Table of Contents
What is White Blood Cell (Leukocytes)?
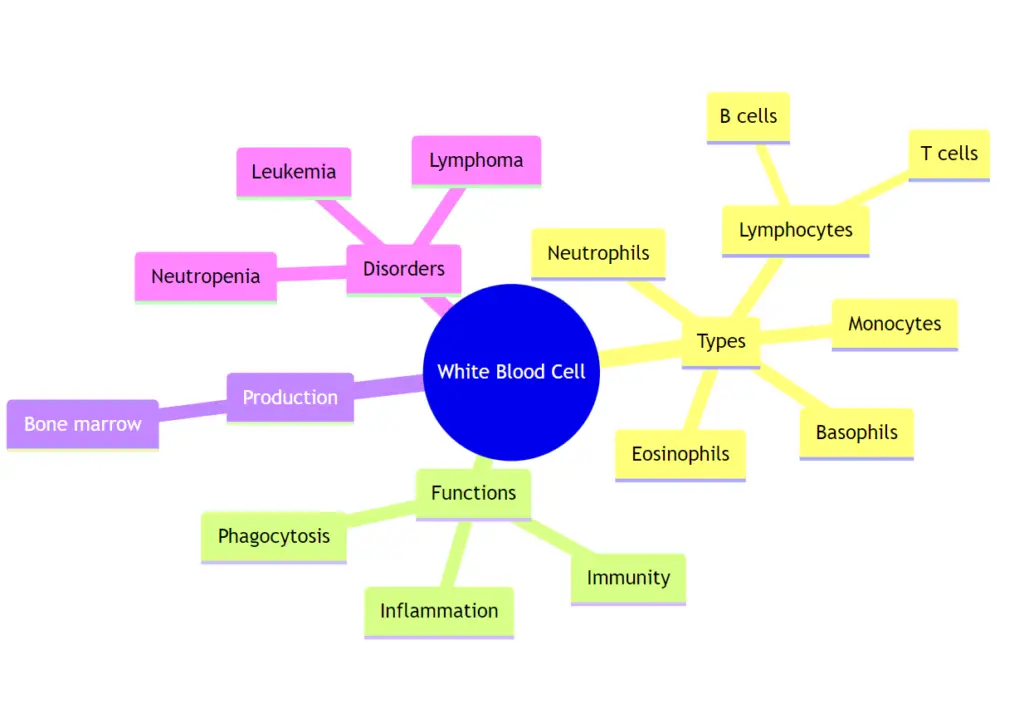
- White blood cells, scientifically termed as leukocytes, are pivotal components of the human immune system, playing a crucial role in safeguarding the body against a myriad of external threats such as pathogens, toxins, and foreign invaders. These cells are not only responsible for combating infectious diseases but also play a role in the removal of dead or malfunctioning cells.
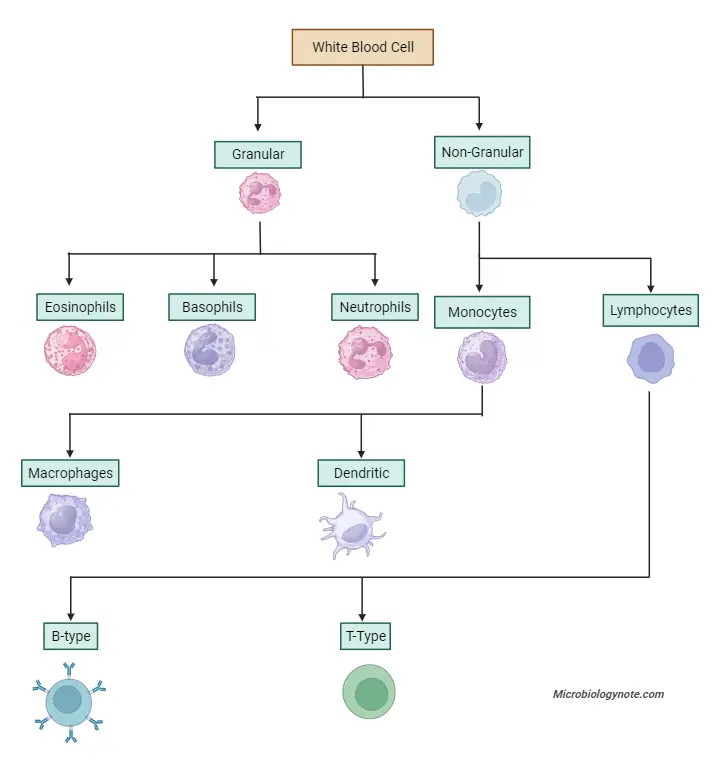
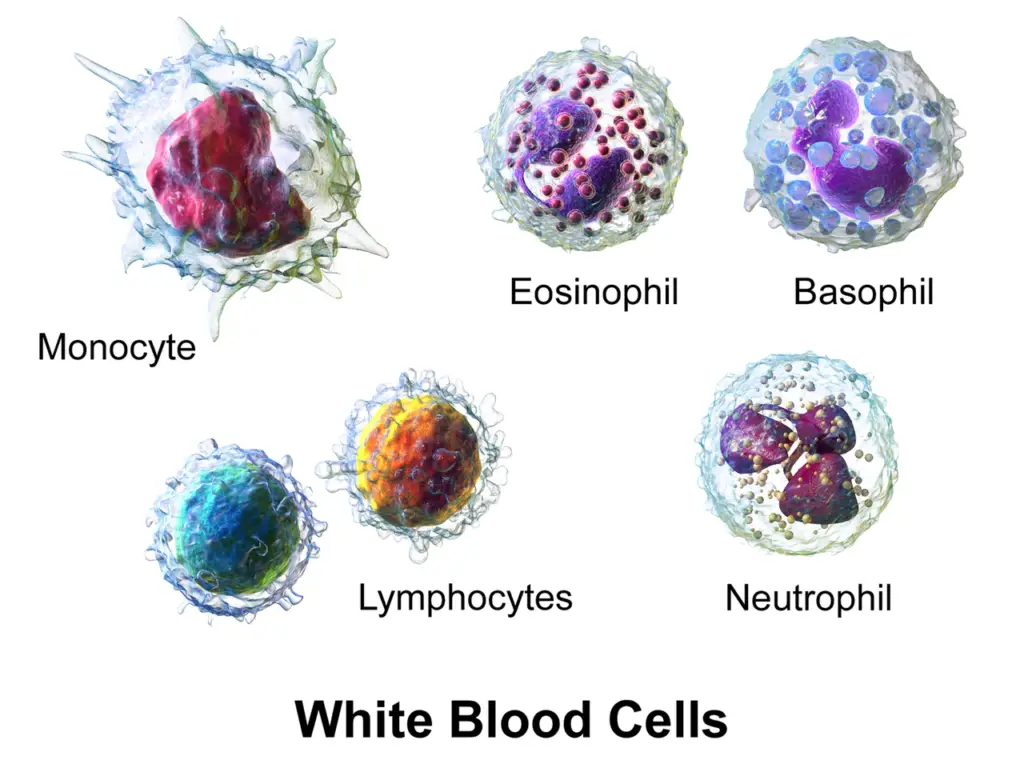
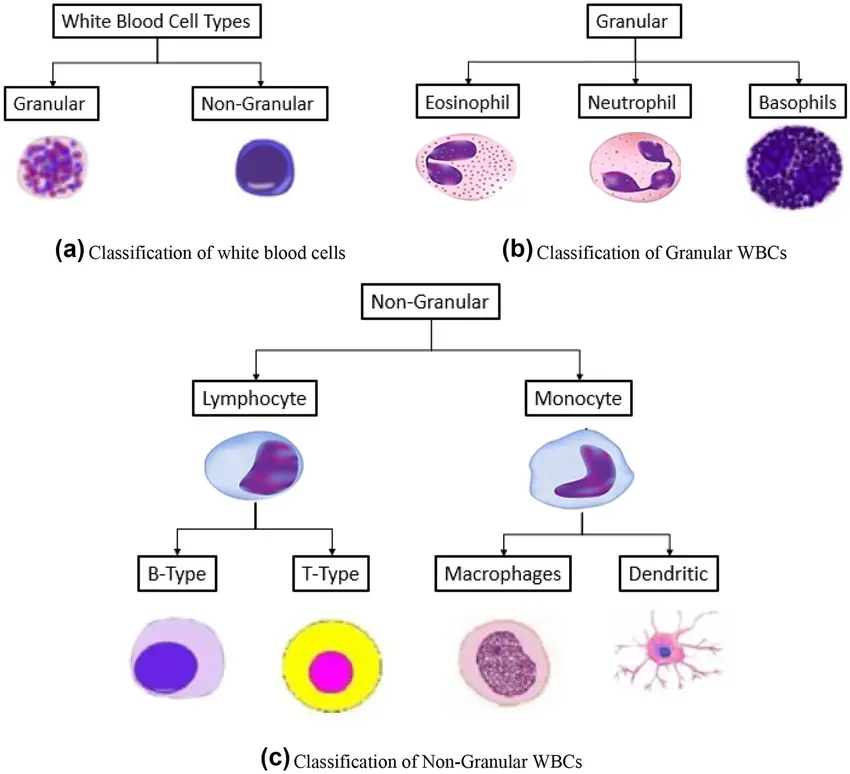
- Leukocytes can be broadly categorized into two primary groups based on their morphological characteristics: granular and non-granular. The granular leukocytes encompass basophils, eosinophils, and neutrophils. On the other hand, the non-granular leukocytes include lymphocytes and monocytes.
- Originating from multipotent hematopoietic stem cells in the bone marrow, all white blood cells undergo a differentiation process that gives rise to various subtypes. These subtypes can be further classified based on their lineage into myeloid and lymphoid cells.
- Myeloid cells comprise neutrophils, eosinophils, mast cells, basophils, and monocytes. Notably, monocytes can be further differentiated into dendritic cells and macrophages, both of which, along with neutrophils, possess phagocytic capabilities.
- Lymphoid cells, or lymphocytes, include T cells (which can be further subdivided into helper T cells, memory T cells, and cytotoxic T cells), B cells (which differentiate into plasma cells and memory B cells), and natural killer cells.
- Historically, the classification of white blood cells was based on their physical attributes, specifically the presence or absence of granules. However, with advancements in scientific understanding, this method of classification has become less prevalent.
- The concentration of leukocytes in the bloodstream serves as a significant indicator of an individual’s health status. Typically, a healthy adult will have a white blood cell count ranging between 4 × 10^9/L and 1.1 × 10^10/L, which translates to 4,000 to 11,000 white blood cells per microliter of blood in the US metrics.
- Although they constitute a mere 1% of the total blood volume, their impact on health is profound, given their central role in immunity.
