Table of Contents
What is Endocrine System?
- The endocrine system plays a vital role in maintaining balance and regulating various processes within the human body. It consists of a complex network of glands that release hormones directly into the bloodstream, enabling communication and coordination between different organs and tissues. These hormones act as chemical messengers, influencing the function of specific target organs located at a distance from the glands that produce them.
- The hypothalamus, situated in the brain, serves as the central control center for the entire endocrine system in vertebrates, including humans. It receives signals from the nervous system and orchestrates the release of hormones from the major endocrine glands.
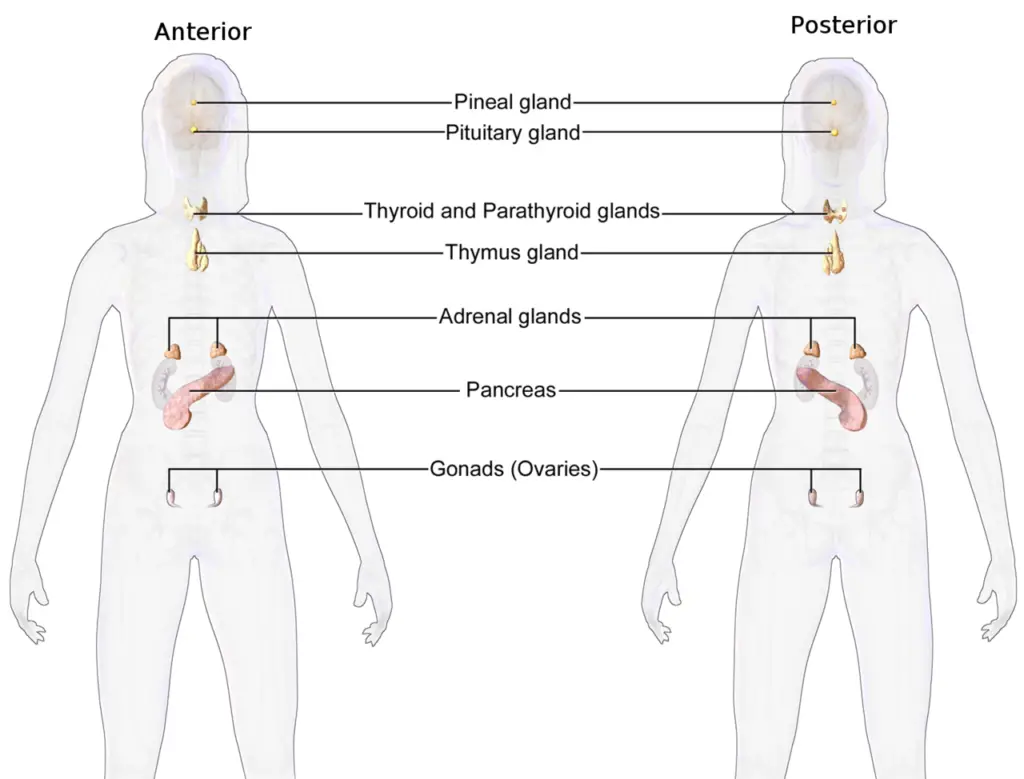
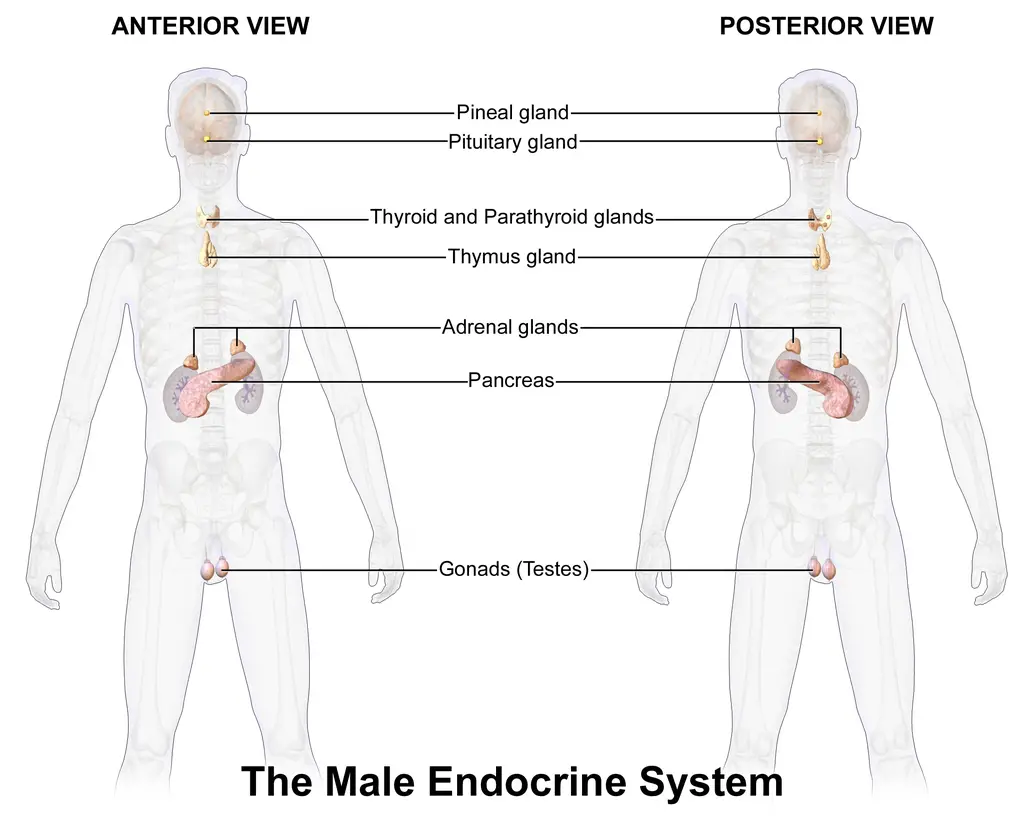
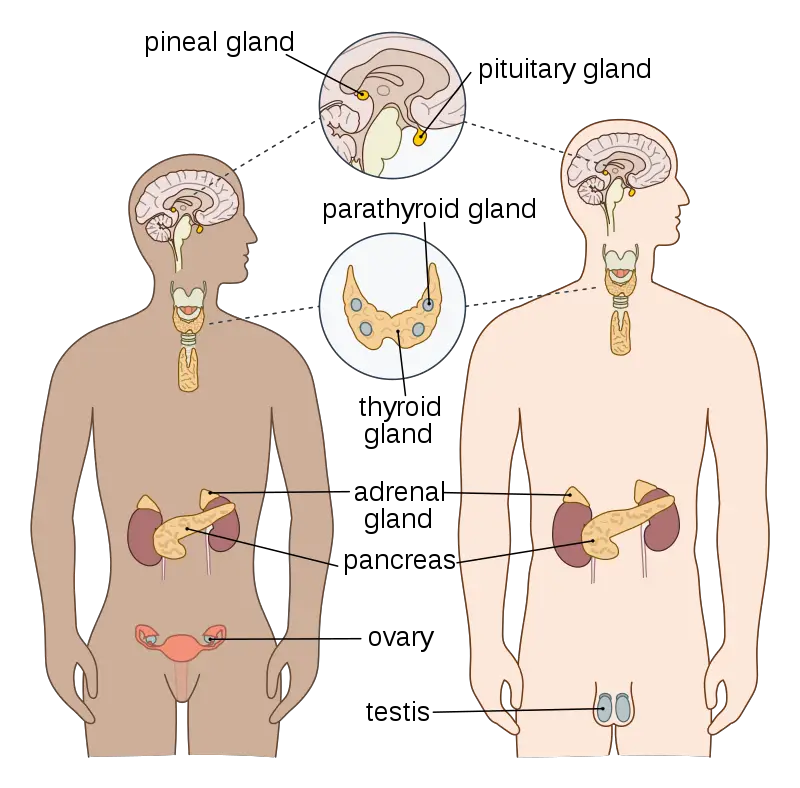
- These glands include the thyroid gland, which produces hormones essential for metabolism regulation, the parathyroid gland, responsible for maintaining calcium levels, the pituitary gland, often referred to as the “master gland” as it controls the activity of other endocrine glands, the pineal gland, which influences sleep patterns and circadian rhythms, the testes in males, which produce testosterone, and the ovaries in females, responsible for producing estrogen and progesterone.
- Additionally, the adrenal glands, pancreas, and thymus also function as endocrine glands, along with their other physiological roles. Furthermore, certain organs like the kidneys have secondary endocrine functions and secrete hormones such as erythropoietin.
- The study of the endocrine system and its disorders is known as endocrinology, a branch of internal medicine that focuses on understanding hormone production, secretion, and their effects on the body. Endocrinologists specialize in diagnosing and treating hormonal imbalances and dysfunctions.
