Table of Contents
What is Hormone?
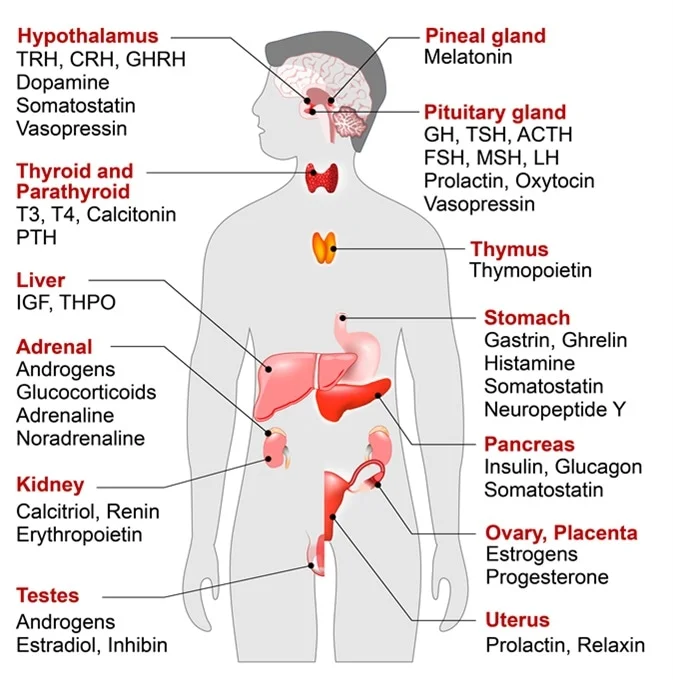
- A hormone is a type of signaling molecule found in multicellular organisms that plays a crucial role in regulating various physiological and behavioral processes. The word “hormone” originates from the Greek term “ὁρμῶν,” which means “setting in motion.” Hormones are essential for the proper development and functioning of animals, plants, and fungi. They are responsible for coordinating communication between different organs and tissues within an organism.
- Hormones encompass a diverse range of molecules due to their broad definition as signaling molecules that exert their effects far from their site of production. Some examples of substances that can be classified as hormones include eicosanoids (such as prostaglandins and thromboxanes), steroids (such as estrogen and brassinosteroid), amino acid derivatives (such as epinephrine and auxin), protein or peptides (such as insulin and CLE peptides), and gases (such as ethylene and nitric oxide).
- In vertebrates, hormones regulate a wide array of physiological processes and behavioral activities. These include digestion, metabolism, respiration, sensory perception, sleep, excretion, lactation, stress responses, growth and development, movement, reproduction, and mood regulation. In plants, hormones modulate nearly all aspects of development, from seed germination to aging.
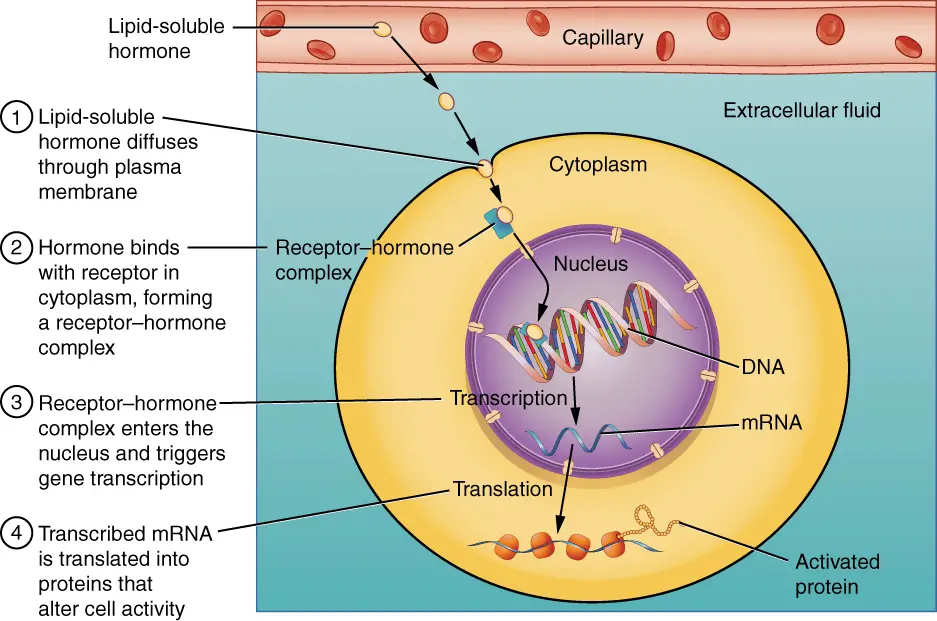
- Hormones exert their effects by binding to specific receptor proteins on target cells, leading to changes in cell function. When a hormone attaches to its receptor, it initiates a signal transduction pathway that typically activates gene transcription, resulting in increased expression of specific proteins. Hormones can also act through non-genomic pathways that complement their genomic effects.
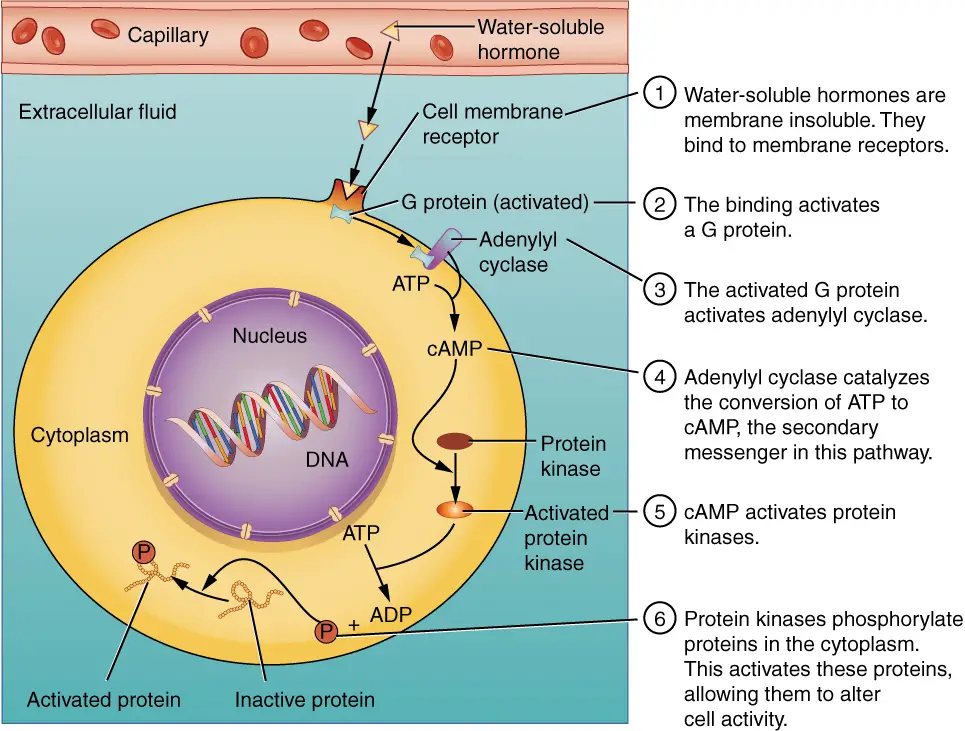
- Water-soluble hormones, such as peptides and amines, generally act on the surface of target cells through second messengers. On the other hand, lipid-soluble hormones, like steroids, can pass through both cytoplasmic and nuclear membranes to act within the nuclei of target cells. Brassinosteroids, a type of plant hormone, are unique lipid-soluble hormones that attach to their receptor at the cell surface, despite their lipid solubility. These hormones have shown potential as anticancer drugs for endocrine-responsive tumors by inducing apoptosis and limiting plant growth.
- In vertebrates, endocrine glands are specialized organs responsible for secreting hormones into the endocrine signaling system. The secretion of hormones is triggered by specific biochemical signals and is often regulated by negative feedback mechanisms. For example, high blood sugar levels stimulate the synthesis of insulin, which then acts to reduce glucose levels and maintain homeostasis, ultimately leading to decreased insulin production. Water-soluble hormones can easily travel through the circulatory system upon secretion, while lipid-soluble hormones require carrier plasma glycoproteins to form ligand-protein complexes. Some hormones, known as prohormones, need to undergo a series of controlled steps for activation within specific cells.
- The endocrine system releases hormones directly into the bloodstream, usually through fenestrated capillaries. In contrast, the exocrine system indirectly secretes hormones using ducts. Hormones with paracrine function diffuse through interstitial spaces to reach nearby target tissues.