- An elevation in this count, termed leukocytosis, can be a sign of an active immune response, but if persistent, may indicate pathological conditions such as blood cancers or bone marrow disorders. Conversely, a reduced count, or leukopenia, signifies a compromised immune system, rendering the individual susceptible to infections.
- In conclusion, white blood cells or leukocytes are indispensable to the human immune system, offering a robust defense mechanism against various threats. Their presence, types, and concentration in the bloodstream provide valuable insights into an individual’s health and immune status.
Dfinition of White Blood Cell (Leukocytes)
White blood cells, or leukocytes, are immune system cells responsible for defending the body against infections, pathogens, and foreign invaders. They originate from the bone marrow and can be categorized into various subtypes based on their functions and characteristics.
Formation of White Blood Cell (Leukocytes)
White blood cells, also known as leukocytes, are a fundamental component of the immune system, responsible for defending the body against infections, pathogens, and other foreign invaders. The formation of these cells is a complex and regulated process that occurs primarily in the bone marrow. Here’s an overview of the formation of leukocytes:
- Hematopoiesis:
- Definition: Hematopoiesis is the process by which all blood cells, including leukocytes, are produced from multipotent hematopoietic stem cells in the bone marrow.
- Stages: Hematopoiesis involves several stages of cell differentiation. Hematopoietic stem cells first differentiate into either myeloid or lymphoid progenitor cells. Myeloid progenitors give rise to granulocytes (neutrophils, eosinophils, and basophils), monocytes, and other cell types, while lymphoid progenitors differentiate into lymphocytes (T cells, B cells, and natural killer cells).
- Microenvironment Influence:
- The bone marrow provides a specialized microenvironment, or niche, that supports the growth and differentiation of hematopoietic stem cells. This niche is composed of various stromal cells, extracellular matrix, and signaling molecules.
- Interactions between hematopoietic stem cells and the bone marrow niche regulate the balance between stem cell self-renewal and differentiation.
- Regulation by Cytokines and Growth Factors:
- The differentiation and proliferation of hematopoietic stem cells are tightly regulated by various cytokines and growth factors. For instance, granulocyte colony-stimulating factor (G-CSF) stimulates the production of neutrophils, while erythropoietin (EPO) regulates the production of red blood cells.
- These signaling molecules ensure that the body produces the right number of each type of blood cell based on its current needs.
- Release into the Bloodstream:
- Once formed, mature leukocytes are released into the bloodstream. From here, they can travel to various tissues and organs, where they carry out their immune functions.
- Some leukocytes, like memory T cells, can live for years, while others, like neutrophils, have a lifespan of only a few days.
- Feedback Mechanisms:
- The body has feedback mechanisms in place to regulate the production of leukocytes. For example, during an infection, the increased presence of pathogens can stimulate the bone marrow to produce more white blood cells. Once the infection is cleared, production levels return to normal.
In summary, the formation of white blood cells is a dynamic and regulated process that ensures the body has an adequate defense mechanism against foreign threats. The bone marrow, with its supportive microenvironment and the influence of various growth factors and cytokines, plays a central role in this process.
Structure of White Blood Cell (Leukocytes)
White blood cells, scientifically termed as leukocytes, are integral components of the immune system, playing a central role in safeguarding the body against infections and foreign entities. The structural composition of these cells is intricate and varies depending on their specific type and function. Here’s a comprehensive overview of the structure of leukocytes:
- Cellular Components:
- All leukocytes possess a nucleus encompassing a nucleolus. This nucleus is the control center of the cell, directing its activities.
- The cytoplasm of these cells houses various organelles, including mitochondria, responsible for energy production; the Golgi apparatus, which modifies and packages proteins; and both rough and smooth endoplasmic reticulum, involved in protein synthesis and lipid metabolism, respectively.
- Ribosomes, lysosomes, and peroxisomes are also present, facilitating protein synthesis, digestion of cellular waste, and breakdown of fatty acids, respectively.
- The phospholipid membrane encases the cell, regulating the entry and exit of substances, while centrioles play a role during cell division.
- Communication Capabilities:
- Leukocytes exhibit remarkable intercellular communication abilities. They can transmit and receive signals from neighboring cells, detect anomalous proteins across various tissues, and adhere to both cellular and pathogenic membranes.
- This communication is facilitated by an intricate array of receptors and channels present on the leukocyte membrane.
- Granulocytes:
- Granulocytes are a subset of leukocytes characterized by the presence of specific granules in their cytoplasm.
- Neutrophils: Typically measuring between twelve to fifteen micrometers, they possess a multi-lobed nucleus. Their primary function is to respond to infections, and they have a short lifespan of a few days.
- Eosinophils: These cells are approximately fifteen micrometers in diameter, with two nuclear lobes and prominent granules.
- Basophils: Comparable in size to neutrophils, their nuclei can be double-lobed or exhibit an S-shape.
- Mast cells: These cells are either oval or round and are primarily found in tissues, maturing outside the bloodstream.
- Natural Killer (NK) cells: These are large granular lymphocytes that undergo maturation in lymphoid organs and possess the capability to self-renew.
- Granulocytes are a subset of leukocytes characterized by the presence of specific granules in their cytoplasm.
- Agranulocytes:
- Agranulocytes lack specific granules and are classified into two primary categories:
- Lymphocytes: Comprising T cells and B cells, lymphocytes are unique as they originate in lymphatic tissues. However, their precursor cells are produced in the red bone marrow.
- Monocytes: These cells can be further categorized based on specific protein markers on their membrane into classical, intermediate, and non-classical monocytes. They have the potential to differentiate into macrophages or dendritic cells, playing a pivotal role in phagocytosis and antigen presentation.