- One notable characteristic of the endocrine system is the presence of hormone signaling axes. These axes involve a sequential signaling pathway between multiple glands. For instance, the hypothalamic-pituitary-adrenal axis regulates the body’s response to stress and is involved in maintaining a stable internal environment. Each gland within these axes releases specific hormones that communicate with one another to maintain homeostasis.
- While the major endocrine glands are crucial components of the system, other organs that are not primarily endocrine glands also possess secondary endocrine functions. The bones, kidneys, liver, heart, and gonads contribute to the endocrine system by releasing hormones. For example, the kidneys secrete erythropoietin, which stimulates the production of red blood cells.
- The endocrine system differs from exocrine glands, which secrete substances externally or through ducts. Endocrine glands lack ducts and release hormones directly into the bloodstream. They are highly vascularized and contain specialized intracellular compartments like vacuoles or granules for hormone storage. In contrast, exocrine glands, such as salivary and sweat glands, have ducts or hollow lumens through which their secretions are transported. The study of exocrine glands and their functions falls under the field of exocrinology.
- Understanding the intricacies of the endocrine system is essential as it governs various physiological processes, including growth and development, metabolism, reproduction, mood regulation, and many others.
- Hormonal imbalances can lead to a wide range of disorders and conditions, such as diabetes, thyroid dysfunction, adrenal insufficiency, and reproductive disorders. Through ongoing research and medical advancements, endocrinologists continue to explore and develop treatments to address these disorders and optimize the functioning of the endocrine system, thereby promoting overall health and well-being.
Definition of Endocrine System
The endocrine system is a network of glands that release hormones into the bloodstream to regulate various functions and maintain balance within the body.
Structure of Endocrine System
- The endocrine system in the human body is a complex network of glands and organs that work together to regulate various physiological processes through the production and secretion of hormones. These hormones are chemical messengers that are released into the bloodstream and act on target cells or organs to elicit specific responses. The structure of the endocrine system is intricately designed to ensure proper communication and coordination within the body.
- The major endocrine systems in the human body operate through feedback loops, with several important feedback systems mediated by the hypothalamus and pituitary gland. One example is the TRH-TSH-T3/T4 feedback loop, which involves the hypothalamus secreting thyrotropin-releasing hormone (TRH), which stimulates the pituitary gland to release thyroid-stimulating hormone (TSH), and ultimately leads to the production and release of the thyroid hormones T3 and T4. Similarly, the GnRH-LH/FSH feedback loop regulates the production of sex hormones, while the CRH-ACTH feedback loop controls the secretion of cortisol. Other feedback systems include renin-angiotensin-aldosterone and the interplay between leptin and ghrelin.
- The endocrine glands are responsible for secreting hormones directly into the interstitial spaces, where they are absorbed into the bloodstream rather than through a duct. The main glands of the endocrine system include the pineal gland, pituitary gland, pancreas, ovaries, testes, thyroid gland, parathyroid gland, hypothalamus, and adrenal glands. The hypothalamus and pituitary gland are unique in that they function as both neural and endocrine organs, playing a crucial role in cell signaling within the nervous system.
- The hypothalamus serves as a key regulator of the autonomic nervous system and has three sets of endocrine outputs: the magnocellular system, the parvocellular system, and autonomic intervention. The magnocellular system is involved in the expression of oxytocin or vasopressin, while the parvocellular system controls the secretion of hormones from the anterior pituitary gland.
- The anterior pituitary gland is responsible for producing and secreting tropic hormones, such as thyroid-stimulating hormone (TSH), adrenocorticotropic hormone (ACTH), growth hormone (GH), luteinizing hormone (LH), and follicle-stimulating hormone (FSH). These tropic hormones act on other endocrine glands to regulate their hormone production and maintain balance within the body.
- The endocrine system comprises various types of cells that make up the tissues and organs involved. For instance, the hypothalamus and anterior pituitary gland are composed of specialized cells that facilitate their functions in hormone regulation. The pineal gland, posterior pituitary gland, thyroid gland, parathyroid gland, thymus gland, adrenal glands, pancreas, ovaries, and testes all consist of specific cells that secrete hormones or perform other essential functions within the endocrine system.
- The posterior pituitary gland, although not responsible for hormone production, stores and releases hormones such as antidiuretic hormone (ADH) and oxytocin, which play important roles in water balance and various reproductive functions.
- The thyroid gland contains follicular cells that produce and secrete T3 and T4 hormones, which regulate metabolic activity and cell growth throughout the body. The parathyroid glands, composed of epithelial cells, secrete parathyroid hormone (PTH) that controls calcium and phosphate levels in the blood and stimulates the conversion of Vitamin D to its active form.
- The adrenal glands consist of two parts: the adrenal cortex and the adrenal medulla. The adrenal cortex secretes hormones such as cortisol, aldosterone, and sex hormones, while the adrenal medulla produces and releases adrenaline and noradrenaline, which are involved in the body’s response to stress.
- The pancreas contains specialized cells called islets of Langerhans, which secrete hormones involved in maintaining blood sugar levels. Alpha cells produce and release glucagon to raise blood sugar levels, while beta cells secrete insulin to lower blood sugar levels. Delta cells and F cells in the pancreas also play roles in hormone regulation.
- The ovaries in females have granulosa cells that produce estrogen and progesterone, which are essential for reproductive processes and the menstrual cycle. In males, the testes contain Leydig cells that secrete testosterone, the primary male sex hormone responsible for various masculine characteristics.
- In conclusion, the structure of the endocrine system encompasses a network of glands and organs that work together to regulate numerous physiological processes through the production and secretion of hormones. Each gland and organ consists of specialized cells that contribute to the overall functioning of the endocrine system, ensuring proper communication and coordination within the body.
Development of Endocrine Gland
- The development of endocrine glands involves the differentiation of cells from various germ layers during embryonic development. The origin of these glands can be traced back to different layers, including the mesoderm, ectoderm, and endoderm, which give rise to glands producing different types of hormones.
- Endocrine glands derived from the mesoderm, such as the adrenal cortex and gonads, primarily produce steroid hormones. These glands undergo a process of differentiation, where specific cells within the mesoderm transform into glandular cells. These glandular cells then develop the ability to synthesize and secrete steroid hormones, which play crucial roles in various physiological processes.
- On the other hand, endocrine glands originating from the ectoderm or endoderm secrete hormones such as amine hormones or protein hormones. During the development of these glands, certain cells in the surface epithelium undergo modifications, acquiring glandular characteristics. Over time, these modified cells mature and detach from the surface epithelium, forming separate organs known as endocrine glands. These glands have a well-vascularized structure, allowing for efficient hormone secretion and distribution throughout the body.
- For example, the thyroid gland develops from the pharyngeal wall during embryonic development. It begins as a part of the surface epithelium but eventually undergoes maturation and becomes a distinct, ductless gland. In contrast, exocrine glands maintain their connection with the surface epithelium through a duct system, enabling the secretion of their products onto the body’s surfaces or into cavities.
- The development of endocrine glands is a complex and intricate process that involves the transformation of cells from their site of origin into specialized glandular structures. This development is crucial for the proper functioning of the endocrine system, as it ensures the production and secretion of hormones necessary for maintaining physiological balance and regulating various bodily processes.
Classification of Endocrine Glands
The classification of endocrine glands can be based on different criteria, including their location, number, and mode of secretion. By categorizing endocrine glands, we can gain a better understanding of their diversity and functions within the vertebrate body.
On the Basis of Location:
- Cranial endocrine glands: These glands are situated in the head region. Examples include the pituitary gland, pineal gland, and hypothalamus. The pituitary gland plays a crucial role in hormone regulation and is often referred to as the “master gland” due to its control over other endocrine glands. The pineal gland produces melatonin, which is involved in regulating sleep-wake cycles. The hypothalamus acts as a bridge between the nervous and endocrine systems, regulating hormone release from the pituitary gland.
- Pharyngeal endocrine glands: These glands are located in the pharyngeal or neck region. The thyroid gland, responsible for producing thyroid hormones that regulate metabolism, is a prominent example. The parathyroid glands, embedded within the thyroid gland, play a vital role in calcium homeostasis.
- Abdominal endocrine glands: These glands are found in the abdominal region. Examples include the pancreas, adrenal glands, testes, and ovaries. The pancreas produces insulin and glucagon, hormones involved in blood sugar regulation. The adrenal glands secrete hormones such as cortisol and adrenaline, which are involved in stress response. The testes produce testosterone in males, while the ovaries produce estrogen and progesterone in females, regulating reproductive processes.