- Unlike vertebrates, plants do not possess specialized hormone-secreting organs. Instead, hormone production is distributed spatially. For instance, the hormone auxin is primarily produced at the tips of young leaves and in the shoot apical meristem. The absence of specialized glands allows the main site of hormone production to change throughout a plant’s lifespan, depending on its age and environmental conditions.
| Endocrine Glands and Their Major Hormones | |||
|---|---|---|---|
| Endocrine gland | Associated hormones | Chemical class | Effect |
| Pituitary (anterior) | Growth hormone (GH) | Peptide | Promotes growth of body tissues |
| Pituitary (anterior) | Prolactin (PRL) | Peptide | Promotes milk production |
| Pituitary (anterior) | Thyroid-stimulating hormone (TSH) | Peptide | Stimulates thyroid hormone release |
| Pituitary (anterior) | Adrenocorticotropic hormone (ACTH) | Peptide | Stimulates hormone release by adrenal cortex |
| Pituitary (anterior) | Follicle-stimulating hormone (FSH) | Peptide | Stimulates gamete production |
| Pituitary (anterior) | Luteinizing hormone (LH) | Peptide | Stimulates androgen production by gonads |
| Pituitary (posterior) | Antidiuretic hormone (ADH) | Peptide | Stimulates water reabsorption by kidneys |
| Pituitary (posterior) | Oxytocin | Peptide | Stimulates uterine contractions during childbirth |
| Thyroid | Thyroxine (T4), triiodothyronine (T3) | Amine | Stimulate basal metabolic rate |
| Thyroid | Calcitonin | Peptide | Reduces blood Ca2+ levels |
| Parathyroid | Parathyroid hormone (PTH) | Peptide | Increases blood Ca2+ levels |
| Adrenal (cortex) | Aldosterone | Steroid | Increases blood Na+ levels |
| Adrenal (cortex) | Cortisol, corticosterone, cortisone | Steroid | Increase blood glucose levels |
| Adrenal (medulla) | Epinephrine, norepinephrine | Amine | Stimulate fight-or-flight response |
| Pineal | Melatonin | Amine | Regulates sleep cycles |
| Pancreas | Insulin | Peptide | Reduces blood glucose levels |
| Pancreas | Glucagon | Peptide | Increases blood glucose levels |
| Testes | Testosterone | Steroid | Stimulates development of male secondary sex characteristics and sperm production |
| Ovaries | Estrogens and progesterone | Steroid | Stimulate development of female secondary sex characteristics and prepare the body for childbirth |
Definition of Hormone
A hormone is a signaling molecule produced by multicellular organisms that regulates physiological processes and behaviors by communicating between organs and tissues.
Characteristics Features of Hormone
- Signaling Molecules: Hormones are specific signaling molecules that transmit information and instructions between cells, tissues, and organs within an organism.
- Regulation: Hormones play a regulatory role in various physiological processes and behaviors, including growth, development, metabolism, reproduction, and homeostasis.
- Distance Communication: Hormones act by being secreted from one location and exerting their effects on distant target cells or organs. They can travel through the bloodstream or diffuse through interstitial spaces to reach their target sites.
- Receptor Binding: Hormones interact with specific receptor proteins on the surface or within target cells. This binding triggers a cascade of molecular events, resulting in cellular responses and changes in gene expression.
- Diverse Chemical Nature: Hormones encompass a wide range of chemical structures, including peptides, proteins, steroids, amino acid derivatives, eicosanoids, and gases.
- Feedback Regulation: Hormone secretion is often subject to feedback regulation to maintain homeostasis. Negative feedback loops control hormone levels by adjusting their production in response to physiological signals.
- Specificity and Selectivity: Hormones exhibit specificity in their actions, targeting specific cells or tissues that possess the appropriate receptor proteins. Different hormones have distinct target sites and physiological effects.
- Synergistic and Complementary Actions: Hormones can interact with each other, leading to synergistic or complementary effects. They may act together to regulate complex physiological processes and achieve coordinated responses.
- Lipid Solubility: Some hormones are lipid-soluble, allowing them to pass through cell membranes and directly influence gene expression by interacting with nuclear receptors. Other hormones are water-soluble and act through cell surface receptors and intracellular signaling pathways.
- Spatial Distribution: In plants, hormone production is spatially distributed rather than concentrated in specialized glands. Hormones are synthesized in specific regions or tissues, and their levels can vary depending on the plant’s age and environmental conditions.
Structure of Hormone
Hormones are chemical messengers produced by various glands and tissues in the body. They play a crucial role in regulating and coordinating numerous physiological processes. The structure of hormones varies depending on their classification into different chemical groups: peptide/protein hormones, steroid hormones, and amino acid-derived hormones.
- Peptide/Protein Hormones: Peptide and protein hormones are composed of chains of amino acids. Peptide hormones consist of relatively short amino acid chains, while protein hormones are longer chains. These chains may be cleaved from larger precursor molecules during hormone synthesis. Examples of peptide hormones include insulin, glucagon, growth hormone, and antidiuretic hormone (ADH). Protein hormones include follicle-stimulating hormone (FSH), luteinizing hormone (LH), and human chorionic gonadotropin (hCG).
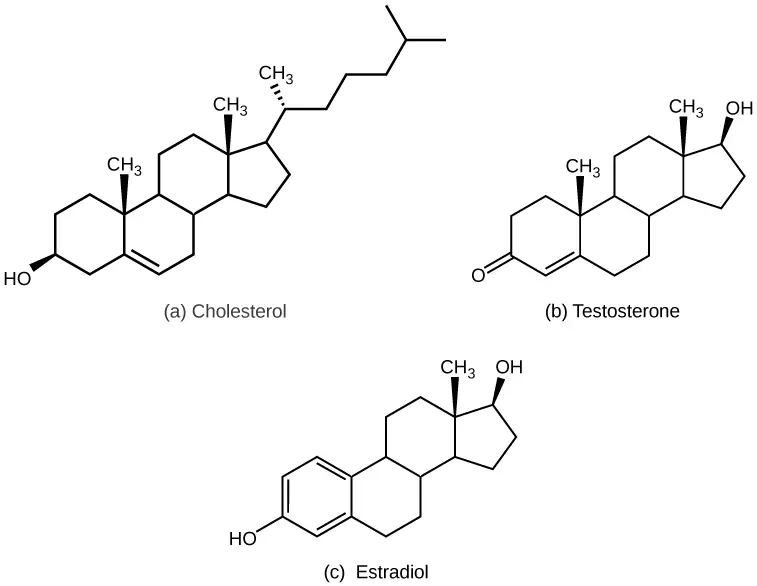
- Steroid Hormones: Steroid hormones are derived from cholesterol and have a characteristic ring structure. They are lipophilic (fat-soluble) and can diffuse across cell membranes. Steroid hormones include hormones produced by the adrenal cortex (such as cortisol and aldosterone) and sex hormones produced by the gonads (such as estrogen, progesterone, and testosterone).
- Amino Acid-Derived Hormones: Amino acid-derived hormones are derived from specific amino acids. Two notable examples are epinephrine (adrenaline) and norepinephrine (noradrenaline), which are derived from the amino acid tyrosine. These hormones are produced in the adrenal medulla and play a role in the body’s response to stress and the regulation of cardiovascular function.
It is important to note that hormone structure extends beyond their chemical composition. Hormones exert their effects by binding to specific receptors located on target cells throughout the body. The interaction between hormones and their receptors initiates a cascade of cellular events that mediate the hormone’s physiological effects.
Overall, the structure of hormones varies depending on their classification, and this structural diversity contributes to their distinct functions and mechanisms of action in the body.
Types of Hormone (Classification of Hormone)
Hormones can be classified based on their chemical nature and mechanism of action.
