Table of Contents
What is Candida albicans?
Candida albicans is a yeast that is typically found as a natural inhabitant within the human body, specifically in the gut flora. Besides being present in the gastrointestinal tract, it is also commonly detected in the mouth of 40–60% of healthy adults. In most situations, C. albicans remains a harmless commensal organism. However, under certain conditions, especially in individuals with compromised immune systems, it can turn pathogenic. Therefore, it is classified as an opportunistic pathogenic yeast.
One of the primary infections caused by this fungus is candidiasis. This condition arises from an overgrowth of the fungus. Candidiasis is particularly prevalent in patients with HIV. Then, it’s worth noting that C. albicans is the predominant fungal species found in biofilms, which can form on implanted medical devices or directly on human tissue. Besides C. albicans, other species like C. tropicalis, C. parapsilosis, and C. glabrata also contribute to candidiasis, accounting for 50–90% of all human cases. The severity of infections caused by C. albicans is evident from the reported 40% mortality rate in patients with systemic candidiasis. Furthermore, studies suggest that the fungus has the potential to cross the blood-brain barrier in mice, indicating its ability to cause more extensive damage than previously thought.
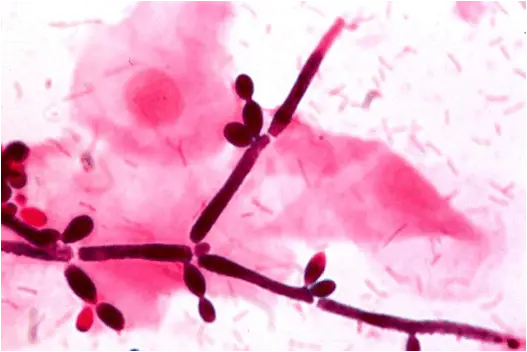
In the realm of scientific research, C. albicans serves as a model organism for studying fungal pathogens. It exhibits dimorphism, meaning it can grow in both yeast and filamentous forms. Additionally, it presents various morphological phenotypes, including the opaque, GUT, and pseudohyphal forms. Contrary to earlier beliefs, C. albicans is not strictly diploid. It can exist in both haploid and tetraploid stages, with the latter resulting from mating of diploid cells when they adopt the opaque form. The genome of this organism is approximately 29 Mb in size, and a significant portion, up to 70%, of its protein-coding genes remains uncharacterized.
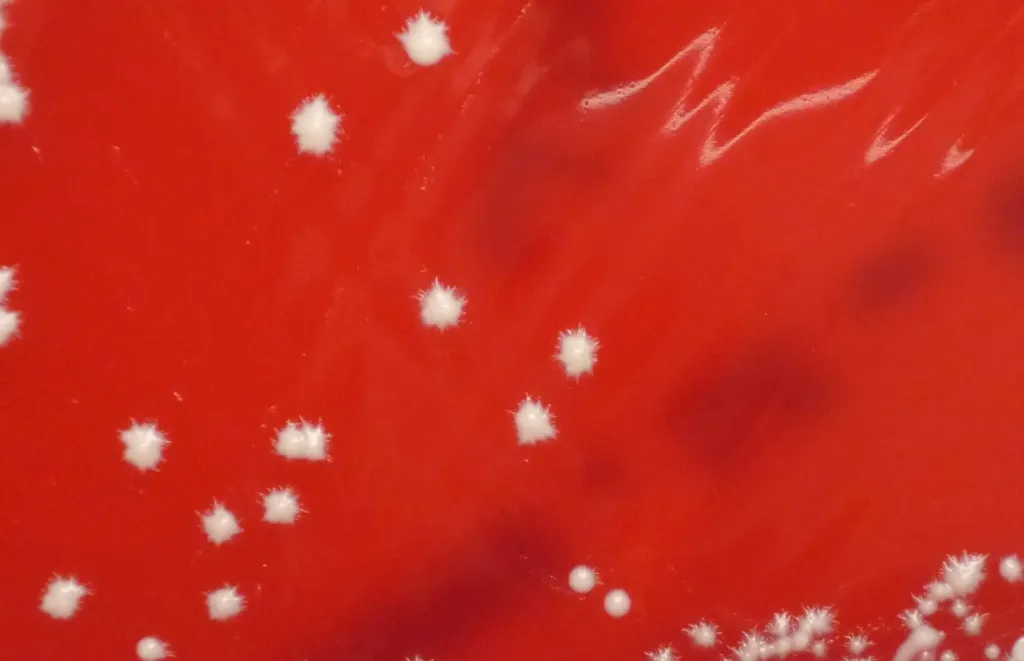
For laboratory studies, C. albicans can be easily cultured. The choice of media can influence its morphological state, emphasizing the importance of the medium in specific research contexts. One such specialized medium is CHROMagar Candida, which aids in distinguishing between different Candida species. In conclusion, Candida albicans is a versatile organism, playing roles both as a commensal member of the human microbiota and as a potential pathogen, making it a focal point in medical and scientific research.