On the Basis of Number:
- Unilateral endocrine glands: These glands exist as a single structure. Examples include the pituitary gland, pineal gland, and pancreas. The pituitary gland, located at the base of the brain, consists of two lobes, the anterior and posterior pituitary, each with distinct hormone-secreting cells. The pineal gland is a single small structure located deep within the brain. The pancreas, although having both exocrine and endocrine functions, is considered a unilateral endocrine gland due to its hormone-secreting islets of Langerhans.
- Bilateral endocrine glands: These glands exist as paired structures. Examples include the thyroid gland, adrenal glands, and parathyroid glands. The thyroid gland, located in the neck on either side of the trachea, consists of two lobes connected by an isthmus. The adrenal glands, situated on top of each kidney, consist of an outer adrenal cortex and an inner adrenal medulla. The parathyroid glands, usually four in number, are small structures embedded within the thyroid gland.
On the Basis of Secretion
- Telecrine glands: These glands release hormones directly into the bloodstream, which then travel to target cells or organs. Examples include the thyroid gland, adrenal gland, and pituitary gland. Hormones produced by these glands have far-reaching effects throughout the body.
- Paracrine glands: These glands secrete hormones that act locally on nearby cells or tissues. Instead of entering the bloodstream, the hormones diffuse through the interstitial fluid to reach adjacent target cells. An example is the islets of Langerhans in the pancreas, where somatostatin secreted by delta cells acts on nearby alpha and beta cells, regulating insulin and glucagon secretion.
By classifying endocrine glands based on their location, number, and secretion patterns, we can appreciate the diversity and specialized functions of these essential components of the endocrine system. Each category of endocrine gland contributes to maintaining homeostasis and regulating various physiological processes within the vertebrate body.
Endocrine glands
- Pituitary Gland
- Thyroid Gland
- Parathyroid Glands
- Adrenal Gland (Suprarenal)
- Pancreas
- Testis
- Ovary
- Placenta
- Thymus
- Pineal Body
- Gastrointestinal Mucosa
- Kidney
- Liver
- Heart
1. Pituitary Gland
The pituitary gland, also known as the hypophysis or master gland, is a small oval structure located on the ventral side of the diencephalon in the brain. It measures about 10 mm in diameter and weighs approximately 0.5 grams. The gland is positioned below the hypothalamus, connected by a stalk called the infundibulum.
The pituitary gland is divided into two main parts: the adenohypophysis (anterior and intermediate lobes) and the neurohypophysis (posterior lobe). The adenohypophysis consists of the anterior lobe (pars distalis and pars tuberalis) and the intermediate lobe (pars intermedia). On the other hand, the neurohypophysis, also known as the posterior lobe, is composed of the pars nervosa and infundibulum.
Often referred to as the “Band master of endocrine orchestra,” the pituitary gland plays a crucial role in regulating the activity of other endocrine glands in the body. It secretes a variety of hormones with different functions. Some of the hormones released by the pituitary gland include:
- Growth hormone (GH): This hormone stimulates the growth and development of tissues and bones, particularly during childhood and adolescence.
- Thyroid-stimulating hormone (TSH): TSH regulates the function of the thyroid gland, stimulating the production and release of thyroid hormones that control metabolism.
- Luteinizing hormone (LH) and follicle-stimulating hormone (FSH): LH and FSH are involved in the regulation of reproductive processes. LH stimulates the production of sex hormones (e.g., testosterone in males, estrogen in females) and ovulation in females, while FSH plays a role in the maturation of eggs in females and the production of sperm in males.
These are just a few examples of the hormones secreted by the pituitary gland. Each hormone has specific functions and targets specific tissues or organs in the body, contributing to the regulation of various physiological processes.
As the master gland, the pituitary gland controls and coordinates the activities of other endocrine glands. It receives signals from the hypothalamus, which acts as a bridge between the nervous and endocrine systems, and releases appropriate hormones to regulate the functioning of target glands. This intricate hormonal control system is essential for maintaining overall homeostasis and ensuring the proper functioning of the body.
Anterior Lobe
The anterior lobe of the pituitary gland, known as the pars distalis, plays a crucial role in the production and secretion of several hormones that regulate various physiological processes. The pars tuberalis, on the other hand, is a supporting structure and does not secrete any hormones.
- Growth Hormone (GH) or Somatotrophic Hormone (STH): The growth hormone is responsible for promoting the growth and development of bones, cartilages, muscles, visceral organs, and the entire body. It stimulates protein synthesis, facilitates intestinal calcium absorption, and promotes glycogenolysis. Hyposecretion of GH during childhood leads to dwarfism, while hypersecretion during childhood results in gigantism. In adulthood, excessive GH secretion causes acromegaly.
- Adrenocorticotropic Hormone (ACTH): ACTH is a tropic hormone that regulates the activity of the adrenal cortex. It stimulates the production of glucocorticoids, which are essential for various metabolic processes. ACTH secretion increases during emotional and physical stress.
- Thyroid Stimulating Hormone (TSH) or Thyrotrophic Hormone (TTH): TSH controls the growth and activity of the thyroid gland. It stimulates the synthesis and release of thyroxine (T4) from the thyroid gland. TSH plays a vital role in maintaining proper thyroid function and regulating metabolism.
- Follicle-Stimulating Hormone (FSH): FSH is a gonadotropic hormone that has different functions in males and females. In females, it stimulates the development and maturation of ovarian follicles. In males, FSH promotes the development of seminiferous tubules in the testes and supports spermatogenesis. FSH is also known as the Gametokinetic factor due to its role in the development of male and female gametes.
- Luteinizing Hormone (LH) or Interstitial Cell Stimulating Hormone (ICSH): LH is another gonadotropic hormone with distinct functions in males and females. In females, it triggers the final maturation of the ovarian follicle, stimulates ovulation, and promotes the formation of the corpus luteum. In males, LH stimulates the interstitial cells of the testes, leading to the production and release of male sex hormones (androgens).
- Lactogenic Hormone or Prolactin (LTH): Also known as prolactin, this hormone plays a crucial role in females during pregnancy and after childbirth. It stimulates the growth and development of mammary glands, preparing them for milk production. After childbirth, prolactin initiates the secretion of milk for breastfeeding.
These hormones secreted by the anterior lobe of the pituitary gland are essential for growth, metabolism, reproduction, and lactation, among other physiological processes in the body.
Intermediate Lobe
The intermediate lobe, also known as the pars intermedia, is a section of the pituitary gland that has a specialized function related to the production of a specific hormone called Melanocyte Stimulating Hormone (MSH) or Intermedin.
- Melanocyte Stimulating Hormone (MSH) or Intermedin: The sole hormone produced by the intermediate lobe is MSH, which plays a role in the synthesis and regulation of melanin pigment in melanocytes or melanophore cells. Melanin is responsible for determining the coloration of the skin, hair, and eyes.
In various species such as fishes, amphibians, and reptiles, MSH influences the dramatic phenomenon of color-change. It triggers the dispersion of melanin pigments within melanophore cells, leading to changes in skin color and patterns. This adaptive response allows these animals to camouflage, communicate, or regulate body temperature.
In higher vertebrates, including humans, the role of MSH in normal physiological processes is not as significant. However, certain conditions such as pregnancy can lead to increased production of MSH, resulting in the darkening of the skin. This change in skin pigmentation is commonly observed in some pregnant women, often referred to as “mask of pregnancy” or “chloasma.”
Overall, while the intermediate lobe of the pituitary gland has a limited hormonal function, MSH plays a role in regulating melanin production and its effects on skin coloration and pigmentation.
Neurohypophysis
The neurohypophysis, also known as the posterior lobe of the pituitary gland, is responsible for the storage and release of two peptide hormones. These hormones are synthesized in the hypothalamus and transported to the posterior lobe via nerve fibers, where they are stored until needed. Let’s explore these hormones in detail:
- Oxytocin (Pitocin): Oxytocin is a hormone that plays a crucial role in reproductive processes and bonding. Its primary functions include:
- Uterine Contraction: Oxytocin stimulates the contraction of the smooth muscles in the uterus during childbirth. This helps facilitate labor and delivery.
- Milk Ejection: In lactating mothers, oxytocin contracts the smooth muscles surrounding the mammary glands, leading to the flow of milk during breastfeeding.
- Smooth Muscle Contraction: Oxytocin also affects other smooth muscles in the body, such as those in the gallbladder, urinary bladder, and intestine, promoting their relaxation.
- Vasopressin (Antidiuretic Hormone – ADH or Pitressin): Vasopressin, also known as antidiuretic hormone (ADH), plays a vital role in regulating water balance in the body. Its key functions include:
- Water Reabsorption: ADH acts on the distal convoluted tubules and collecting tubules of the kidney, increasing the reabsorption of water. This helps in reducing urine volume and preventing excessive water loss. Insufficient production or release of ADH can lead to a condition called diabetes insipidus, characterized by increased urine volume.