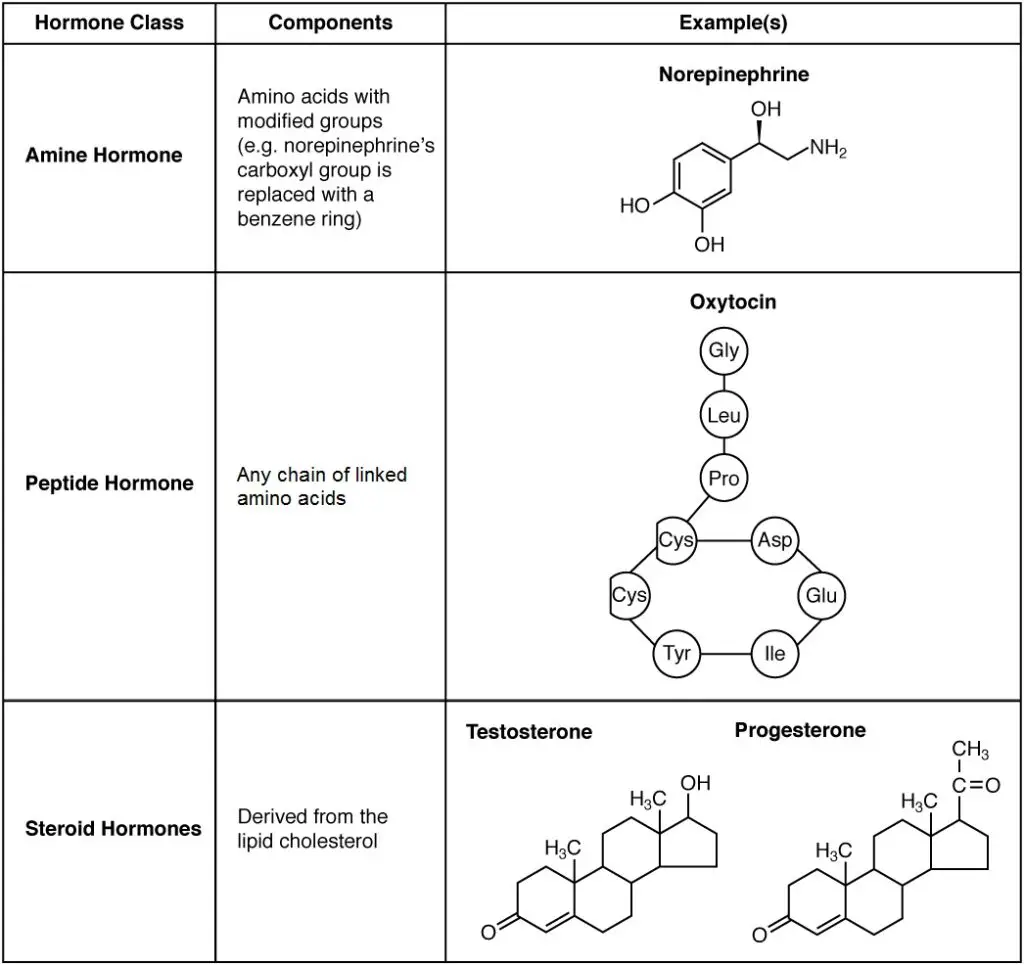
A. On the basis of chemical nature:
1. Peptide Hormones
Peptide hormones are a type of hormone composed of short chains of amino acids. They are synthesized in cells as larger precursor molecules, which are then cleaved into their active form through post-translational modification.
Peptide hormones are produced by various glands and tissues in the body, including the hypothalamus, pituitary gland, pancreas, and gastrointestinal tract. They play important roles in regulating numerous physiological processes and maintaining homeostasis.
Examples of peptide hormones include:
- Insulin: Produced by the beta cells of the pancreas, insulin regulates glucose metabolism by promoting the uptake of glucose into cells and the storage of glucose as glycogen in the liver and muscles. It helps to lower blood glucose levels.
- Glucagon: Secreted by the alpha cells of the pancreas, glucagon has the opposite effect of insulin. It stimulates the breakdown of glycogen in the liver, leading to the release of glucose into the bloodstream. Glucagon raises blood glucose levels.
- Growth hormone (GH): Produced by the anterior pituitary gland, GH stimulates growth and development in children and has metabolic effects in adults. It promotes cell growth, protein synthesis, and the breakdown of fats for energy.
- Oxytocin: Released by the posterior pituitary gland, oxytocin plays a role in reproductive functions and social bonding. It stimulates uterine contractions during childbirth and promotes milk ejection during breastfeeding. It is also involved in emotional bonding and social interactions.
- Adrenocorticotropic hormone (ACTH): Produced by the anterior pituitary gland, ACTH stimulates the adrenal glands to release cortisol, a hormone involved in stress response and regulation of metabolism, immune function, and inflammation.
- Antidiuretic hormone (ADH): Also known as vasopressin, ADH is produced by the hypothalamus and released by the posterior pituitary gland. It regulates water balance by controlling the reabsorption of water in the kidneys, reducing urine output, and conserving water in the body.
These are just a few examples of the many peptide hormones found in the body. Peptide hormones typically act by binding to specific receptors on target cells, initiating signaling pathways that regulate various cellular processes and physiological functions.
2. Protein Hormones
Protein hormones are a type of hormone composed of longer polypeptide chains or proteins. They are synthesized in cells as larger precursor molecules, which undergo post-translational modifications to form the active hormone.
Protein hormones are produced by various glands and tissues in the body, including the pituitary gland, thyroid gland, parathyroid glands, and pancreas. They play crucial roles in regulating various physiological processes and maintaining homeostasis.
Here are some examples of protein hormones:
- Growth Hormone (GH): Produced by the anterior pituitary gland, GH stimulates growth and development in children and has metabolic effects in adults. It promotes cell growth, protein synthesis, and the breakdown of fats for energy.
- Thyroid-Stimulating Hormone (TSH): Secreted by the anterior pituitary gland, TSH regulates the production and release of thyroid hormones (T3 and T4) from the thyroid gland. It controls the metabolism, growth, and development of cells throughout the body.
- Parathyroid Hormone (PTH): Produced by the parathyroid glands, PTH regulates calcium and phosphate levels in the blood. It increases calcium release from bones, enhances calcium reabsorption in the kidneys, and stimulates the production of active vitamin D, which promotes calcium absorption from the intestines.
- Insulin-like Growth Factors (IGFs): Produced by the liver and other tissues, IGFs are stimulated by GH and play a role in promoting growth and development. They act on various target tissues, promoting cell division, protein synthesis, and tissue growth.
- Insulin: Secreted by the beta cells of the pancreas, insulin regulates glucose metabolism. It promotes the uptake of glucose into cells, particularly in muscle and adipose tissue, and regulates carbohydrate, protein, and lipid metabolism. Insulin helps lower blood glucose levels.
- Glucagon-like Peptide-1 (GLP-1): Secreted by the intestine in response to food intake, GLP-1 stimulates insulin release from the pancreas, inhibits glucagon secretion, and slows down gastric emptying. It helps regulate blood glucose levels and plays a role in appetite control.
Protein hormones typically exert their effects by binding to specific receptors on the surface of target cells. This binding initiates intracellular signaling pathways, leading to various cellular responses and the regulation of physiological functions. Protein hormones are water-soluble and cannot pass through the cell membrane, so their receptors are located on the cell surface.
3. Steroid hormones
Steroid hormones are a type of hormone derived from lipids, specifically cholesterol. They play essential roles in regulating various physiological processes in the body. Examples of steroid hormones include testosterone and estrogen, which are reproductive hormones produced by the gonads (testes and ovaries), as well as aldosterone and cortisol, which are produced by the adrenal glands.
One characteristic of steroid hormones is their hydrophobic nature, meaning they are not soluble in water. Since blood is primarily water-based, steroid hormones require transport proteins to travel through the bloodstream to reach their target cells. The binding of steroid hormones to transport proteins extends their half-life, which is the time required for half the concentration of the hormone to be degraded. For instance, cortisol, a lipid-derived hormone, has a half-life of approximately 60 to 90 minutes, while the amino acid-derived hormone epinephrine has a much shorter half-life of approximately one minute.
Unlike peptide hormones, steroid hormones are able to pass through cell membranes due to their fat-soluble nature. This enables them to bind to intracellular receptors located in the cytoplasm or nucleus of target cells. Once inside the cell, the steroid hormone-receptor complex undergoes a series of molecular interactions that regulate gene expression. This ultimately leads to the production of new proteins and the physiological response associated with the specific hormone.
Steroid hormones are involved in a wide range of biological functions, including sexual development and reproduction, stress response, metabolism, electrolyte balance, and immune system regulation. They exert their effects by modulating gene expression and protein synthesis in target tissues, thereby influencing cellular processes and overall physiological responses.
Overall, steroid hormones are important regulators of numerous bodily functions and play a vital role in maintaining homeostasis and coordinating various physiological processes.
Some examples of steroid hormones include:
- Testosterone: Testosterone is the primary male sex hormone. It is responsible for the development and maintenance of male reproductive tissues, as well as secondary sexual characteristics like muscle mass, bone density, and facial hair.
- Estrogen: Estrogen refers to a group of hormones including estradiol, estrone, and estriol. These hormones are predominantly produced in the ovaries in females and play a crucial role in the development and maintenance of female reproductive organs, regulation of the menstrual cycle, and the development of secondary sexual characteristics.
- Progesterone: Progesterone is a hormone involved in the menstrual cycle and pregnancy. It prepares the uterus for implantation of a fertilized egg and helps maintain pregnancy.
- Cortisol: Cortisol, often referred to as the stress hormone, is produced by the adrenal glands. It plays a role in regulating the body’s response to stress, metabolism, immune system function, and inflammation.
- Aldosterone: Aldosterone is a hormone produced by the adrenal glands that regulates electrolyte balance, particularly the reabsorption of sodium and the excretion of potassium in the kidneys. It helps maintain blood pressure and fluid balance in the body.
- DHEA (Dehydroepiandrosterone): DHEA is a precursor hormone that is converted into other steroid hormones, including testosterone and estrogen. It plays a role in the development of secondary sexual characteristics and overall well-being.