- Agranulocytes lack specific granules and are classified into two primary categories:
In essence, the structure of white blood cells is tailored to their specific roles within the immune system, ensuring efficient defense mechanisms against potential threats to the body.
Types of White Blood Cell (Leukocytes)
Leukocytes, commonly referred to as white blood cells, are a fundamental component of the immune system, playing a pivotal role in safeguarding the body against infections and foreign invaders. Based on their structural characteristics, particularly the presence or absence of cytoplasmic granules, leukocytes are categorized into two primary groups:
- Granulocytes:
- Characteristics: Granulocytes are distinguished by the presence of conspicuous, stainable cytoplasmic granules.
- Subtypes:
- Neutrophils: These are the most abundant type of granulocytes, playing a crucial role in the body’s immediate response to infections.
- Eosinophils: These cells are involved in combating parasitic infections and are also associated with allergic reactions.
- Basophils: The least abundant among granulocytes, basophils release histamine during allergic reactions, contributing to inflammation.
- Agranulocytes:
- Characteristics: Agranulocytes lack prominent, stainable cytoplasmic granules and are often referred to as mononuclear leukocytes due to their singular nucleus.
- Subtypes:
- Monocytes: These cells circulate in the bloodstream and can differentiate into macrophages upon entering tissues, playing a role in phagocytosis and antigen presentation.
- Lymphocytes: Lymphocytes are pivotal for the adaptive immune response. They can be further categorized into T cells, which mediate cellular immunity, and B cells, responsible for humoral immunity through antibody production.
In summary, leukocytes can be broadly classified into granulocytes and agranulocytes based on their structural attributes. Each subtype of leukocyte has a unique role in the immune system, ensuring a comprehensive defense mechanism against potential threats to the body.
A. Granulocytes
1. Neutrophil
Neutrophils, a subset of leukocytes or white blood cells, serve as the immune system’s primary responders, offering immediate defense against infections.
Morphological Characteristics:
- Neutrophils, typically spherical in their resting state, possess the ability to alter their shape to combat infections. They measure between 12-14µm in diameter.
- A distinguishing feature of neutrophils is their polymorphonuclear appearance, attributed to their multilobed nuclei.
- In females, a unique ‘drum-stick’ formation is observed in approximately 3% of neutrophil nuclei, signifying the presence of the inactive X chromosomes’ sex chromatin.
- While inherently clear, neutrophils undergo a color transformation upon interaction with dyes, rendering them visible under microscopic examination. Their cytoplasm contains fine, neutrophilic granules, which, when subjected to Leishman staining, exhibit a violet hue.
Location and Lifespan:
- Originating from hematopoiesis within the bone marrow, neutrophils are subsequently released into the peripheral blood. They circulate for a duration of 7-10 hours prior to migrating into tissues. Within these tissues, their lifespan is relatively short, spanning only a few days.
Prevalence:
- Neutrophils are the predominant white blood cell type, constituting 40-75% of the total white blood cell count in adults.
- A complete blood count typically includes a neutrophil count, with the standard range being 2500-7500 neutrophils per µl of blood.
Defense Mechanisms:
- Neutrophils are drawn to inflammatory sites by various chemotactic factors produced during inflammation.
- Their primary role involves defending the body against microbial invaders. This is achieved through phagocytosis of these microbes and smaller particles in circulation, and similar actions in other tissues post-extravasation.
- Neutrophils, when actively phagocytic, can enzymatically reduce oxygen to generate reactive oxygen species, including superoxide radicals and hydrogen peroxide. This process likely facilitates bacterial destruction by activating certain granule contents.
- Post-phagocytosis, neutrophils undergo apoptosis. The resultant dead neutrophils, combined with bacteria, tissue debris, and interstitial fluid, constitute the characteristic green-yellow pus observed in infected tissues.
Conditions Impacting Neutrophils:
- Neutropenia: A condition characterized by abnormally low neutrophil counts, leading to recurrent infections and inflammation. Potential causes include cancer treatments, infections (like hepatitis, tuberculosis, sepsis, Lyme disease), bone marrow disorders, vitamin deficiencies, and autoimmune diseases.
- Neutrophilia: This condition, also termed neutrophilic leukocytosis, is marked by elevated neutrophil counts. It can result from bacterial infections, inflammation, injuries, certain drug reactions, or premature release of immature neutrophils from the bone marrow into the bloodstream.
Functional Role:
- Neutrophils are adept at migrating to infection sites, where they neutralize or destroy microorganisms through phagocytosis and enzyme release.
- By bolstering the body’s immune response, neutrophils play an indispensable role in maintaining health and combating infections.
2. Eosinophil
Eosinophils, classified under granulocytes, are a subset of leukocytes or white blood cells. They play a pivotal role in the immune system, actively participating in combating diseases and amplifying inflammation at sites of infection.
Morphological Characteristics:
- Eosinophils are motile cells, typically measuring between 5-15µm in diameter. Despite their crucial role, they are relatively scarce in normal blood, with counts ranging from 100 to 400 per µl.
- Their nucleus is bifurcated, often appearing U-shaped or resembling spectacles in blood smears.
- The cytoplasm of eosinophils is characterized by its coarse, acidophilic granules, which are integral to their function.
Location and Lifespan:
- Eosinophils originate in the bone marrow and subsequently migrate to various tissues. They are predominantly located in the connective tissues of the stomach and intestines.