- Smooth Muscle Contraction: ADH also affects the contraction of smooth muscles in various organs, including the intestines, gallbladder, urinary bladder, and blood vessels. Contraction of blood vessels can lead to increased arterial blood pressure.
- Alcohol’s Effect: Intake of alcohol inhibits the secretion of ADH, resulting in increased urine production and potential dehydration.
In summary, the neurohypophysis releases oxytocin and vasopressin. Oxytocin plays a role in uterine contraction, milk ejection, and smooth muscle relaxation, while vasopressin regulates water reabsorption, smooth muscle contraction, and blood pressure. These hormones are essential for various physiological processes and help maintain proper bodily functions.
Hypophysectomy
Hypophysectomy refers to the surgical removal of the pituitary gland, also known as the hypophysis. This procedure can lead to various disorders and hormonal imbalances due to the absence of pituitary gland function. Let’s explore the consequences of hypophysectomy:
- Impaired Gonadal Function: Without the pituitary gland, the secretion of gonadotropins, such as luteinizing hormone (LH) and follicle-stimulating hormone (FSH), is disrupted. These hormones are responsible for stimulating the development and function of the gonads (testes in males and ovaries in females). As a result, the gonads fail to mature in young individuals and undergo degeneration in adults. This leads to infertility and a loss of reproductive capacity.
- Thyroid Gland Dysfunction: The pituitary gland plays a crucial role in regulating the thyroid gland’s activity through the secretion of thyroid-stimulating hormone (TSH). In the absence of TSH, the thyroid gland’s function is compromised, leading to shrinkage of the gland and a slowdown in metabolic processes. This can result in symptoms such as fatigue, weight gain, and sluggishness.
- Adrenal Cortex Inactivity: Another important hormone regulated by the pituitary gland is adrenocorticotropic hormone (ACTH), which stimulates the production of cortisol in the adrenal cortex. Without ACTH, the adrenal cortex becomes inactive, leading to a deficiency of cortisol. This can result in adrenal insufficiency, characterized by fatigue, weakness, low blood pressure, and potentially life-threatening symptoms.
- Impaired Growth: The pituitary gland also secretes growth hormone (GH), which is essential for normal growth and development. Removal of the pituitary gland eliminates the production of GH, resulting in complete retardation of growth. This can lead to short stature and developmental delays.
- Inhibition of Pregnancy and Lactation: The absence of pituitary gland function disrupts the secretion of hormones involved in pregnancy and lactation. Hormones such as prolactin, which promotes milk production in the breast, may be significantly reduced or absent. As a result, pregnancy and lactation are inhibited, making it difficult or impossible for individuals to conceive or produce breast milk.
Overall, hypophysectomy disrupts the normal hormonal balance and can have significant consequences on reproductive function, thyroid activity, adrenal function, growth, and the ability to conceive and lactate. Hormone replacement therapy and other interventions may be necessary to manage these hormonal deficiencies and maintain normal bodily functions after the removal of the pituitary gland.
Hypothalamus
The hypothalamus is a small, vital region located at the base of the brain, and it plays a crucial role in regulating various bodily functions and maintaining homeostasis. One of its key functions is the secretion of releasing and inhibitory hormones that control the release of certain anterior pituitary hormones. Let’s explore some of these hypothalamic hormones:
- Thyrotropin Releasing Hormone (TRH): TRH stimulates the release of thyroid-stimulating hormone (TSH) from the anterior pituitary gland. TSH, in turn, regulates the activity of the thyroid gland and the production of thyroid hormones, such as thyroxine (T4) and triiodothyronine (T3), which are important for metabolism and energy regulation.
- Corticotropin Releasing Hormone (CRH): CRH stimulates the secretion of adrenocorticotropic hormone (ACTH) from the anterior pituitary. ACTH then stimulates the adrenal glands to release cortisol, a hormone involved in stress response, metabolism, and immune function.
- Growth Hormone-Releasing Hormone (GH-RH): GH-RH stimulates the release of growth hormone (GH) from the anterior pituitary. GH plays a crucial role in promoting growth, particularly during childhood and adolescence. It also influences metabolism, body composition, and tissue repair.
- Growth Hormone Release Inhibiting Hormone (GH-RIH) or Somatostatin: Somatostatin, also known as GH-RIH, inhibits the release of growth hormone from the anterior pituitary. It acts as a negative regulator to maintain the balance of GH secretion.
- Prolactin Releasing Factor (PRF): PRF stimulates the release of prolactin (PRL) from the anterior pituitary. Prolactin plays a key role in lactation and milk production in breastfeeding women.
- Prolactin Inhibiting Factor (PIF): PIF, also known as dopamine, inhibits the release of prolactin from the anterior pituitary. It helps regulate the production of prolactin, preventing excessive levels of the hormone when not needed for lactation.
- Gonadotropin Releasing Hormone (GnRH): GnRH controls the secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary. FSH and LH play vital roles in regulating the reproductive system and the production of sex hormones in both males and females.
- MSH-Releasing Hormone (MRH): MSH-Releasing Hormone stimulates the release of melanocyte-stimulating hormone (MSH). MSH is involved in regulating pigmentation and melanin production in the skin and hair.
- MSH-Release Inhibiting Hormone (MRIH): MRIH, also known as dopamine, inhibits the release of melanocyte-stimulating hormone (MSH). It helps regulate the production of MSH and the pigmentation processes in the body.
The hypothalamus acts as a control center for these releasing and inhibitory hormones, and their secretion is finely regulated to maintain hormonal balance and ensure proper functioning of the endocrine system. The hypothalamus-pituitary axis is a crucial pathway for hormonal regulation and plays a vital role in maintaining overall physiological stability.
Function Of Hormones Secreted By Pituitary Gland
The pituitary gland, comprised of the anterior and posterior parts, plays a vital role in regulating various physiological processes through the secretion of hormones. The hormones released by the pituitary gland can be categorized into two main groups: those secreted by the anterior pituitary and those stored and released by the posterior pituitary.
Anterior Pituitary Hormones:
- Human Growth Hormone (HGH): This hormone is responsible for the growth and repair of cells throughout the body. It promotes protein synthesis, stimulates tissue growth, and influences bone and muscle development.
- Thyroid Stimulating Hormone (TSH): TSH stimulates the thyroid gland to produce and release thyroxine, which plays a crucial role in regulating metabolism, energy production, and the overall functioning of organs and tissues.
- Adrenocorticotropic Hormone (ACTH): ACTH stimulates the adrenal glands to secrete cortisol, often referred to as the “stress hormone.” Cortisol helps the body respond to stress, regulates blood sugar levels, and plays a role in metabolism and immune system function.
- Luteinising Hormone (LH) and Follicle-Stimulating Hormone (FSH): LH and FSH, collectively known as gonadotropins, are involved in regulating the reproductive system. In females, LH triggers ovulation and stimulates the production of estrogen and progesterone. In males, LH stimulates the production of testosterone. FSH plays a role in the development of eggs in females and the production of sperm in males.
- Prolactin (PRL): Prolactin is responsible for stimulating milk production in the mammary glands. Its levels increase during pregnancy and after childbirth to support lactation.
- Melanocyte-Stimulating Hormone (MSH): MSH is involved in the regulation of melanin production by the skin and hair. It plays a role in determining skin pigmentation and hair color.
Posterior Pituitary Hormones:
- Antidiuretic Hormone (ADH): Also known as vasopressin, ADH regulates the water balance in the body by controlling the reabsorption of water by the kidneys. It helps maintain proper hydration levels and prevents excessive water loss through urine.
- Oxytocin: Oxytocin plays a crucial role in various reproductive processes. In females, it stimulates uterine contractions during childbirth and promotes milk ejection during breastfeeding. It also plays a role in bonding, social interaction, and emotional attachment.
These hormones released by the pituitary gland are essential for maintaining homeostasis, regulating growth and development, controlling reproductive functions, and ensuring the proper functioning of various organs and systems in the body.
2. Thyroid Gland
The thyroid gland is a vital endocrine gland found in vertebrates, including humans. In humans, it is located in the lower part of the neck, ventral to the trachea, just behind the larynx. The gland is bilobed, with two lobes joined together by a thin band of tissue called the isthmus. It typically weighs around 25 to 40 grams and consists of numerous glandular follicles or vesicles that are filled with a proteinaceous secretion called thyroglobulin.
The thyroid gland is responsible for producing and secreting two important hormones:
- Thyroxine (T4): Thyroxine, also known as tetraiodothyronine, is a crucial hormone produced by the thyroid gland. It plays a vital role in regulating metabolism and energy balance throughout the body. Thyroxine influences the metabolism of carbohydrates, proteins, and fats, helps maintain body temperature, supports growth and development, and affects various organ systems. It is synthesized by combining the amino acid tyrosine with iodine, and it circulates in the bloodstream, affecting cells throughout the body.