These are just a few examples of steroid hormones. There are additional steroid hormones with specific functions and roles in the body, each contributing to various physiological processes and maintaining homeostasis.
4. Amino acid derivatives hormones
Amino acid derivative hormones, also known as amine hormones, are derived from the modification of specific amino acids. These hormones retain the amine (-NH3+) group while the carboxyl (-COOH) group is removed during the modification process.
Two amino acids commonly involved in the synthesis of amine hormones are tryptophan and tyrosine. From tryptophan, the hormone melatonin is produced. Melatonin is primarily secreted by the pineal gland and plays a crucial role in regulating circadian rhythms and sleep-wake cycles.
On the other hand, tyrosine derivatives give rise to several important hormones. Thyroid hormones, such as triiodothyronine (T3) and thyroxine (T4), are produced by the thyroid gland and are involved in regulating metabolism and growth throughout the body.
Tyrosine is also the precursor for catecholamines, which include hormones like epinephrine (adrenaline), norepinephrine (noradrenaline), and dopamine. Epinephrine and norepinephrine are secreted by the adrenal medulla and are involved in the body’s response to stress, triggering the fight-or-flight response. Dopamine, produced by the hypothalamus, inhibits the release of certain hormones from the anterior pituitary gland.
These amine hormones are relatively small molecules and are involved in various physiological processes in the body. Their production and release are tightly regulated to maintain homeostasis and ensure proper functioning of the body’s systems.
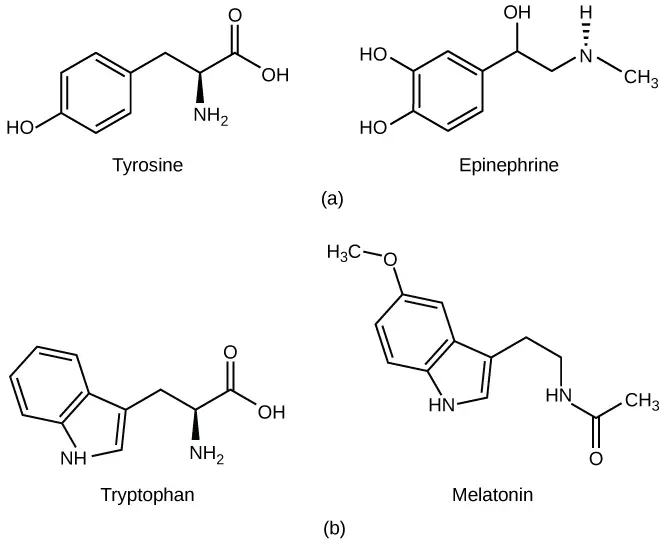
Examples of amino acid derivative hormones include:
- Melatonin: Derived from the amino acid tryptophan, melatonin is primarily produced by the pineal gland in the brain. It regulates the sleep-wake cycle and helps synchronize the body’s internal biological rhythms with the external environment.
- Thyroid hormones (Triiodothyronine – T3 and Thyroxine – T4): Synthesized by the thyroid gland, these hormones are derived from the amino acid tyrosine. Thyroid hormones play a crucial role in regulating metabolism, growth, and development in the body.
- Epinephrine (adrenaline): Produced by the adrenal medulla, epinephrine is a catecholamine derived from the amino acid tyrosine. It is released in response to stress or emergency situations, increasing heart rate, boosting energy, and preparing the body for “fight or flight” response.
- Norepinephrine (noradrenaline): Another catecholamine derived from tyrosine and produced in the adrenal medulla, norepinephrine acts as a neurotransmitter and hormone. It plays a role in regulating blood pressure, heart rate, and the body’s response to stress.
- Dopamine: Derived from tyrosine and produced in various regions of the brain, dopamine acts as a neurotransmitter and hormone. It is involved in the regulation of movement, mood, motivation, and reward pathways.
These amino acid derivative hormones have diverse functions and play critical roles in the body’s physiological processes and overall well-being.
5. Glycoprotein Hormones
Glycoprotein hormones are a type of hormone that have a glycoprotein structure, meaning they are composed of both protein and carbohydrate components. The carbohydrate groups attached to the protein backbone of these hormones include mannose, galactose, fucose, and others.
Examples of glycoprotein hormones include:
- Luteinizing Hormone (LH): LH is produced and released by the anterior pituitary gland. It plays a crucial role in regulating the reproductive system in both males and females. In females, LH stimulates ovulation and the production of progesterone by the ovaries. In males, LH stimulates the production of testosterone by the testes.
- Follicle-Stimulating Hormone (FSH): Also produced by the anterior pituitary gland, FSH works in conjunction with LH to regulate the reproductive system. In females, FSH stimulates the growth and maturation of ovarian follicles, which contain the eggs. In males, FSH stimulates the production of sperm in the testes.
- Thyroid-Stimulating Hormone (TSH): TSH is released by the anterior pituitary gland and acts on the thyroid gland. It stimulates the thyroid gland to produce and release thyroid hormones, such as thyroxine (T4) and triiodothyronine (T3), which are involved in regulating metabolism, growth, and development.
Glycoprotein hormones play vital roles in reproductive function and the regulation of hormone production in the body. The presence of carbohydrate groups in their structure allows for proper folding, stability, and interaction with specific receptors on target cells.
6. Eicosanoids Hormones
- Eicosanoids are a group of hormone-like signaling molecules derived from polyunsaturated fatty acids, particularly arachidonic acid. They play diverse roles in inflammation, immune response, blood clotting, and other physiological processes. Prostaglandins are a well-known class of eicosanoids.
- Prostaglandins are synthesized from arachidonic acid by the action of enzymes called cyclooxygenases (COX). They act as local hormones, exerting their effects in the immediate vicinity of their synthesis. Prostaglandins are involved in various biological functions, including regulating inflammation, blood flow, smooth muscle contraction, and platelet aggregation.
- The effects of prostaglandins can be wide-ranging and depend on the specific type and location of their receptors. For example, some prostaglandins can cause inflammation and pain, while others promote vasodilation or vasoconstriction, influencing blood pressure regulation. Prostaglandins also play a role in reproductive processes, such as inducing labor contractions and controlling the menstrual cycle.
- Eicosanoids, particularly prostaglandins, are highly influential in modulating various physiological processes and are involved in both normal and pathological conditions. They act as local mediators, exerting their effects in a paracrine or autocrine manner, meaning they act on nearby cells or the same cells that produced them. Their rapid synthesis and short half-life allow for precise control and regulation of cellular responses.
- In summary, eicosanoids, such as prostaglandins, are small hormone-like molecules derived from arachidonic acid. They play significant roles in inflammation, immune response, blood clotting, and other physiological processes, acting as local mediators with diverse effects on target cells.
B. On the basis of mechanism of hormone action
- Group I hormones (lipophilic hormones):
- These hormones are lipophilic in nature, meaning they are lipid-soluble.
- They are usually derivatives of cholesterol.
- They bind to intracellular receptors located inside the target cells.
- Examples include steroid hormones (estrogen, androgen, glucocorticoids), thyroxine, and cholecalciferol.
- Group II hormones (water-soluble hormones):
- These hormones bind to cell surface receptors located on the outer surface of target cells.
- They stimulate the release of secondary messengers, which are molecules that mediate the hormone’s effects inside the cell.
- Based on the specific secondary messenger involved, group II hormones can be further categorized:
- i. Secondary messenger is cAMP (cyclic adenosine monophosphate): Examples include adrenocorticotropic hormone (ACTH), follicle-stimulating hormone (FSH), luteinizing hormone (LH), parathyroid hormone (PTH), antidiuretic hormone (ADH), calcitonin, and glucagon.
- ii. Secondary messenger is phosphatidylinositol/calcium or both: Examples include acetylcholine, vasopressin, cholecystokinin, gastrin, gonadotropin-releasing hormone, thyrotropin-releasing hormone, insulin, chorionic somatomammotropin, epidermal growth factors, fibroblast growth factors, growth hormone (GH), and prolactin.
- iii. Secondary messenger is cGMP (cyclic guanosine monophosphate): An example of this type is atrial natriuretic peptide (ANP).
By understanding the classification of hormones, scientists and healthcare professionals can better understand their chemical properties and mechanisms of action, which is crucial for diagnosing and treating hormonal disorders.
C. Types of Hormones based on Nature of Action
Hormones can be classified based on the nature of their action into two main types: local hormones and general hormones.
(a) Local Hormones
Local hormones, also known as paracrine hormones, have specific effects on nearby cells or tissues. They are released by a cell and act on neighboring cells without entering the bloodstream. One example of a local hormone is testosterone, which is produced by the testes and has localized effects on the reproductive system. Testosterone acts on nearby cells to regulate sperm production and secondary sexual characteristics.