- Their overall lifespan is brief, spanning a few days. Of this duration, approximately 10 hours are spent circulating in the bloodstream, with the remaining time in extracellular tissues.
Prevalence:
- Eosinophils constitute a minor fraction of white blood cells, accounting for 1-4% of the total count.
- Their count is an integral component of a complete blood count, with the standard range being 100 to 400 eosinophils per µl of blood.
Defense Mechanisms:
- Eosinophil levels typically surge during worm infections and specific allergic disorders. It is postulated that eosinophils evolved primarily to counteract parasitic and cancerous cells.
- They possess surface receptors for Ig E, which, upon binding to Ig E-antigen complexes, initiate phagocytosis and granule release.
- Eosinophils release a plethora of toxic molecules from their granules, such as eosinophil cationic protein and major base proteins, which exhibit antiparasitic properties. Additionally, they release histaminase, instrumental in mitigating the inflammatory outcomes of mast cell degranulation.
Conditions Impacting Eosinophils:
- Eosinopenia: This condition is marked by eosinophil counts falling below the standard range. Common causes include Cushing’s syndrome and sepsis.
- Eosinophilia: Contrarily, eosinophilia is characterized by elevated eosinophil counts. Potential triggers encompass alcohol intoxication, allergies, gastrointestinal disorders, leukemia, excessive cortisol production, and parasitic infections.
Functional Role:
- Eosinophils are multifunctional. Their roles encompass cell destruction, migration to inflamed regions, substance entrapment, antibacterial and antiparasitic activities, participation in immediate allergic reactions, and modulation of inflammatory responses.
In summary, eosinophils, though present in limited numbers, play a multifaceted role in the immune system, ensuring the body’s robust defense against various threats.
3. Basophils
Basophils, classified under granulocytes, are a subset of leukocytes. These cells, albeit smaller than other granulocytes, are relatively larger in size and play a pivotal role in the body’s defense mechanisms against various pathogens, including bacteria, fungi, viruses, allergens, and parasites. Additionally, basophils are instrumental in releasing enzymes that deter blood clotting and enhance blood circulation.
Morphological Characteristics:
- Basophils are spherical cells, typically measuring between 10-14µm in diameter.
- Their defining characteristic is the presence of large, prominent basophilic granules. Additionally, they possess a kidney-shaped nucleus, further distinguishing them from other granulocytes.
Location and Lifespan:
- Basophils originate and mature in the bone marrow. Post-maturation, they circulate in the bloodstream and, upon detecting injury, migrate to the affected tissue to facilitate healing.
Prevalence:
- Basophils constitute a minor fraction of the total leukocyte count, accounting for merely 0.5 to 1%. The standard count for basophils ranges from 25-200 per µl of blood.
Defense Mechanisms:
- The granules within basophils house various inflammatory agents, including heparin and histamine.
- Basophils are equipped with high-affinity membrane receptors for Ig E and are coated with Ig E antibodies. When these antibodies bind to their corresponding antigens, it instigates the degranulation of cells. This process results in vasodilation, increased vascular permeability, and the attraction of other granulocytes, manifesting symptoms of immediate hypersensitivity, such as those observed in allergic rhinitis.
- Histamine, released by basophils, augments blood flow by dilating blood vessels, thereby aiding in the healing of the affected region. Concurrently, heparin acts as an anticoagulant, preventing rapid blood clotting.
Conditions Impacting Basophils:
- Basopenia: This condition is characterized by a deficiency in basophil production. Hyperthyroidism is often associated with basopenia.
- Basophilia: Contrarily, basophilia denotes an overproduction of basophils. Conditions such as leukemia, polycythemia vera, myelofibrosis, hypothyroidism, and certain autoimmune diseases can lead to basophilia.
Functional Role:
- Basophils serve as the body’s protective shield against external threats, including pathogens, parasites, and allergens.
- The enzymes contained within basophil granules, upon release, enhance blood circulation and act as anticoagulants, preventing premature blood clotting.
In summary, basophils, though present in limited numbers, play a multifaceted role in the immune system, ensuring the body’s robust defense against various threats and facilitating healing processes.
B. Agranulocytes leukocytes
1. Monocytes
Monocytes, a subset of leukocytes or white blood cells, are the most substantial in size among their counterparts. These cells circulate in the blood and tissues, actively seeking and neutralizing microorganisms, and facilitating the removal of infected cells.
Morphological Characteristics:
- Monocytes are notably larger, approximately twice the size of red blood cells, measuring between 15-20 µm in diameter.
- Despite their size, they constitute a minor fraction of the total white blood cell count, ranging from 2-8% with a typical cell count of 100-700 per µl.
- Microscopically, monocytes exhibit a bilobed nucleus that is dynamic in shape, often appearing oval, kidney, or horse-shaped. This nucleus is suspended in the cytoplasm, a fluid that lacks granules in monocytes.
Location and Lifespan:
- Monocytes originate in the bone marrow. Post-maturation, they traverse through the bloodstream, migrating to tissues where they collaborate with other immune cells to defend against infections.
Defense Mechanisms:
- Monocytes are inherently phagocytic, equipped with numerous lysosomes. Their phagocytic activity is initiated upon recognizing opsonized materials.
- These cells express class II MHC antigens, facilitating their interaction with other immune cells.
- A significant portion of monocytes is believed to transition from the bone marrow to peripheral tissues, differentiating into macrophages and dendritic cells. Specific subsets of monocytes may target inflamed tissues.