- Calcitonin: Calcitonin is another hormone secreted by the thyroid gland, but it is produced by specialized cells called C cells or parafollicular cells. Calcitonin plays a role in regulating calcium levels in the body. It helps to lower blood calcium levels by inhibiting the release of calcium from bones and promoting its excretion by the kidneys. Calcitonin works in opposition to another hormone called parathyroid hormone (PTH), which increases blood calcium levels.
Both thyroxine and calcitonin are important for maintaining the overall homeostasis of the body. They are regulated by feedback mechanisms involving the hypothalamus and the pituitary gland. The hypothalamus releases thyrotropin-releasing hormone (TRH), which stimulates the pituitary gland to release thyroid-stimulating hormone (TSH). TSH, in turn, stimulates the thyroid gland to produce and release thyroxine. The production and secretion of calcitonin are regulated independently.
Imbalances in thyroid hormone production can lead to various disorders. Hypothyroidism occurs when the thyroid gland produces insufficient amounts of thyroid hormones, resulting in symptoms such as fatigue, weight gain, and sluggishness. Hyperthyroidism, on the other hand, is characterized by excessive production of thyroid hormones, leading to symptoms such as weight loss, increased heart rate, and irritability.
The thyroid gland is a crucial component of the endocrine system, and its hormones play a vital role in maintaining overall health and metabolic balance in the body.
a. Thyroxine
Thyroxine, also known as tetraiodothyronine, is a hormone produced by the thyroid gland. It is an iodine-containing hormone, with 80% of it being in the form of tetraiodothyronine (T4) and 20% in the form of tri-iodothyronine (T3). T3 is more biologically active, being 3 to 4 times more potent than T4. The production of these hormones is regulated by thyroid-stimulating hormone (TSH) released by the pituitary gland.
Thyroxine plays several important roles in the body:
- Increased Basal Metabolic Rate (BMR): Thyroxine stimulates the metabolism of cells, leading to increased oxygen consumption and energy production. This results in an elevated basal metabolic rate, influencing processes such as body temperature regulation and energy utilization.
- Normal Growth and Development: Thyroxine is crucial for the normal growth and development of various tissues and organs, especially during infancy and childhood. It supports the growth and maturation of bones, muscles, and the nervous system.
- Hair and Skin Health: Adequate levels of thyroxine contribute to the maintenance of healthy hair and skin. Thyroxine deficiency may lead to dryness, hair loss, and changes in skin texture.
- Increased Glucose Absorption: Thyroxine enhances the absorption of glucose from the intestine, supporting the body’s energy needs.
- Nervous System Function: Thyroxine influences the excitability of nerve fibers, helping to regulate the transmission of nerve impulses.
- Metamorphosis: In certain organisms like amphibians, thyroxine plays a critical role in the metamorphosis of tadpole larvae into adult frogs. It triggers developmental changes, such as limb formation and the reabsorption of the tail.
When there is excessive secretion of thyroxine, a condition known as hyperthyroidism occurs. This can result in symptoms such as exophthalmic goiter (bulging of the eyes), increased metabolic rate, rapid heartbeat, high blood pressure, restlessness, nervousness, and difficulty sleeping.
On the other hand, insufficient secretion of thyroxine leads to hypothyroidism. In adults, this condition is known as myxedema or Gull’s disease. Symptoms include facial and hand puffiness, dry and coarse skin, low body temperature, and a slow pulse rate. In children, inadequate thyroxine production can cause a condition called cretinism, characterized by stunted growth, intellectual impairment, and delayed physical, mental, and sexual development. Inadequate dietary intake of iodine can also result in thyroid gland enlargement, known as simple goiter.
Thyroxine plays a crucial role in maintaining the body’s overall metabolic balance, growth, and development. Imbalances in its production can lead to significant physiological and clinical effects.
b. Thyrocalcitonin (TCT)
- Thyrocalcitonin (TCT), also known as calcitonin, is a polypeptide hormone secreted by the thyroid gland. Its release is stimulated by high levels of ionized calcium in the blood. TCT primarily acts as a hypocalcemic and hypophosphatemic hormone, meaning it reduces the levels of calcium and phosphorus in the blood.
- The main target of TCT is the bones. It exerts its effects by inhibiting the removal of calcium from the bones, a process known as bone resorption. In young animals, particularly during periods of growth and bone formation, TCT plays a crucial role. It promotes the deposition of calcium onto the bones while simultaneously inhibiting its release into the bloodstream. This mechanism allows for the proper growth and development of bones.
- By inhibiting bone resorption, TCT helps maintain the balance of calcium in the body. It prevents excessive levels of calcium from entering the bloodstream, which could lead to hypercalcemia. Instead, TCT promotes the excretion of excess calcium through urine, aiding in its elimination from the body.
- The regulation of calcium levels in the blood is important for various physiological processes. Calcium is essential for the functioning of muscles, nerve transmission, blood clotting, and maintaining healthy bone density. TCT acts as a counter-regulatory hormone to parathyroid hormone (PTH). While PTH increases blood calcium levels by promoting its release from bones, TCT works in the opposite direction, preventing excessive calcium release and aiding in its retention within the bones.
- In certain medical conditions, such as osteoporosis, where excessive bone resorption occurs, synthetic calcitonin may be used as a therapeutic intervention to help reduce bone loss. However, the clinical use of calcitonin has become less common in recent years.
- Overall, TCT plays a crucial role in regulating calcium and phosphorus levels in the body, particularly by inhibiting bone resorption and aiding in bone growth and development. Its actions help maintain the balance of these essential minerals and contribute to overall skeletal health.
3. Parathyroid Glands
- The parathyroid glands are four small endocrine glands located on the posterior surface of the thyroid gland. There are usually two parathyroid glands situated on each lobe of the thyroid gland. These glands secrete a protein hormone known as parathormone (PTH), which plays a crucial role in maintaining calcium levels in the blood, along with another hormone called calcitonin.
- The primary function of parathormone is to regulate the level of calcium in the bloodstream. It acts to increase blood calcium levels by various mechanisms. PTH promotes the release of calcium from bones, where it is stored, into the bloodstream. This process is known as bone resorption. PTH also enhances the absorption of calcium from the intestines, thereby increasing the amount of calcium entering the bloodstream through the digestive system. Additionally, PTH decreases the excretion of calcium through urine, further aiding in maintaining adequate levels of calcium in the blood.
- When there is a deficiency of parathormone, it results in lower blood calcium levels, a condition known as hypocalcemia. Hypocalcemia can lead to increased excitability of nerves and muscles, causing symptoms such as muscle cramps, twitching, and spasms. Severe hypocalcemia can even lead to a condition called parathyroid tetany, characterized by muscle stiffness and spasms.
- On the other hand, excessive secretion of parathormone leads to a condition called hyperparathyroidism. In hyperparathyroidism, there is an excess of PTH, resulting in elevated blood calcium levels. The high levels of calcium can have detrimental effects on various organs and tissues. It can lead to the demineralization and weakening of bones, a condition known as osteoporosis. Increased calcium levels in the blood can also cause the formation of kidney stones and affect the functioning of other organs.
- In contrast to parathormone, the parathyroid glands also secrete calcitonin, which has the opposite effect on calcium regulation. Calcitonin works to lower blood calcium levels by promoting the deposition of calcium into bones, inhibiting bone resorption. Its actions counterbalance the effects of parathormone and contribute to the overall regulation of calcium homeostasis.
- In summary, the parathyroid glands play a crucial role in maintaining calcium balance in the body. Parathormone increases blood calcium levels by promoting its release from bones, increasing calcium absorption from the intestines, and reducing calcium excretion. Calcitonin, secreted by the parathyroid glands, works to lower blood calcium levels by promoting calcium deposition in bones. The balance between parathormone and calcitonin is essential for maintaining optimal calcium levels, which are vital for various physiological processes in the body.
4. Adrenal Gland (Suprarenal)
The adrenal glands, also known as suprarenal glands, are a pair of endocrine glands located on top of each kidney. Each adrenal gland consists of two distinct regions: the outer cortex and the inner medulla, which have different origins, structures, and functions.
Adrenal Cortex
The adrenal cortex can be further divided into three layers: the zona glomerulosa, zona fasciculata, and zona reticularis. Each layer secretes different hormones and plays a specific role in the body.