(b) General Hormones
General hormones, also referred to as circulating hormones, are transported throughout the body via the bloodstream to reach their target organs or tissues. These hormones are produced by specialized glands or tissues and are released into the bloodstream, allowing them to exert their effects on distant cells or tissues. Examples of general hormones include insulin, which is produced by the pancreas and acts on various cells in the body to regulate glucose metabolism, and thyroid hormone, which is produced by the thyroid gland and affects multiple organs and tissues to control metabolism and growth.
General hormones are typically synthesized and secreted by endocrine glands located in different parts of the body. They travel through the bloodstream and bind to specific receptors on target cells, initiating a series of cellular responses. The effects of general hormones can be widespread and may impact multiple organ systems.
In summary, based on the nature of their action, hormones can be classified into local hormones, which have specific effects on nearby cells through paracrine secretion, and general hormones, which are transported by the bloodstream to reach distant target organs or tissues. Understanding the classification of hormones based on the nature of their action helps to elucidate how they regulate various physiological processes in the body.
D. Types of Hormones based on Effect
- Kinetic Hormones: Kinetic hormones are a type of hormone that can induce various physiological effects such as pigment migration, muscle contraction, and glandular secretion. These hormones directly influence the movement and activities of different cells and tissues in the body. Examples of kinetic hormones include Pinealin, MSH (Melanocyte-Stimulating Hormone), and Epinephrine.
- Metabolic Hormones: Metabolic hormones primarily function by altering the rate of metabolism and maintaining a balance in biochemical reactions within the body. These hormones regulate the utilization and storage of nutrients, such as carbohydrates, proteins, and fats, and help maintain energy homeostasis. Examples of metabolic hormones include Insulin, Glucagon, and PTH (Parathyroid Hormone).
- Morphogenetic Hormones: Morphogenetic hormones play a crucial role in growth and differentiation processes. They are responsible for regulating the development and maturation of various organs and tissues, as well as promoting cellular differentiation and specialization. Hormones in this category include STH (Somatotropic Hormone or Growth Hormone), LTH (Luteotropic Hormone or Prolactin), FSH (Follicle-Stimulating Hormone), and Thyroid hormones.
Each type of hormone exerts specific effects on the body and contributes to the overall regulation and maintenance of various physiological processes. Understanding the different types of hormones based on their effects is essential in comprehending the intricate mechanisms underlying hormone signaling and their impact on overall health and well-being.
D. Types of Hormones based on Stimulation of Endocrine Glands
Types of Hormones based on Stimulation of Endocrine Glands:
- Tropic Hormones: Tropic hormones are a type of hormone that stimulate the secretion of other endocrine glands. They act by targeting specific endocrine glands and triggering the release of hormones from those glands. The secretion of these hormones subsequently influences various physiological processes in the body. For example, TSH (Thyroid-Stimulating Hormone) secreted by the pituitary gland stimulates the thyroid gland to release thyroid hormones, which play a vital role in regulating metabolism, growth, and development.
- Non-tropic Hormones: Non-tropic hormones are hormones that directly affect non-endocrine target tissues. Rather than stimulating other endocrine glands, these hormones act directly on specific tissues or organs to elicit their effects. They do not trigger the release of hormones from other endocrine glands. An example of a non-tropic hormone is the thyroid hormone. Thyroid hormone, produced by the thyroid gland, influences the metabolic activity and oxygen consumption rate of almost every cell in the body. It affects a wide range of tissues and plays a crucial role in regulating energy metabolism and overall cellular activity.
Synthesis of Hormones
Hormones play a vital role in coordinating a series of physiological events. The synthesis of all hormones is regulated by genetic processes.
1. Synthesis of Peptide Hormones
- The synthesis of peptide hormones involves a series of steps using the translational method. These hormones are created through the transfer of genetic information encoded in DNA, in the form of polynucleotides, to biologically active proteins (hormones) composed of poly-amino acids.
- The synthesis of polypeptide hormones begins with the formation of a precursor molecule known as a pro-hormone. Post-translational modifications, such as enzymatic cleavage, lead to the breakdown of the pro-hormone, resulting in the formation of the active hormone itself.
- The genetic code dictates that protein synthesis occurs in ribosomes following transcription. The pro-hormone initially contains a signal peptide or leader peptide, which is a hydrophobic amino acid sequence located at the amino terminus. This signal peptide plays a crucial role in guiding the pro-hormone into the Golgi complex through the endoplasmic reticulum.
- Within the Golgi complex, enzymatic actions facilitate the conversion of the pro-hormone into the mature hormone. Finally, the hormone is released through exocytosis, allowing it to exert its biological effects. The diagram below provides a schematic representation of the cellular synthesis of peptide hormones.
- Overall, the synthesis of peptide hormones involves the translation of genetic information, the formation of pro-hormones, their transportation through cellular compartments, enzymatic modifications, and the eventual secretion of the active hormones. These intricate steps ensure the proper production and release of peptide hormones, enabling them to carry out their physiological functions.
2. Synthesis of Peptide Hormones
- The synthesis of non-peptide hormones, including thyroid hormones, adrenal medullary hormones, and steroid hormones, requires the involvement of multiple enzymes. Thyroid and medullary hormones are primarily derived from the amino acid tyrosine.
- Steroid hormones, on the other hand, are synthesized from a precursor molecule called cholesterol. The synthesis of non-peptide hormones takes place within cells, where precursor molecules are transformed into the final hormone through a series of sequential enzymatic reactions. These reactions may occur in different cellular compartments such as mitochondria or endoplasmic reticulum.
- Once synthesized, non-peptide hormones can be secreted from the cells through active exocytosis or simple diffusion, depending on the specific hormone and its target tissues.
- Overall, the synthesis of non-peptide hormones involves the conversion of precursor molecules into the final hormone form through the coordinated actions of multiple enzymes. The hormones are then released from the cells to exert their physiological effects on target tissues.
Transport and Metabolism of Hormones
- After secretion, the majority of hormones are released directly into the bloodstream. They travel through the circulatory system to reach their target organs. In some cases, hormones may be bound to carrier proteins while in transit. Alternatively, hormones can be transported through intercellular fluid, particularly in paracrine secretion, where the hormones act on neighboring cells.
- Once hormones have exerted their effects on target tissues, they undergo metabolic degradation. Hormones can be metabolically altered or consumed at the site of action. Typically, degradation occurs in organs such as the liver and kidneys. Subsequently, the degraded hormone molecules are excreted from the body through urine.
- In the case of peptide hormones, they undergo digestion and are broken down into individual amino acids. This process takes place in lysosomes, specialized cellular compartments involved in intracellular digestion.
- Overall, the transport and metabolism of hormones involve their release into the bloodstream or intercellular fluid, binding to carrier proteins, targeting specific organs, metabolic degradation in organs like the liver and kidneys, and excretion from the body. Peptide hormones undergo digestion into amino acids in lysosomes. These processes ensure the regulation and elimination of hormones after their physiological actions have taken place.
Gastrointestinal Hormones and Digestive Secretions
There are several important gastrointestinal hormones that play a crucial role in regulating digestive secretions. These hormones include:
- Gastrin: Secreted by G-cells in the pyloric region of the stomach, gastrin stimulates the gastric glands to secrete and release gastric juice. It also promotes gastric mobility.
- Enterogastrone (Gastric Inhibitory Peptide – GIP): Produced by the duodenal epithelium, enterogastrone inhibits gastric secretion and motility. It slows down gastric contractions, earning it the name gastric inhibitory peptide.
- Secretin: Discovered as the first hormone, secretin is secreted by the duodenal epithelium. It stimulates the release of bicarbonates in the pancreatic juice and increases bile secretion. Additionally, secretin decreases gastric secretion and motility.
- Cholecystokinin pancreozymin (CCK-PZ): This hormone, secreted by the epithelium of the entire small intestine, stimulates the gall bladder to release bile and the pancreas to secrete digestive enzymes in the pancreatic juice.
- Duocrmin: Secreted by the duodenal epithelium, duocrmin stimulates the Brunner’s glands to release mucus and enzymes into the intestinal juice.
- Enterocrinin: Produced by the epithelium of the entire small intestine, enterocrinin stimulates the crypts of Lieberkuhn to release enzymes into the intestinal juice.
- Vasoactive Intestinal Peptide (VIP): VIP is secreted by the epithelium of the entire small intestine. It dilates peripheral blood vessels in the gut and inhibits gastric acid secretion.
- Villikinin: Secreted by the epithelium of the entire small intestine, villikinin accelerates the movement of villi.
- Somatostatin (SS): Somatostatin, secreted by the Delta cells of the pancreatic islets of Langerhans, inhibits the secretion of glucagon by alpha cells and insulin by beta cells. Additionally, somatostatin produced by argentaffin cells of gastric and intestinal glands suppresses the release of hormones from the digestive tract.