Requirements for Candida albicans gram stain
1. Compound Light Microscope: A compound light microscope is a primary tool in this procedure. It is used to magnify and observe the stained Candida albicans cells. The microscope allows for the differentiation of the cells based on their color after staining, providing insights into their classification.
2. Reagents and Glasswares: For the gram staining process, specific reagents and glasswares are indispensable. These include:
- Bunsen Flame: This is used to heat-fix the smear onto the slide, ensuring the cells adhere to the slide and are killed, making them ready for staining.
- Wire Loop: A sterilized wire loop is employed to pick and smear the Candida albicans culture onto the slide.
- Clean Grease-free Slides: These are the platforms on which the smear is placed. It’s crucial that they are clean and free from grease to ensure proper adherence and staining of the specimen.
- Marker Pen: This is used to label the slides, ensuring proper identification and organization.
- Crystal Violet (Basic dye): This is the primary stain used in the gram staining process. It imparts a purple color to all cells initially.
- Gram’s Iodine (Mordant): This is applied after the crystal violet and functions to fix the stain, ensuring it binds firmly to the cell structures.
- 95% Ethanol (Decolorizing Agent): This agent is crucial in the differentiation process. It removes the crystal violet from certain cells, based on the nature of their cell walls.
- 1% Safranin: This is the counterstain. Cells that have been decolorized by the ethanol will take up this red dye, providing a contrast to the purple cells that retained the crystal violet.
3. Specimen: Lastly, the specimen, in this case, is the growth of Candida albicans on Sabouraud Dextrose Agar (SDA). This culture provides the cells that will be stained and observed under the microscope.
Smear Preparation
- Slide Selection: The first step in smear preparation is the selection of a clean, grease-free slide. The cleanliness of the slide is paramount as any contaminants can interfere with the staining process and lead to inaccurate results. Therefore, ensuring the slide is free from grease and other residues is essential for the clarity and accuracy of the subsequent microscopic examination.
- Collection of the Specimen: Using an inoculating loop, a small portion of the microbial colony is gently touched to collect a sample. The loop must not dig into the agar or medium, as this can introduce extraneous material into the smear. The aim is to collect a thin, even layer of the organism.
- Smearing the Specimen: The collected specimen is then spread on the slide in a thin, even layer. This step is crucial as a thick smear can prevent proper penetration of stains and may also result in clumping of cells, making individual cells difficult to discern under the microscope.
- Air Drying: Once the smear is prepared, it is allowed to air dry. This step ensures that the water content from the sample evaporates, leaving behind the microbial cells adhered to the slide. Rushing this step or using artificial means to speed up drying can distort the cells, affecting the quality of the smear.
- Heat Fixation: After the smear is completely dry, it is subjected to heat fixation. Holding the slide at one end, it is swiftly passed over the flame of a Bunsen burner two to three times. The purpose of this step is twofold: firstly, it kills the microbial cells, ensuring safety during subsequent handling. Secondly, it causes the cells to adhere firmly to the slide, preventing them from being washed away during the staining process.