- Mineralocorticoids: The zona glomerulosa secretes mineralocorticoid hormones, with aldosterone being the most prominent one. Mineralocorticoids regulate salt and water balance in the body. Aldosterone acts on the renal tubules of the kidneys, promoting the reabsorption of sodium and water while excreting potassium. This helps maintain electrolyte balance, blood volume, and blood pressure. Disorders of mineralocorticoid secretion can lead to conditions such as Addison’s disease (hypo-secretion) or hypertension (hyper-secretion).
- Glucocorticoids: The zona fasciculata secretes glucocorticoids, including cortisol (hydrocortisone). Glucocorticoids play a crucial role in carbohydrate, protein, and lipid metabolism. They are involved in regulating blood sugar levels, suppressing inflammation, and modulating the immune response. Cortisol secretion is stimulated by adrenocorticotropic hormone (ACTH) from the anterior lobe of the pituitary gland. Synthetic glucocorticoids, such as cortisone and prednisone, are widely used in medical treatments for their anti-inflammatory and immunosuppressive properties. Excessive glucocorticoid secretion can result in Cushing’s syndrome, characterized by weight gain, muscle weakness, and increased blood sugar levels.
- Sex Corticoids: The zona reticularis secretes small amounts of sex corticoids, including androgens (male sex hormones) and estrogens (female sex hormones). These hormones play a role in the development of secondary sexual characteristics. Excess secretion of androgens in females may lead to masculinization, while hypersecretion in children can cause premature puberty.
Adrenal Medulla
The adrenal medulla is an integral part of the sympathetic nervous system. It secretes two hormones: epinephrine (adrenaline) and norepinephrine (noradrenaline). These hormones belong to a group called catecholamines and are derived from the amino acid tyrosine.
Epinephrine and norepinephrine are involved in the body’s response to stress and emergency situations. When stimulated by the sympathetic nervous system, the adrenal medulla releases these hormones into the bloodstream. They increase heart rate and blood pressure, promote vasodilation in skeletal muscles, cardiac muscles, and the brain, and enhance the supply of oxygen and glucose-rich blood to these vital areas. This physiological response prepares the body for “fight or flight” during situations such as fear, excitement, or danger.
In summary, the adrenal glands consist of the outer cortex and inner medulla. The cortex secretes hormones that regulate salt and water balance (mineralocorticoids), carbohydrate metabolism and immune response (glucocorticoids), and secondary sexual characteristics (sex corticoids). The medulla releases epinephrine and norepinephrine, which are involved in the body’s response to stress and emergency situations. The adrenal glands play a vital role in maintaining homeostasis and adapting to various physiological challenges.
5. Pancreas
The pancreas is a gland with both exocrine and endocrine functions. The exocrine part consists of pancreatic acini, which secrete digestive enzymes, while the endocrine portion is composed of clusters of cells called the Islets of Langerhans. The Islets of Langerhans contain different types of cells, including alpha cells that produce glucagon hormone and beta cells that produce insulin hormone.
Glucagon is a peptide hormone and acts as a hyperglycemic factor, meaning it raises blood glucose levels. It achieves this by stimulating the liver to break down glycogen into glucose, which is then released into the bloodstream. Glucagon is primarily active in the liver since it is secreted into the hepatic portal vein and reaches the liver first. It is broken down in the liver after its action on glycogen, and it does not affect muscle glycogen.
The secretion of glucagon is regulated by the level of blood sugar. When blood sugar levels are within the optimal range, glucagon secretion is reduced. However, in hypoglycemic conditions (low blood sugar), more glucagon is secreted to increase blood glucose levels.
Insulin, the first hormone to be discovered, is a protein hormone consisting of 51 amino acids arranged in two polypeptide chains. Its primary function is to regulate blood glucose levels, earning it the name “hypoglycemic factor” or “anti-diabetic factor.”
The functions of insulin include:
- Promotion of glycogen formation (glycogenesis) from glucose in the liver and muscle.
- Reduction of glucose production from non-carbohydrate sources like proteins and fats.
- Increased permeability of cell membranes to facilitate glucose transport into cells.
- Acceleration of glucose phosphorylation into glucose-6-phosphate for entry into the respiratory cycle.
- Prevention of fat breakdown and the formation of toxic ketone bodies.
- Stimulation of protein synthesis and overall growth of the organism.
Insufficient insulin production or impaired insulin function leads to a condition called diabetes mellitus. In this disease, blood glucose levels rise above normal (80 to 120 mg/100 ml). When it exceeds 180 mg, glucose appears in the urine (glycosuria). Patients with diabetes experience frequent urination, dehydration, weight loss due to protein and fat breakdown, weakness, and fatigue. Abnormal fat metabolism can lead to the overproduction of ketone bodies, resulting in diabetic coma and potentially death.
Insulin and glucagon have opposing actions, and a balanced secretion of both hormones is necessary to maintain the body’s glucose homeostasis. Recent discoveries have identified a third type of endocrine cells in the Islets of Langerhans called delta cells (δ cells). These cells secrete somatostatin, a small peptide consisting of 14 amino acids. Somatostatin has a short lifespan and is rapidly destroyed after secretion.
Some of the inhibitory functions of somatostatin include:
- Inhibition of insulin and glucagon secretion.
- Decrease in the motility of the stomach, duodenum, and gall bladder.
- Reduction of secretion and absorption in the gastrointestinal tract.
Overall, the pancreas plays a crucial role in regulating blood glucose levels through the secretion of insulin, glucagon, and somatostatin. Proper functioning of these hormones is essential for maintaining metabolic balance and preventing conditions like diabetes mellitus.
6. Testis
The testis, also known as the male gonads, is a pair of reproductive organs responsible for producing spermatozoa and secreting male sex hormones, collectively known as androgens. The androgens are steroid hormones produced by the interstitial cells, or Leydig cells, located in the seminiferous tubules of the testis.
The primary function of androgens, particularly testosterone, is to control secondary sex characteristics, regulate the reproductive cycle, and contribute to the growth and development of accessory reproductive organs.
Testosterone, the most important androgen, carries out the following activities:
- Growth and Normal Functioning of Reproductive Organs: Testosterone promotes the growth and normal functioning of various male reproductive organs, including the epididymis, vas deferens, prostate, seminal vesicles, and penis.
- Spermatogenesis and Seminal Fluid Secretion: Testosterone plays a crucial role in promoting spermatogenesis, the process of sperm production. It also helps in the secretion of seminal fluid, which is essential for sperm viability and motility.
- Development of Secondary Sexual Characteristics: Testosterone stimulates the development of secondary sexual characteristics in males. These include a deepening of the voice, the growth of facial, axillary (armpit), and pubic hair, and increased skeletal and muscular growth.
The secretion of testosterone is stimulated by luteinizing hormone (LH) from the anterior lobe of the pituitary gland. The production and release of testosterone are regulated by a feedback inhibition mechanism, ensuring that hormone levels remain within the appropriate range.
Hyposecretion, or underproduction, of testosterone can result in a disorder called eunuchoidism. In this condition, the secondary sex organs, such as the prostate and seminal vesicles, do not develop properly, and the penis remains small and infantile.
Overall, the testis plays a vital role in male reproductive function by producing spermatozoa and secreting androgens, particularly testosterone. These hormones are essential for the development of secondary sexual characteristics, the reproductive cycle, and the proper growth and functioning of male reproductive organs.
7. Ovary
The ovary is one of the primary female reproductive organs, existing as a pair located on each side of the lower abdomen. Structurally, the ovary is composed of germinal epithelium, connective tissues, and groups of interstitial cells.
The ovary plays a crucial role in the female reproductive system by producing hormones and releasing eggs. The developing ovarian follicles within the ovary secrete estrogens, particularly estradiol, which is the most functionally significant form of estrogen. Estrogens are responsible for various physiological effects in females.
The functions of estrogens include:
- Development of Secondary Sex Characteristics: Estrogens promote the development of secondary sexual characteristics during puberty. These include the development of mammary glands, a broad pelvic region, enlargement of the genitalia, growth of pubic and axillary hair, a high-pitched voice, and deposition of fat in specific areas, creating the typical feminine body shape.
- Thickening of Reproductive Structures: Estrogens prepare the uterine mucosa (endometrium), the internal layer of the fallopian tubes, and the vaginal epithelium. They stimulate the thickening of these tissues, making them stratified and glandular, in preparation for potential implantation of a fertilized ovum.
- Menstrual Cycle Regulation: Estrogens, along with other hormones, play a role in regulating the menstrual cycle. Excessive production of estrogens can disrupt the normal menstrual cycle and, in some cases, contribute to the development of certain types of cancer. Insufficient estrogen secretion may lead to menstrual irregularities and underdeveloped genital structures.
After ovulation, the ruptured follicle in the ovary transforms into a structure called the corpus luteum, which produces another hormone known as progesterone. Progesterone is essential for maintaining pregnancy throughout the gestation period. Its functions include:
- Endometrial Preparation and Pregnancy Support: Progesterone prepares the endometrium of the uterus to facilitate the implantation of a fertilized ovum. It also supports the development of the placenta, which supplies nutrients for the growing fetus.
