptoms and prevent dehydration. Antibiotics are generally not recommended as they may increase the release of toxins and worsen the course of the disease.
How can STEC infections be prevented?
Prevention of STEC infection involves practicing good hygiene and safe food handling practices. This includes thorough cooking of meat products, avoiding consumption of unpasteurized dairy products and contaminated water, washing hands properly, and maintaining proper sanitation in food preparation areas.
Are there any long-term complications associated with STEC infection?
While most individuals recover fully from STEC infection, some may experience long-term complications. These can include kidney problems, high blood pressure, and neurological issues. Close medical monitoring and follow-up are important, especially for individuals who have developed HUS.
Where are STEC infections most commonly reported?
STEC infections can occur worldwide, but they are more frequently reported in industrialized countries. Outbreaks have been associated with various food sources and environmental exposures. The prevalence of specific STEC serotypes may vary geographically, highlighting the importance of surveillance and preventive measures.
References
- Sandhu KS, Gyles CL. Pathogenic Shiga toxin-producing Escherichia coli in the intestine of calves. Can J Vet Res. 2002 Apr;66(2):65-72. PMID: 11989736; PMCID: PMC226985.
- Paton JC, Paton AW. Pathogenesis and diagnosis of Shiga toxin-producing Escherichia coli infections. Clin Microbiol Rev. 1998 Jul;11(3):450-79. doi: 10.1128/CMR.11.3.450. PMID: 9665978; PMCID: PMC88891.
- https://www.frontiersin.org/articles/10.3389/fcimb.2020.00169/full
- http://conditions.health.qld.gov.au/HealthCondition/condition/14/33/568/shiga-toxin-producing-e-coli-stec-and-haemoly
- https://www.ecdc.europa.eu/en/publications-data/shiga-toxin-producing-escherichia-coli-stec-infection-annual-epidemiological
- https://www.health.gov.au/diseases/shiga-toxin-producing-escherichia-coli-stec-infection
- https://www.chp.gov.hk/en/healthtopics/content/24/23315.html
- https://www.fsis.usda.gov/policy/federal-register-rulemaking/federal-register-notices/expansion-fsis-shiga-toxin-producing
- https://www.federalregister.gov/documents/2022/11/18/2022-25140/expansion-of-fsis-shiga-toxin-producing-escherichia-coli-stec-testing-to-additional-raw-beef
- https://www.testing.com/tests/shiga-toxin-producing-escherichia-coli/
- https://www.iss.it/en/malattie-a-trasmissione-alimentare/-/asset_publisher/bEkyu2xLEXUY/content/shigatoxin-producing-escherichia-coli-stec-
- https://www.albertahealthservices.ca/assets/info/hp/diseases/if-hp-dis-ecoli-stec.pdf
- https://www.thelancet.com/journals/lanmic/article/PIIS2666-5247(22)00223-3/fulltext
- https://www.dshs.texas.gov/e-coli-infection-escherichia-coli-infection
- https://hhs.iowa.gov/cade/disease-information/ecoli
- https://www.health.ny.gov/diseases/communicable/e_coli/stec.htm
- https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/Shiga-toxin-producing-Escherichia-coli.aspx
- https://www.vdh.virginia.gov/epidemiology/epidemiology-fact-sheets/shiga-toxin-producing-escherichia-coli-stec/
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/Shiga-toxin-producing-Ecoli