- Dendritic cells identify antigens from invasive pathogens, subsequently releasing cytokines. These proteins signal other white blood cells to converge at the infection site and neutralize the threat.
- Macrophages, on the other hand, engulf and neutralize microorganisms using toxic enzymes. They also play a role in clearing dead cells from tissues.
Conditions Impacting Monocytes:
- Monocytopenia: This condition arises when monocyte counts plummet. Common triggers include a reduction in leukocytes, aplastic anemia, blood infections, burn injuries, HIV, and adverse reactions to chemotherapy.
- Monocytosis: Conversely, monocytosis denotes elevated monocyte levels. Potential causes encompass autoimmune diseases (e.g., lupus, rheumatoid arthritis), blood disorders, cancers, cardiovascular diseases, infections, and other inflammatory conditions.
Functional Role:
- Monocytes serve as the body’s vanguard, either directly neutralizing infectious agents or signaling other blood cells to assist in the defense. Their actions bolster the body’s immune response, ensuring a robust defense against various threats.
In essence, monocytes, though present in limited numbers, play a multifaceted role in the immune system, ensuring the body’s resilience against pathogens and facilitating the healing process.
2. Lymphocytes
Lymphocytes, a pivotal subset of white blood cells, are integral to the body’s immune defenses. Their prevalence in adulthood makes them the second most abundant type of white blood cell. Lymphocytes are instrumental in safeguarding the body against infections and diseases.
Morphological Characteristics:
- Lymphocytes are characteristically larger than red blood cells, with their size ranging from 6-16µm. The majority of circulating lymphocytes measure between 6-8 µm in diameter.
- These cells are distinguished by a prominent nucleus that occupies most of the cell’s volume, leaving minimal cytoplasm. Notably, the cytoplasm lacks granules.
Origins and Distribution:
- Lymphocytes originate in the bone marrow. Post-maturation, they disseminate into the bloodstream and populate the entire lymphatic system.
- Some lymphocytes migrate to the thymus gland, differentiating into T cells, while others venture to lymph nodes and organs, maturing into B cells.
Prevalence and Lifespan:
- Lymphocytes typically range between 1500 to 2700 per µl of blood, accounting for 20-30% of the total white blood cell count.
- Their lifespan is variable, spanning from a few days to several years. This extended longevity is crucial for sustaining immunological memory.
Defensive Mechanisms:
- Lymphocytes are the memory keepers of the immune system. They catalog every antigen they encounter, ensuring a swift response upon re-exposure. This memory function underpins the rationale for vaccinations and explains the lifelong immunity to diseases like chickenpox after a single episode.
- T cells are multifunctional. Cytotoxic T cells, for instance, latch onto antigens on infected cells, subsequently destroying them. Helper T cells, on the other hand, assist B cells in antibody production.
- B cells are equipped with antigen receptors. Upon antigen binding, B cells differentiate into memory or plasma cells. Plasma cells generate antibodies specific to the encountered antigen, leading to the primary immune response. Subsequent encounters with the same antigen activate memory B cells, which rapidly proliferate and produce the appropriate antibodies, constituting the secondary immune response.
Conditions Impacting Lymphocytes:
- Lymphocytopenia: A condition characterized by reduced lymphocyte levels. Potential causes include flu, mild infections, viral infections, tuberculosis, autoimmune disorders, blood diseases, and treatments like radiation and chemotherapy.
- Lymphocytosis: This condition denotes elevated lymphocyte counts. It can result from various factors, including viral infections, syphilis, mononucleosis, tuberculosis, hypothyroidism, and certain blood cancers.
Functional Roles:
- T cells are adept at identifying and eliminating infected and tumorous cells. They also modulate the broader immune response.
- B cells are antibody factories. They produce antibodies tailored to neutralize specific viruses, bacteria, and other foreign antigens, fortifying the body’s defenses.
In summary, lymphocytes are indispensable components of the immune system, orchestrating a coordinated defense against a myriad of pathogens and ensuring the body’s resilience against recurrent threats.
WBC Normal Range
White Blood Cells (WBC), also known as leukocytes, play a pivotal role in the immune system, defending the body against infections and diseases. The concentration of these cells in the bloodstream is a crucial indicator of one’s health and can provide insights into potential medical conditions.
WBC Normal Range Based on Age:
- Newborn: The immune system of a newborn is still developing, and as a result, their WBC count is typically higher. The standard range for a newborn is between 13,000 to 38,000 cells per cubic millimeter of blood.
- 2-week-old baby: As the infant grows, there is a noticeable decrease in the WBC count, reflecting the ongoing development and maturation of their immune system. For a two-week-old baby, the WBC count usually ranges from 5,000 to 28,000 cells per cubic millimeter.
- Adult: In adulthood, the immune system is fully developed and functions at its peak. The WBC count stabilizes, and the standard range for adults is between 4,500 to 11,000 cells per cubic millimeter of blood.
It’s essential to understand that these ranges are general guidelines. Various factors, including overall health, lifestyle, and genetics, can influence an individual’s WBC count. Regular health check-ups and blood tests can ensure that one’s WBC count remains within the standard range, signaling a healthy immune system. If deviations are observed, it’s crucial to consult with a healthcare professional for a comprehensive assessment.
Low White Blood Cell Counts
White blood cells (WBCs), or leukocytes, are the body’s primary defense mechanism against infections and diseases. A decrease in the number of these cells can compromise the immune system, making the body more susceptible to infections.
Potential Causes of Low WBC Count:
- Severe Infections: Certain infections can suppress bone marrow function, leading to a decrease in WBC production.