- Pancreatic Polypeptide (PP): Pancreatic polypeptide is secreted by the pancreatic polypeptide cells (also known as PP cells or F-cells) of the islets of Langerhans. It inhibits the release of pancreatic juice from the pancreas.
These gastrointestinal hormones play important roles in regulating various aspects of digestive secretions, including gastric juice, bile, pancreatic enzymes, and mucus production. They ensure the proper functioning of the digestive system and contribute to the overall process of digestion and nutrient absorption.
How Hormones Work
Hormones exert their effects on target cells by following specific mechanisms:
- Receptor Specificity: Hormones bind to specific hormone receptors on target cells. Each hormone has a unique chemical structure that allows it to selectively bind to its corresponding receptor. Different cell types may have varying numbers of receptors for a specific hormone, determining their sensitivity to that hormone.
- Cell-Surface Receptors: Some hormones, such as water-soluble peptides and amines, bind to receptors located on the surface of target cells. These receptors are typically coupled to intracellular signaling pathways and trigger a cascade of events upon hormone binding. This can lead to the activation or inhibition of various cellular processes through the generation of second messengers.
- Intracellular Receptors: Other hormones, such as lipid-soluble steroids, can cross the cell membrane and bind to receptors located within the cytoplasm or nucleus of target cells. The hormone-receptor complex enters the nucleus and directly modulates gene transcription. This results in the synthesis of specific proteins that ultimately affect cellular activity.
- Gene Transcription: Hormone-receptor complexes that bind to intracellular receptors can act as transcription factors. They bind to specific DNA sequences in the promoter regions of target genes, either promoting or inhibiting gene transcription. The resulting changes in gene expression lead to alterations in cellular activity and the synthesis of proteins necessary for the hormone’s intended effects.
- Modulation of Cellular Processes: Hormone-receptor binding can modulate a wide range of cellular processes. This includes changes in metabolic activity, enzymatic reactions, ion transport, cell growth and proliferation, and secretion of other hormones or signaling molecules.
- Feedback Mechanisms: Hormonal regulation often involves feedback mechanisms to maintain homeostasis. High levels of a particular hormone can trigger down-regulation, where the number of hormone receptors on target cells decreases. This reduces the cell’s sensitivity to the hormone, helping to prevent excessive stimulation. Conversely, low hormone levels can induce up-regulation, increasing the number of hormone receptors on target cells and enhancing cellular sensitivity.
- Integration of Multiple Signals: Target cells often receive signals from multiple hormones, allowing for complex regulation and integration of different physiological processes. Hormones may act in synergy or opposition, coordinating and balancing various cellular activities.
In summary, hormones work by binding to specific receptors on target cells, leading to changes in cellular activity and the regulation of various physiological processes. The specific location of the receptor, as well as the hormone’s chemical structure, determines the mechanism through which the hormone mediates its effects, either by directly influencing gene transcription or by stimulating signaling pathways.
Pathways Involving Intracellular Hormone Receptors
- Intracellular hormone receptors play a crucial role in mediating the effects of lipid-derived (soluble) hormones within target cells. Unlike water-soluble hormones that bind to cell surface receptors, lipid-derived hormones, such as steroid hormones, are able to diffuse across the membranes of endocrine cells. Once outside the cell, these hormones bind to transport proteins that keep them soluble in the bloodstream, facilitating their transport to target cells.
- Upon reaching the target cell, the hormone molecules are released from the carrier proteins and can freely diffuse across the lipid bilayer of the cell’s plasma membrane. This ability to pass through the plasma membrane is a unique characteristic of lipid-derived hormones, as they are able to interact with intracellular receptors.
- Intracellular receptors for lipid-derived hormones can be found in two primary locations within the cell: the cytoplasm or the nucleus. In the cytoplasm, the hormone-receptor complex interacts with receptors residing in this compartment. Alternatively, some receptors are located within the nucleus itself.
- Once the hormone binds to its specific receptor, a complex is formed. This hormone-receptor complex initiates a series of intracellular signaling pathways that ultimately lead to the regulation of gene expression. The complex acts as a transcription regulator, influencing the synthesis of mRNA molecules from specific genes.
- By altering gene expression, the hormone-receptor complex determines the amount of corresponding protein that is synthesized within the cell. This protein may contribute to structural changes in the cell or act as enzymes that catalyze important chemical reactions. Ultimately, the regulation of specific cell processes is achieved through the modulation of gene expression by the hormone-receptor complex.
- While steroid hormones are a well-known example of lipid-derived hormones that utilize intracellular receptors, other lipid-soluble hormones like vitamin D and thyroxine also follow a similar mechanism. These hormones, despite not being steroids, are able to diffuse across both the plasma membrane and the nuclear envelope. They subsequently bind to receptors located in the nucleus, where the hormone-receptor complex stimulates the transcription of specific genes.
- In summary, intracellular hormone receptors play a vital role in mediating the effects of lipid-derived hormones. By binding to these receptors, hormone molecules initiate intracellular signaling pathways that regulate gene expression, leading to the synthesis of specific proteins and influencing various cellular processes. This mechanism allows for precise and targeted regulation of cellular function in response to lipid-derived hormones.
Pathways Involving Cell Membrane Hormone Receptors
- Plasma membrane hormone receptors are essential for mediating the effects of amino acid-derived hormones and polypeptide hormones, which are not lipid-derived and therefore cannot diffuse through the plasma membrane of cells.
- Unlike lipid-derived hormones such as steroid hormones, which act through intracellular receptors, lipid-insoluble hormones bind to receptors located on the outer surface of the plasma membrane. These receptors are known as plasma membrane hormone receptors. When a hormone binds to its specific receptor, it initiates a signaling pathway that triggers intracellular activity and leads to the specific effects associated with the hormone.
- In this mechanism, the hormone does not enter the target cell but instead remains bound to the cell surface receptor. Similarly, the intracellular products resulting from the signaling pathway remain inside the cell. The hormone that initiates the signaling pathway is referred to as the first messenger, while the intracellular molecules involved in the signaling cascade are known as second messengers.
- One example of amino acid-derived hormones is epinephrine and norepinephrine, which bind to beta-adrenergic receptors on the plasma membrane of cells. Binding of these hormones to the receptor activates a G-protein associated with the receptor. The G-protein, when activated, stimulates the activity of an enzyme called adenylyl cyclase. Adenylyl cyclase converts ATP to cyclic AMP (cAMP), which serves as a second messenger.
- cAMP then activates a group of proteins known as protein kinases. These protein kinases catalyze phosphorylation, which involves transferring a phosphate group from ATP to a substrate molecule. Phosphorylation leads to changes in the structural orientation and activation of the substrate molecule. These activated molecules can then mediate changes in cellular processes.
- The signaling pathway initiated by hormone-receptor binding results in an amplification of the hormonal effect. The binding of a single hormone molecule to a receptor leads to the activation of multiple G-proteins, which subsequently activate adenylyl cyclase. Each molecule of adenylyl cyclase generates numerous molecules of cAMP. Additionally, protein kinases, once activated by cAMP, can catalyze multiple reactions. This amplification process allows a small amount of hormone to trigger the formation of a significant amount of cellular product.
- To regulate hormone activity and prevent overproduction of cellular products, cAMP is deactivated by an enzyme called phosphodiesterase (PDE), which is present in the cytoplasm. PDE breaks down cAMP, terminating the signaling cascade.
- The specific response of a cell to a lipid-insoluble hormone depends on the types of receptors present on the cell membrane and the substrate molecules within the cytoplasm. Cellular responses to hormone-receptor binding include alterations in membrane permeability and metabolic pathways, stimulation of protein and enzyme synthesis, and activation of hormone release.
- In summary, plasma membrane hormone receptors play a vital role in mediating the effects of lipid-insoluble hormones. Through the activation of signaling pathways and the involvement of second messengers, these receptors initiate intracellular activity and regulate various cellular processes in response to hormone binding.