Procedure of Gram Staining of Candida albicans
- Application of Primary Stain: Begin by covering the smear with crystal violet, a basic dye. Allow this stain to remain on the smear for one minute. The function of this step is to impart a purple color to all bacterial cells, regardless of their Gram classification.
- Rinsing: After the allotted time, the smear is gently rinsed under tap water. This step ensures the removal of excess crystal violet that hasn’t been taken up by the bacterial cells.
- Application of Mordant: Cover the smear with Gram’s iodine and let it stand for one minute. Gram’s iodine acts as a mordant, which means it forms a complex with the crystal violet, ensuring the dye binds firmly to the bacterial cell structures.
- Second Rinsing: The smear is then gently rinsed again under tap water to remove any unbound iodine.
- Decolorization: The smear is decolorized using 95% alcohol. This step is crucial in the differentiation process. Gram-positive bacteria will retain the crystal violet-iodine complex due to the nature of their cell walls, while Gram-negative bacteria will lose this color.
- Third Rinsing: After decolorization, the smear is again gently rinsed under tap water. This step ensures the removal of excess alcohol and any unbound dye.
- Counterstaining: The smear is then covered with safranin, a red counterstain, for one minute. Safranin imparts a red color to the Gram-negative bacteria, which have been decolorized in the previous steps, providing a contrast to the purple Gram-positive bacteria.
- Final Rinsing and Drying: The smear is rinsed one final time under tap water and then allowed to air dry. This step ensures the removal of excess safranin and prepares the smear for microscopic examination.
- Microscopic Examination: Initially, observe the smear under the low power (10X) objective to get an overview. Then, for detailed observation and differentiation of bacterial cells, switch to the oil immersion (100X) objective.
Result Interpretation of Gram Stain
- Gram-Positive Bacteria: Upon completion of the Gram stain procedure, if the bacterial cells appear purple or violet in color under the microscope, they are classified as Gram-positive. This coloration indicates that these bacteria possess a thick layer of peptidoglycan in their cell walls. Therefore, they retain the crystal violet-iodine complex during the decolorization step, resulting in a violet appearance. The presence of Gram-positive bacteria can be indicative of certain types of infections and can guide the choice of antibiotics in clinical scenarios.
- Gram-Negative Bacteria: Conversely, if the bacterial cells display a pink or red hue under the microscope, they are categorized as Gram-negative. This coloration signifies that these bacteria have a thin peptidoglycan layer and an outer lipid membrane. During the decolorization step, they lose the initial purple stain and take up the red counterstain, safranin. Gram-negative bacteria are associated with a different set of infections and often require a different therapeutic approach due to their unique cell wall structure.
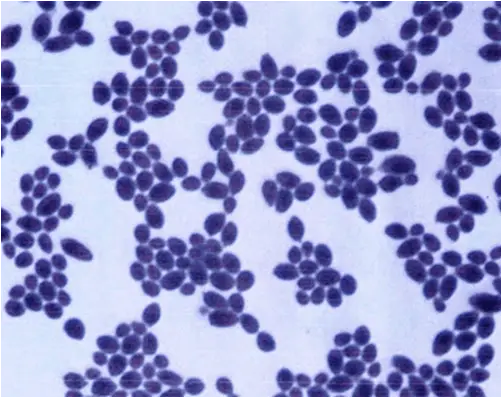
- Fungi and Yeast Cells: Besides bacteria, the Gram stain can also be used to observe fungi, including yeast cells. Fungi, when subjected to the Gram stain procedure, also exhibit a Gram-positive reaction. This means that fungal and yeast cells will appear purple or violet under the microscope, similar to Gram-positive bacteria. The image provided would show yeast cells with this characteristic coloration. However, the morphology and size of yeast cells typically differ from bacterial cells, aiding in their differentiation.