- Bone Marrow Disorders: Conditions such as aplastic anemia, or the invasion of bone marrow by blood cancers or metastatic cancer, can hinder the production of WBCs. Additionally, certain drugs or chemicals may damage the bone marrow, affecting its ability to produce WBCs.
- Autoimmune Diseases: Diseases like lupus can cause the body to attack its own WBCs, leading to a reduced count.
- Splenic Sequestration: In some cases, the spleen may accumulate and trap white blood cells, reducing their number in the bloodstream.
Symptoms Associated with Low WBC Count:
While a low WBC count itself might not manifest noticeable symptoms, the resulting vulnerability to infections can lead to:
- Fever
- Persistent cough
- Pain or frequent urination
- Presence of blood in stools
- Diarrhea
- Areas of redness, swelling, or warmth indicating an infection site
Chemotherapy and WBC Count:
Chemotherapy, a common treatment for cancer, can have a profound impact on the WBC count, particularly on neutrophils, a type of WBC. This condition, termed chemotherapy-induced neutropenia, heightens the risk of severe infections. Neutrophils act as the immune system’s first line of defense. When their count is diminished due to chemotherapy, the body becomes less equipped to fend off infections. Consequently, even bacteria that are typically harmless can lead to severe illnesses in individuals with neutropenia.
In conclusion, maintaining an optimal WBC count is crucial for a robust immune response. Any significant deviation from the normal range warrants medical attention to identify the underlying cause and initiate appropriate treatment.
Functions of White Blood Cells
White blood cells (WBCs), also known as leukocytes, are essential components of the immune system. Their primary function is to defend the body against infections, foreign invaders, and other harmful substances. Here’s a detailed overview of the functions of various types of white blood cells:
- Neutrophils:
- Primary Responders: They are the first to arrive at the site of an infection.
- Phagocytosis: Neutrophils engulf and digest bacteria and fungi.
- Formation of Neutrophil Extracellular Traps (NETs): They can release a web-like structure to trap and kill pathogens.
- Lymphocytes:
- B Cells: Produce antibodies that are specific to the antigen they encounter. These antibodies help in neutralizing pathogens.
- T Cells:
- Helper T Cells: Assist other white blood cells in immunologic processes, including maturation of B cells into plasma cells and memory B cells.
- Cytotoxic T Cells: Attack and destroy infected cells.
- Natural Killer (NK) Cells: Detect and destroy cells that are infected with viruses or have turned cancerous.
- Monocytes:
- Phagocytosis: Engulf and digest cellular debris, foreign substances, microbes, and cancer cells.
- Differentiation: Can differentiate into macrophages and dendritic cells in tissues to combat infections.
- Macrophages:
- Phagocytosis: Engulf and digest pathogens and dead cells.
- Antigen Presentation: Display fragments of pathogens to T cells, facilitating their activation.
- Dendritic Cells:
- Antigen Presentation: Capture and present antigens to adaptive immune cells, initiating an immune response.
- Eosinophils:
- Parasitic Infections: Primarily involved in combating multicellular parasites.
- Modulation of Allergic Inflammatory Responses: Play a role in allergic reactions, such as asthma.
- Basophils:
- Allergic Responses: Release histamine, contributing to inflammation and allergic reactions.
- Protection Against Parasites: Produce substances that can combat certain parasites.
- Mast Cells:
- Release of Histamine: Involved in wound healing and defense against pathogens.
- Allergic Responses: Play a key role in causing allergic symptoms.
In summary, white blood cells are the body’s primary defense mechanism against infections, diseases, and foreign invaders. They work in a coordinated manner to ensure the body remains healthy and free from harmful substances.
Difference Between Basophils, Eosinophils, and Neutrophils
White blood cells, or leukocytes, are crucial components of the immune system, playing distinct roles in defending the body against pathogens. Among these, basophils, eosinophils, and neutrophils are types of granulocytes, each with unique characteristics and functions. Here’s a comparative analysis of these three cell types:
- Role in Immune System:
- Basophils: Primarily assist in diagnosing autoimmune diseases and blood-related disorders. They play a role in allergic reactions and inflammation.
- Eosinophils: Predominantly combat allergies and certain diseases, especially parasitic infections.
- Neutrophils: Act as the frontline defense, providing a rapid immune response against foreign particle invasions, including bacterial infections.
- Nucleus Structure:
- Basophils: Possess a multi-lobed nucleus.
- Eosinophils: Characterized by a bean-shaped nucleus.
- Neutrophils: Typically have a two or bilobed nucleus.
- Life Span:
- Basophils: Survive for approximately 60–70 hours.
- Eosinophils: Have a shorter life span, ranging from 8–12 hours.
- Neutrophils: Their life span varies widely, from about 5 to 90 hours.
- Cell Size:
- Basophils: Measure around 10–14 micrometres in diameter.
- Eosinophils: Slightly larger, with a diameter of about 12–17 micrometres.
- Neutrophils: Smallest among the three, with a diameter of approximately 8.86 micrometres.
- Associated Disorders:
- Basophils: Disorders include hypothyroidism and leukopenia (a condition characterized by a low level of white blood cells).
- Eosinophils: Eosinophilia denotes a high level of eosinophils, often seen in allergic reactions or parasitic infections.
- Neutrophils: Neutropenia refers to a low neutrophil count, increasing susceptibility to infections. Conversely, leukocytosis indicates a high neutrophil count, often seen in acute bacterial infections.