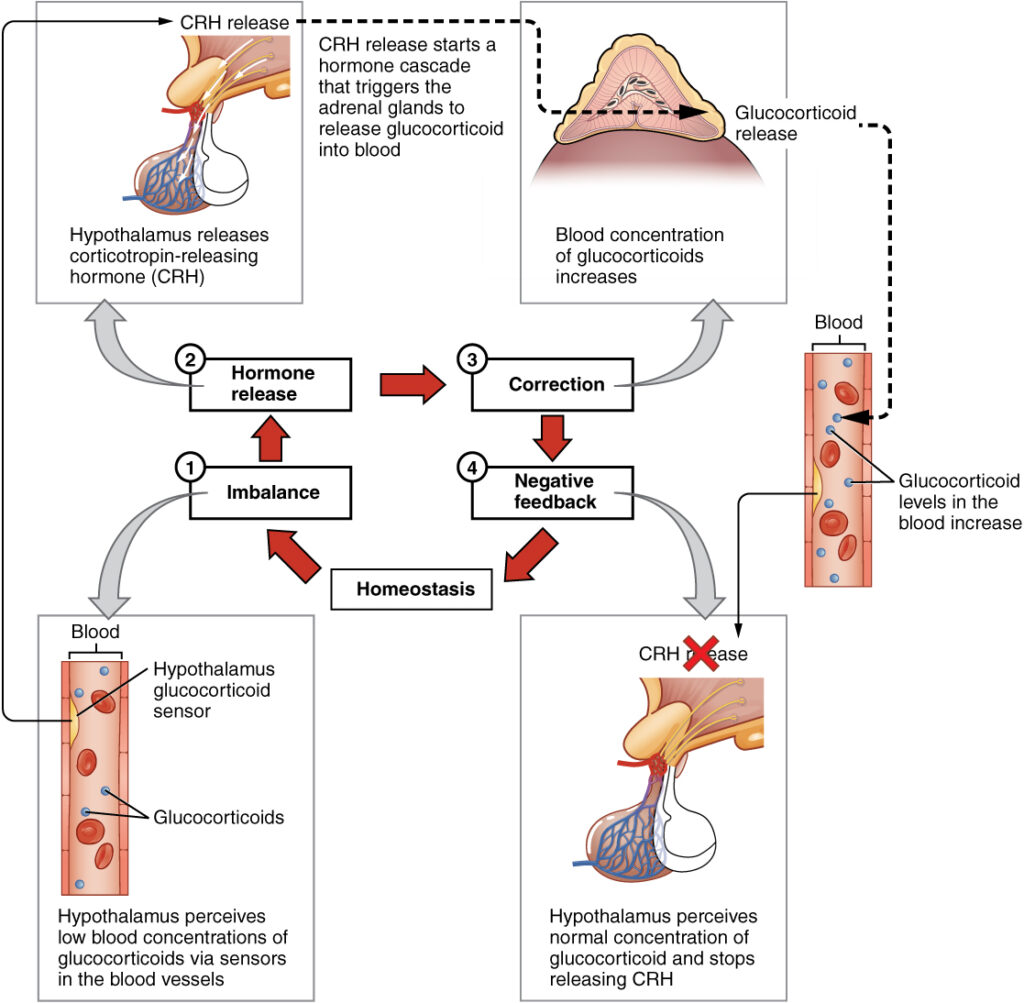
Regulation of Hormone Production
- The regulation of hormone production and release is primarily governed by a mechanism known as negative feedback. Negative feedback systems operate by maintaining hormone concentrations within a specific range. When the concentration of a particular hormone reaches a certain level, it triggers a signal that inhibits further production and release of that hormone.
- In negative feedback, a stimulus initiates the release of a substance, such as a hormone. As the concentration of the hormone increases, it reaches a threshold level that signals the body to cease further secretion. This process ensures that the hormone levels remain within a narrow and optimal range, thereby maintaining homeostasis.
- One example of negative feedback regulation is observed in the control of insulin and glucagon secretion in response to blood glucose levels. When blood glucose levels rise, it stimulates the release of insulin from pancreatic beta cells. Insulin helps to lower blood glucose by promoting its uptake into cells and inhibiting the release of glucose from the liver. As blood glucose levels decrease due to the actions of insulin, it eventually reaches a point where it signals the body to halt further insulin secretion. On the other hand, when blood glucose levels drop, it triggers the release of glucagon from pancreatic alpha cells, which stimulates the liver to release stored glucose into the bloodstream. As blood glucose levels rise, glucagon secretion is inhibited through negative feedback.
- The regulation of hormone production involves direct secretion by endocrine glands or indirect control through the hypothalamus, a region of the brain that influences other endocrine glands to release hormones. The hormones released then act on target cells, initiating physiological changes that restore homeostasis. Once normal conditions have been restored, the production of hormones is discontinued or reduced as a result of negative feedback. In other words, the corrective actions triggered by hormone production are diminished or ceased when the initial abnormal condition has been rectified.
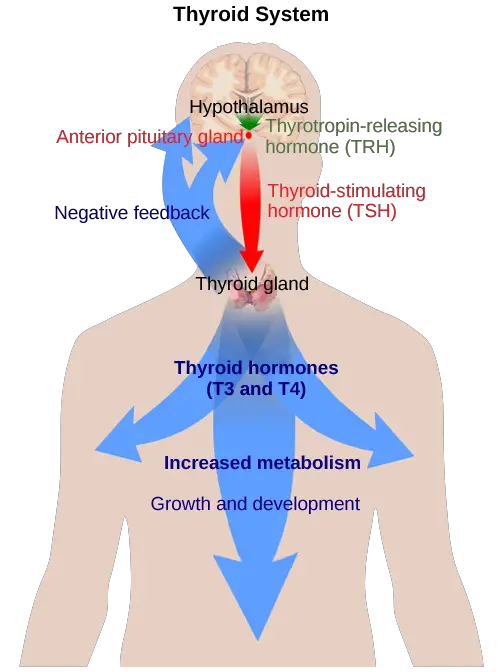
- Another example of hormone regulation through negative feedback occurs in the interaction between the hypothalamus, anterior pituitary gland, and the thyroid gland. The hypothalamus releases a hormone called thyrotropin-releasing hormone (TRH), which signals the anterior pituitary gland to release thyroid-stimulating hormone (TSH). TSH, in turn, stimulates the thyroid gland to produce and release thyroid hormones (T3 and T4). As the levels of thyroid hormones in the blood increase, they provide negative feedback to the hypothalamus and anterior pituitary, inhibiting further release of TRH and TSH. This negative feedback loop helps maintain appropriate levels of thyroid hormones in the body.
In summary, the regulation of hormone production and release is primarily governed by negative feedback mechanisms. This feedback system ensures that hormone concentrations are maintained within a narrow range, contributing to the maintenance of homeostasis in the body. Hormone secretion is initiated in response to stimuli, but once the desired conditions are restored, the feedback mechanism halts further production, maintaining balance and stability.
Role of Feedback Loops
- Feedback loops play a crucial role in maintaining homeostasis, which is the body’s ability to regulate its internal environment. There are two types of feedback loops: positive feedback and negative feedback.
- Positive feedback loops involve the release of additional hormone in response to the initial release of a hormone. An example of a positive feedback loop is the release of oxytocin during childbirth. When oxytocin is initially released, it signals the uterine muscles to contract, pushing the fetus toward the cervix and causing it to stretch. This stretching, in turn, stimulates the pituitary gland to release more oxytocin, which intensifies the labor contractions. Once the childbirth is complete, the release of oxytocin decreases, and the positive feedback loop is interrupted.
- On the other hand, the more common method of hormone regulation is through negative feedback loops. Negative feedback is characterized by the inhibition of further hormone secretion when adequate levels of that hormone are reached. This mechanism helps to maintain hormone levels within a narrow range in the bloodstream. For example, the release of glucocorticoid hormones from the adrenal glands is regulated by negative feedback. The hypothalamus and pituitary gland direct the release of glucocorticoids. As the concentration of glucocorticoids in the blood rises, the hypothalamus and pituitary gland reduce their signaling to the adrenal glands, preventing additional secretion of glucocorticoids. This negative feedback loop helps to keep the glucocorticoid levels in check and prevent them from becoming excessively high.
- In summary, feedback loops play a critical role in hormone regulation and homeostasis. Positive feedback loops amplify the effects of a hormone, while negative feedback loops help to maintain hormone levels within a balanced range. These mechanisms ensure that the body’s hormone levels and physiological processes are appropriately regulated and functioning optimally.
Role of Endocrine Gland Stimuli
Stimuli play a crucial role in triggering the synthesis and release of hormones from endocrine glands. There are three main mechanisms by which these glands are stimulated: humoral stimuli, hormonal stimuli, and neural stimuli.
- Humoral stimuli refer to the control of hormone release in response to changes in extracellular fluids, such as blood or ion concentrations. The term “humoral” derives from “humor,” which pertains to bodily fluids. For example, when blood glucose levels rise, the pancreas releases insulin to lower blood glucose levels. As insulin decreases blood glucose levels, it signals the pancreas to cease insulin production through a negative feedback loop.
- Hormonal stimuli involve the release of a hormone in response to another hormone. Several endocrine glands release hormones when stimulated by hormones released by other endocrine glands. For instance, the hypothalamus produces hormones that stimulate the anterior pituitary gland. In turn, the anterior pituitary gland releases hormones that regulate hormone production by other endocrine glands. An example of hormonal stimuli is the release of thyroid-stimulating hormone (TSH) by the anterior pituitary, which stimulates the thyroid gland to produce T3 and T4 hormones. As blood concentrations of T3 and T4 increase, they inhibit both the pituitary and the hypothalamus through a negative feedback loop.