- Inhibition of Uterine Contractions: Progesterone relaxes the uterine muscles, preventing premature contractions and acting as an “antiabortion hormone” to maintain pregnancy.
- Mammary Gland Growth: Progesterone stimulates the full growth and development of mammary glands in preparation for lactation.
Additionally, relaxin is another hormone secreted by the corpus luteum, uterus, and placenta. Its primary role is to facilitate the relaxation of the pubic symphysis in the pelvic girdle toward the end of pregnancy, allowing for easier delivery.
Overall, the ovary is a vital organ involved in the production of hormones, primarily estrogens and progesterone, and the release of eggs for fertilization. These hormones play critical roles in the development of secondary sexual characteristics, regulation of the menstrual cycle, preparation of the reproductive structures for pregnancy, and maintenance of gestation.
8. Placenta
- The placenta is a specialized organ that forms during pregnancy in viviparous mammals. It serves as a vital connection between the developing fetus and the uterine wall of the mother. While its primary function is to provide oxygen, nutrients, and waste elimination for the fetus, the placenta also plays a role in hormone secretion.
- One of the hormones secreted by the placenta is Chorionic Gonadotropin (CG). CG is primarily produced during the early stages of pregnancy and serves multiple purposes. It exerts a protective influence on the developing fetus and helps in maintaining the pregnancy. CG stimulates the ovary to continue producing progesterone, a hormone critical for the maintenance of the endometrium and the prevention of uterine contractions that could lead to miscarriage. Additionally, CG promotes the development of the mammary glands in preparation for lactation.
- The presence of CG in the blood and urine is an important indicator of pregnancy. Detection of CG in urine is commonly used in pregnancy tests to confirm whether an individual is pregnant or not.
- In addition to CG, the placenta also secretes small amounts of estrogens and progesterone. These hormones play crucial roles in regulating various aspects of pregnancy, including the growth and development of the fetus, the preparation of the uterine lining, and the suppression of the maternal immune response to prevent rejection of the developing fetus.
- Furthermore, in some mammals, the placenta secretes another hormone called relaxin. Relaxin helps in preparing the maternal body for childbirth by relaxing the ligaments and joints of the pelvic region. This relaxation allows for easier passage of the baby through the birth canal during labor and delivery.
- Overall, the placenta serves as a dynamic endocrine organ during pregnancy, secreting hormones such as Chorionic Gonadotropin, estrogens, progesterone, and sometimes relaxin. These hormones are essential for supporting and maintaining a healthy pregnancy, facilitating fetal development, and preparing the mother’s body for childbirth and lactation.
9. Thymus
- The thymus is a gland found in all vertebrates, although its size, number, and location can vary among different species. In humans, it is situated between the upper part of the breastbone (sternum) and the pericardium, which is the protective membrane around the heart. The thymus undergoes significant development during childhood and reaches its peak size around the age of 14 to 15 years. However, as individuals reach adulthood, the thymus gradually decreases in size and undergoes a process called atrophy.
- The thymus is considered a dual-function organ, as it contains both endocrine and lymphoid tissue. The endocrine part of the thymus is responsible for secreting several hormones, including thymosin, thymin I, and thymin II. These hormones play a role in regulating the amount of acetylcholine at the neuromuscular junctions of skeletal muscles. Acetylcholine is a neurotransmitter involved in muscle contraction, and the hormones from the thymus help maintain the proper balance of this neurotransmitter.
- Hypersecretion of these thymic hormones can lead to a condition known as myasthenia gravis, characterized by muscle weakness and fatigue. In myasthenia gravis, the excessive thymic hormones disrupt the normal functioning of acetylcholine, impairing the communication between nerves and muscles.
- During childhood, the thymus also serves as a primary lymphoid organ. It plays a vital role in the maturation and development of T lymphocytes (or T cells), which are a type of white blood cell involved in the immune response. The thymus provides an environment where T cells mature and acquire their specific functions.
- Additionally, the thymus aids in the production of antibodies and contributes to the establishment of immune tolerance. It helps the body recognize “self” from “non-self” to prevent the immune system from attacking its own cells and tissues. Through a process called thymic education, immature T cells undergo selection and maturation within the thymus, ensuring the production of functional T cells that can effectively fight against pathogens while avoiding harmful immune responses against the body’s own tissues.
- In summary, the thymus is a gland with both endocrine and lymphoid functions. It secretes hormones that regulate acetylcholine levels in skeletal muscles and contribute to the proper functioning of the neuromuscular junctions. During childhood, the thymus plays a crucial role in the maturation of T cells, production of antibodies, and establishment of immune tolerance. However, as individuals age, the thymus gradually decreases in size and activity, reflecting its importance primarily during early stages of development and immune system education.
10. Pineal Body
- The pineal body, also known as the pineal gland or epiphysis, is a functional gland in lower vertebrates but tends to atrophy in humans around the age of 7 years. It is located between the anterior corpora quadrigemina on the dorsal side of the brain and can have a stalk-like, cone-shaped, or pea-sized structure (as seen in rabbits).
- In lower vertebrates, the pineal body plays a significant role in producing a hormone called melatonin. Melatonin is involved in various physiological processes, including regulating the sleep-wake cycle and influencing seasonal and daily behaviors in animals. One of its effects is the stimulation of melanophores, cells responsible for the production and distribution of melanin pigments in the skin. Melatonin concentrates melanin, resulting in lighter skin coloration. This action is in contrast to the effect of another hormone called MSH (melanocyte-stimulating hormone), which promotes the dispersion of melanin and darkens the skin.
- Furthermore, melatonin has been found to inhibit gametogenesis (the production of gametes) and the secretion of gonadal hormones in laboratory animals. Increased melatonin secretion can delay sexual maturation in immature animals, while its removal in children may lead to premature puberty. Therefore, the pineal body and its hormone play a role in the regulation of sexual development and maturation.
- The pineal body also has an association with the regulation of biological rhythms and the circadian clock in animals. The secretion of melatonin follows a distinct pattern, with higher levels being produced during darkness and lower levels during daylight. This pattern helps synchronize an organism’s physiological functions with the environmental cycle of day and night. Thus, the pineal body and melatonin contribute to the regulation of circadian behavior and the biological clock in animals.
- However, the specific role of the pineal body in humans is still not fully understood. While the pineal gland continues to exist in humans, its function and significance in adulthood are uncertain. Research suggests that melatonin may still play a role in regulating circadian rhythms and influencing sleep patterns in humans, but further investigation is needed to fully elucidate its functions and potential effects on human physiology.
- In summary, the pineal body is a gland that produces melatonin in lower vertebrates. It influences skin pigmentation, regulates sexual maturation, and plays a role in the circadian rhythms and biological clocks of animals. Although the pineal body tends to atrophy in humans at a young age, its exact role in human physiology remains unclear and requires further study.
11. Gastrointestinal Mucosa
The gastrointestinal mucosa, the inner lining of the gastrointestinal (GI) tract, plays a vital role in the digestive processes. Within the glandular cells of the GI mucosa, several hormones are produced that regulate the secretion and flow of digestive enzymes into the lumen of the GI tract.
These hormones, which are protein hormones, have specific functions and contribute to the overall digestive function of the body. Let’s explore some of these hormones:
- Gastrin: Produced by the mucous membrane in the pyloric region of the stomach, gastrin is stimulated by the presence of food in the stomach. Gastrin stimulates the secretion of gastric juices, such as hydrochloric acid (HCl), and enzymes from the oxyntic and peptic cells of the stomach mucosa. These secretions aid in the breakdown of food and the initiation of the digestive process in the stomach.
- Secretin: Secretin is secreted by the duodenal mucosa in response to the presence of food in the duodenum, the first part of the small intestine. Its target organ is the pancreas. Secretin promotes the secretion of pancreatic juice from the pancreas, which contains digestive enzymes and bicarbonate ions. This secretion helps neutralize the acidic chyme entering the duodenum from the stomach and creates an optimal pH for the activity of pancreatic enzymes.
- Pancreozymin: Also secreted by the duodenal mucosa, pancreozymin has a similar target organ as secretin, which is the pancreas. This hormone regulates the amount of pancreatic enzymes to be secreted, complementing the role of secretin, which controls the volume of pancreatic juice. Together, secretin and pancreozymin ensure the appropriate secretion of enzymes for effective digestion.
- Cholecystokinin: When food enters the duodenum, the duodenal mucosa secretes cholecystokinin (CCK). This hormone targets the gallbladder and stimulates its rhythmic contraction, facilitating the release of bile into the duodenum. Bile aids in the emulsification and digestion of fats, ensuring their proper absorption.