In summary, while basophils, eosinophils, and neutrophils are all integral to the immune system, they have distinct roles, structures, and associated disorders. Recognizing these differences is crucial for medical diagnostics and understanding immune responses.
| Characteristics | Basophils | Eosinophils | Neutrophils |
|---|---|---|---|
| Role | Helps in diagnosing autoimmune diseases and blood-related disorders | Fights against allergies and diseases | Provides immune response against foreign particle attacks |
| Nucleus | Multi-lobed | Bean-shaped | Two or bilobed |
| Life Span | 60–70 hours | 8–12 hours | 5–90 hours |
| Size (Diameter) | 10–14 micrometres | 12–17 micrometres | 8.86 micrometres |
| Disorders | Hypothyroidism, Leukopenia (low level) | Eosinophilia (high level) | Leukocytosis (high level), Neutropenia (low level) |
Difference Between B Cells and T Cells
| Characteristics | B Cells | T Cells |
|---|---|---|
| Site of Maturation | Originate and mature in the bone marrow | Originate in the bone marrow and mature in the thymus |
| Also Known As | B lymphocytes | T lymphocytes |
| Position | Present outside the lymph nodes | Present inside the lymph nodes |
| Life Span | Shorter life span | Longer life span compared to B cells |
Quiz
Which of the following is NOT a type of white blood cell?
a) Erythrocyte
b) Neutrophil
c) Lymphocyte
d) Basophil
Which white blood cell is primarily responsible for producing antibodies?
a) Monocyte
b) Eosinophil
c) B lymphocyte
d) Neutrophil
Which cell is the largest type of white blood cell?
a) Lymphocyte
b) Monocyte
c) Basophil
d) Neutrophil
Which white blood cell is most numerous in the bloodstream?
a) Neutrophil
b) Eosinophil
c) Basophil
d) Lymphocyte
Which white blood cell is primarily involved in allergic reactions?
a) Neutrophil
b) Basophil
c) Lymphocyte
d) Monocyte
Which cell matures in the thymus gland?
a) B lymphocyte
b) T lymphocyte
c) Monocyte
d) Eosinophil
Which white blood cell has granules that stain red with eosin dye?
a) Neutrophil
b) Basophil
c) Eosinophil
d) Lymphocyte
Which white blood cell plays a role in the destruction of parasitic worms?
a) Neutrophil
b) Basophil
c) Eosinophil
d) Monocyte
Which cell is responsible for phagocytosis and later becomes a macrophage in tissues?
a) Lymphocyte
b) Neutrophil
c) Eosinophil
d) Monocyte
Which white blood cell is involved in the body’s immune response against viral infections and tumor cells?
a) Natural Killer Cell
b) Basophil
c) Eosinophil
d) Neutrophil
FAQ
What are white blood cells (leukocytes)?
White blood cells, or leukocytes, are cells of the immune system that are involved in protecting the body against both infectious diseases and foreign invaders.
How many types of white blood cells are there?
There are five main types of white blood cells: neutrophils, lymphocytes, monocytes, eosinophils, and basophils.
What is the primary function of white blood cells?
The primary function of white blood cells is to combat infections by eliminating pathogens and responding to foreign substances in the body.
Where are white blood cells produced?
White blood cells are produced in the bone marrow, which is the soft tissue inside bones.
What is leukopenia?
Leukopenia is a condition where there is a decrease in the number of white blood cells in the blood, which can increase the risk of infections.
What is leukocytosis?
Leukocytosis refers to an increase in the number of white blood cells in the blood, often due to infections, inflammation, or other conditions.
How do white blood cells recognize foreign invaders?
White blood cells recognize foreign invaders through specific receptors on their surface that can identify and bind to pathogens or other foreign substances.
What role do white blood cells play in allergies?
Certain white blood cells, like basophils and eosinophils, play a role in allergic reactions. They release substances like histamines that cause symptoms of allergies.
How can I increase my white blood cell count?
A healthy diet, adequate sleep, managing stress, and avoiding known risk factors like smoking can help maintain a healthy white blood cell count. In certain cases, medications or treatments might be prescribed to increase the count.
Why is a white blood cell count test important?
A white blood cell count test helps determine the body’s ability to fight infections, assess the function of the immune system, and diagnose diseases and conditions like leukemia, infections, or an immune system disorder.
References
- White Blood Cells. (2012). Clinical Veterinary Advisor, 972. doi:10.1016/b978-1-4160-9979-6.00455-4
- Valenciano, A. C., Cowell, R. L., Rizzi, T. E., & Tyler, R. D. (2014). White Blood Cells. Atlas of Canine and Feline Peripheral Blood Smears, 111–213.e2. doi:10.1016/b978-0-323-04468-4.00003-3
- Al-Shura, A. N. (2020). Leukocytes. Advanced Hematology in Integrated Cardiovascular Chinese Medicine, 35–39. doi:10.1016/b978-0-12-817572-9.00006-9
- Peculiarities of blood formation from bone marrow in secondary chronic inflammation on the background of mesenchymal stem cells
- Dynamic Microtubule Arrays in Leukocytes and Their Role in Cell Migration and Immune Synapse Formation
- Genetic Variation of a −176g>c Interleukin-6 Correlated with White Blood Cells Count in Obesity of Indonesia
- https://biologydictionary.net/white-blood-cell/
- https://www.verywellhealth.com/understanding-white-blood-cells-and-counts-2249217
- https://teachmephysiology.com/immune-system/cells-immune-system/white-blood-cells/