- Enterocrinin: Enterocrinin is secreted by the mucous membrane of both the small and large intestine. It stimulates the small intestine to produce intestinal juice, also known as succus entericus. Intestinal juice is a mixture of various enzymes, such as peptidases, disaccharidases, and lipases, which further assist in the digestion and absorption of nutrients in the small intestine.
- Enterogastrone: In response to the presence of fat in the small intestine, the intestinal mucosa produces enterogastrone. This hormone acts to inhibit the secretion of gastric juice in the stomach, serving as a protective adaptation. By controlling excessive hydrochloric acid (HCl) secretion in the stomach, enterogastrone helps prevent potential damage to the gastric mucosa.
These hormones, produced by the glandular cells of the gastrointestinal mucosa, regulate various aspects of the digestive process. They control the secretion of digestive enzymes, stimulate the release of bile, and influence the overall function of the digestive system. Through their precise coordination, these hormones ensure efficient digestion and absorption of nutrients, contributing to the overall health and well-being of the organism.
12. Kidney
The kidney, an essential organ of the urinary system, plays a crucial role in maintaining homeostasis in the body. In addition to its primary functions in filtration and excretion, the kidney also possesses an endocrine function, producing hormones that influence various physiological processes.
Two important hormones produced by the endocrine part of the kidney are renin and erythropoietin:
- Renin: Renin is an enzyme produced and released by specialized cells in the kidney known as juxtaglomerular cells. Its primary role is to regulate blood pressure. When the kidney detects low blood pressure or reduced blood flow, such as in the case of anoxia (a condition of oxygen deficiency in the blood), it releases renin into the bloodstream. Renin initiates a cascade of reactions that ultimately lead to the production of angiotensin II, a potent vasoconstrictor. This vasoconstriction helps to raise blood pressure, thus restoring blood flow to vital organs.
- Erythropoietin: Erythropoietin (EPO) is a hormone produced by specialized cells in the kidney known as interstitial fibroblasts. Its primary function is to stimulate the production of red blood cells (RBCs) in the bone marrow. When the kidney detects a decrease in oxygen levels, such as in the case of anemia or reduced oxygen-carrying capacity of the blood, it increases the production and release of erythropoietin. Erythropoietin then acts on the bone marrow, stimulating the production of new RBCs. This process helps to maintain adequate oxygen-carrying capacity in the blood and ensures oxygen delivery to tissues throughout the body.
Both renin and erythropoietin play crucial roles in maintaining homeostasis in the body. Renin helps regulate blood pressure, while erythropoietin stimulates the production of RBCs, ensuring adequate oxygen supply to tissues. These hormones represent the kidney’s endocrine function and demonstrate its ability to respond to changes in the body’s physiological needs.
It is important to note that the kidney’s endocrine function is just one aspect of its overall function. The kidney also performs vital roles in regulating fluid and electrolyte balance, acid-base balance, and waste product excretion. Together, these functions contribute to the kidney’s vital role in maintaining overall health and homeostasis in the body.
13. Heart
- The heart, an extraordinary organ at the center of our circulatory system, not only plays a vital role in pumping blood throughout the body but also has intriguing secrets hidden within its chambers. One such secret lies in the hormone known as atriopeptin, which is secreted by the heart itself.
- Atriopeptin, also called atrial natriuretic peptide (ANP), is a remarkable hormone that acts as a messenger between the heart and other organs, influencing various physiological processes. Primarily, it exerts its effects on blood vessels, offering a unique ability to regulate blood pressure. When released into the bloodstream, atriopeptin works to relax the walls of blood vessels, promoting vasodilation. This dilation widens the vessels and reduces peripheral resistance, resulting in a decrease in blood pressure. By modulating vascular tone, atriopeptin helps maintain a delicate balance within the cardiovascular system.
- In addition to its impact on blood vessels, atriopeptin also plays a crucial role in kidney function. This hormone interacts with the kidneys to regulate fluid balance within the body. When atriopeptin reaches the kidneys, it acts on the specialized cells within the nephrons, the functional units of the kidney. Here, it stimulates the excretion of sodium and water, leading to increased urine production. By promoting the elimination of excess fluid, atriopeptin helps to maintain the body’s fluid balance, ensuring that it stays within optimal levels.
- The intricate interplay between the heart, blood vessels, and kidneys underscores the significance of atriopeptin in maintaining homeostasis within the body. This hormone acts as a natural regulator, fine-tuning blood pressure and fluid levels to ensure the proper functioning of vital organs.
- Beyond its physiological functions, the discovery of atriopeptin serves as a reminder of the complexities inherent within the human body. It highlights the interconnectedness of organs and the multifaceted roles they play, often extending beyond their primary functions. The heart, traditionally known as a powerful pump, now reveals itself as a sophisticated communicator, secreting hormones that influence various physiological processes.
- Understanding the intricate mechanisms of hormones like atriopeptin not only expands our knowledge of the human body but also paves the way for potential therapeutic interventions. Researchers and medical professionals continue to delve deeper into the complexities of these fascinating hormonal interactions, exploring their implications for cardiovascular health and disease management.
- In conclusion, atriopeptin, the hormone secreted by the heart, showcases the remarkable capabilities of this vital organ. Its effects on blood vessels, reducing blood pressure, and its role in maintaining fluid balance through the kidneys demonstrate the intricate web of communication within the body. The discovery and study of atriopeptin shed light on the hidden complexities of the heart, further deepening our understanding of its crucial role in maintaining overall health and well-being.
FAQ
What is the endocrine system?
The endocrine system is a network of glands that produce and release hormones into the bloodstream. These hormones act as chemical messengers, regulating various bodily functions and maintaining homeostasis.
What are the main glands of the endocrine system?
The major glands of the endocrine system include the hypothalamus, pituitary gland, thyroid gland, parathyroid glands, adrenal glands, pancreas, ovaries (in females), and testes (in males).
What are hormones?
Hormones are chemical substances produced by the endocrine glands that travel through the bloodstream to target cells or organs. They regulate processes such as growth and development, metabolism, reproduction, and mood.
How do hormones work?
Hormones bind to specific receptor sites on target cells or organs, triggering a response within those cells. This response can involve changes in gene expression, cellular activity, or the release of other hormones.
What does the pituitary gland do?
Often referred to as the “master gland,” the pituitary gland produces and releases hormones that control the functions of other endocrine glands. It regulates growth, reproduction, metabolism, and the balance of other hormones in the body.
What is the role of the hypothalamus in the endocrine system?
The hypothalamus acts as the control center for the endocrine system. It produces hormones that regulate the pituitary gland and influences other endocrine glands. The hypothalamus also plays a role in maintaining body temperature, hunger, thirst, and sleep.
What is the function of the thyroid gland?
The thyroid gland produces hormones that regulate metabolism, growth, and development. It helps control the rate at which the body uses energy, maintains body temperature, and influences the function of various organs.
What is the role of the adrenal glands?
The adrenal glands produce hormones that are essential for stress response and regulation of metabolism. They secrete cortisol, which helps the body respond to stress, and aldosterone, which regulates electrolyte balance and blood pressure.
How does the pancreas contribute to the endocrine system?
The pancreas produces hormones such as insulin and glucagon, which are involved in regulating blood sugar levels. Insulin helps lower blood sugar, while glucagon raises it, maintaining a delicate balance necessary for proper cellular function.
How can endocrine disorders be diagnosed and treated?
Endocrine disorders are diagnosed through a combination of medical history, physical examination, blood tests, and imaging studies. Treatment options may include hormone replacement therapy, medications, surgery, or lifestyle modifications, depending on the specific disorder and its underlying cause. A specialist called an endocrinologist is typically involved in the diagnosis and management of endocrine disorders.
References
- https://opentextbc.ca/biology/chapter/11-4-endocrine-system/
- https://uta.pressbooks.pub/histology/chapter/endocrine-system/
- https://uomustansiriyah.edu.iq/media/lectures/2/2_2017_03_08!01_26_15_PM.pdf
- https://vetmed.tamu.edu/peer/wp-content/uploads/sites/72/2020/04/7-Endocrine-System.pdf
- http://fblt.cz/en/skripta/xi-regulacni-mechanismy-1-endokrinni-regulace/1-funkcni-morfologie-endokrinniho-systemu/
- https://www.hopkinsmedicine.org/health/wellness-and-prevention/anatomy-of-the-endocrine-system
- https://biologydictionary.net/endocrine-system/
- https://www.biologydiscussion.com/chemical-coordination/endocrine-glands-of-human-beings-with-diagram/5124
- https://www.biologydiscussion.com/endocrinology/endocrine-gland-definition-development-and-classification/18427