- Neural stimuli occur when the nervous system directly stimulates endocrine glands to release hormones. This mechanism is known as neural stimuli. In certain situations, the sympathetic nervous system can directly stimulate the adrenal medulla to release hormones such as epinephrine and norepinephrine. These hormones play a crucial role in providing bursts of energy required for the body’s response to short-term stress. The neuronal signaling from the sympathetic nervous system triggers the release of epinephrine and norepinephrine in response to stress.
In summary, stimuli, including humoral, hormonal, and neural stimuli, play a pivotal role in regulating hormone synthesis and release. These mechanisms ensure that the body can respond appropriately to various internal and external factors, maintaining homeostasis and coordinating physiological processes.
Functions of Hormone
Hormones serve various functions in organisms, including:
- Regulation of Growth and Development: Hormones play a crucial role in controlling the growth and development of organisms. They influence processes such as cell division, cell differentiation, and tissue formation, ensuring proper growth and maturation.
- Metabolic Regulation: Hormones regulate metabolism by controlling the breakdown, synthesis, and utilization of nutrients. They influence energy balance, nutrient absorption, and the release of stored energy sources like glucose and fatty acids.
- Reproduction and Sexual Development: Hormones are involved in reproductive processes, including the development of primary and secondary sexual characteristics, regulation of the menstrual cycle, sperm production, ovulation, fertilization, and pregnancy.
- Homeostasis and Internal Balance: Hormones contribute to maintaining internal balance and homeostasis in the body. They regulate body temperature, fluid and electrolyte balance, blood pressure, and pH levels to ensure optimal physiological functioning.
- Behavior and Emotions: Hormones influence behavior, mood, and emotions. They can modulate processes such as stress responses, aggression, sexual behavior, sleep-wake cycles, appetite, and social interactions.
- Regulation of Metabolic Disorders: Hormones play a critical role in preventing and managing metabolic disorders such as diabetes and obesity. Hormones like insulin regulate blood sugar levels, while others control appetite, satiety, and fat metabolism.
- Immune Response and Inflammation: Certain hormones regulate immune responses and inflammation. They help modulate the body’s immune system, promote the production of immune cells, and regulate the inflammatory process.
- Calcium and Bone Metabolism: Hormones like parathyroid hormone and calcitonin regulate calcium levels in the blood and bone metabolism. They ensure the maintenance of appropriate calcium levels for various physiological processes, including muscle function and bone health.
- Stress Response: Hormones are involved in the body’s response to stress. Hormones like cortisol, adrenaline, and noradrenaline are released during stress and help prepare the body for the fight-or-flight response.
- Circadian Rhythms: Hormones play a role in regulating circadian rhythms, which are the body’s internal biological rhythms. Hormones like melatonin help regulate sleep-wake cycles and other physiological processes that follow a daily rhythm.
These are just a few examples of the diverse functions of hormones in organisms. Hormones act as chemical messengers that coordinate and regulate numerous physiological processes to maintain overall health and proper functioning.
What is Endocrinologist?
- An endocrinologist is a medical doctor who specializes in diagnosing and treating disorders related to the endocrine glands, hormone systems, and metabolic pathways involving glucose and lipids. They play a crucial role in managing various endocrine diseases and conditions. Endocrinologists may work closely with endocrine surgeons, who specialize in surgical interventions for endocrine disorders and diseases.
- The scope of an endocrinologist’s practice includes managing diseases such as diabetes mellitus (disorders of the pancreas), gigantism, acromegaly, and pituitary dwarfism (disorders of the pituitary gland), goiter and Graves’ disease (disorders of the thyroid gland), and Cushing’s disease and Addison’s disease (disorders of the adrenal glands). These specialists possess in-depth knowledge and expertise in the complex interplay of hormones and their effects on the body.
- To diagnose endocrine disorders, endocrinologists rely on extensive laboratory tests. They use various tests that stimulate or suppress the functioning of endocrine organs to assess hormone production. Blood samples are collected before and after these tests to evaluate the hormonal response. For example, in the diagnosis of diabetes mellitus, patients may undergo a fasting period followed by a sugary drink to stimulate the pancreas to produce insulin and regulate blood glucose levels. Blood samples are taken after the drink to assess the pancreas’ functionality. The A1C test is another example, which measures average blood glucose levels over several months, providing insights into long-term glucose management.
- Once a disease is diagnosed, endocrinologists develop treatment plans tailored to each patient’s needs. They may recommend lifestyle modifications, including exercise, weight loss, and dietary changes for managing conditions like diabetes mellitus. In some cases, medication may be prescribed to enhance insulin release or regulate hormone levels. For patients who cannot effectively manage their conditions through lifestyle changes and medications, endocrinologists may recommend insulin injections or other advanced treatment options.
- Apart from clinical practice, endocrinologists often engage in primary research and development activities. They contribute to ongoing studies and trials aimed at advancing the understanding and treatment of endocrine disorders. For example, research on islet cell transplantation investigates the potential of transplanting healthy pancreatic islet cells into diabetic patients, with the goal of eliminating the need for insulin injections.
In summary, endocrinologists are specialized medical professionals who diagnose and treat disorders of the endocrine glands, hormone systems, and metabolic pathways. Their expertise in hormonal regulation and extensive use of laboratory tests allow them to provide comprehensive care for patients with various endocrine diseases, ensuring optimal management and improved quality of life.
Why are Hormones called Chemical Messengers?
Hormones are referred to as chemical messengers because they play a crucial role in transmitting signals and information throughout the body. The hypothalamus, located in the forebrain, contains specialized cells called neurosecretory cells that produce a hormone known as neurohormones. These neurohormones stimulate the anterior lobe of the pituitary gland to secrete various other hormones.
The primary function of hormones is to act as messengers, relaying important signals and instructions to target cells and organs. When hormones are released into the bloodstream, they travel to their target tissues where they bind to specific receptors. This binding initiates a series of biochemical reactions and signaling pathways within the target cells, ultimately leading to specific physiological responses.
Hormones not only act as messengers but also serve as regulators of the body’s internal environment. They help maintain homeostasis, which is the balance and stability of various physiological processes. Changes in hormone production can lead to specific changes in the body, ensuring that the appropriate responses are triggered to maintain equilibrium.
To regulate hormone production, feedback control mechanisms come into play. These mechanisms monitor the levels of hormones in the body and adjust their production accordingly. Feedback control can be either positive or negative. In negative feedback, the response aims to counteract the initial stimulus, bringing the hormone levels back to a normal range. Positive feedback, on the other hand, amplifies the initial stimulus, causing an increase in hormone production until a specific response is achieved.
In summary, hormones are called chemical messengers because they transmit signals and information throughout the body. They act as regulators, maintaining homeostasis, and their production is controlled by feedback mechanisms. Hormones play a crucial role in coordinating and modulating various physiological processes, ensuring the proper functioning of the body.
Feedback Mechanism – Thyroid
- The thyroid gland plays a crucial role in maintaining thyroid hormone levels through a feedback mechanism. Thyroxine, a hormone produced by the thyroid gland, is regulated by the Thyrotropin Releasing Hormone (TRH) from the hypothalamus and the Thyroid Stimulating Hormone (TSH) from the anterior pituitary.
- In a feedback mechanism, when the level of thyroxine in the blood decreases, the hypothalamus responds by releasing TRH, which stimulates the secretion of TSH from the anterior pituitary. TSH, in turn, stimulates the thyroid gland to produce and release more thyroxine. This positive feedback mechanism ensures that thyroxine levels are increased when they are too low.
- However, if the hypothalamus continues to stimulate thyroxine production without appropriate regulation, it can lead to excessive thyroxine levels in the blood, a condition known as hyperthyroidism. In response to high thyroxine levels, negative feedback occurs. The elevated thyroxine levels signal the hypothalamus to reduce or stop the secretion of TRH and the anterior pituitary to decrease TSH secretion. This negative feedback mechanism helps regulate and maintain the appropriate levels of thyroxine in the body.
- Once hormones have carried out their functions in target tissues, they need to be removed from circulation. The liver, kidney, and other organs play a significant role in removing hormones from the bloodstream. These organs metabolize and eliminate hormones from the body, ensuring that hormone levels remain balanced.
- In summary, the thyroid gland and its hormone, thyroxine, are regulated by a feedback mechanism. Low thyroxine levels stimulate the hypothalamus and anterior pituitary to increase hormone production through positive feedback. However, excessive thyroxine levels trigger negative feedback, reducing the secretion of TRH and TSH to maintain balance. Hormones are efficiently removed from the bloodstream by organs like the liver and kidney once their function is fulfilled.
List of Female Hormones
Here is a list of some of the key hormones involved in the female reproductive system:
- Estrogen: Estrogen refers to a group of hormones, including estradiol, estrone, and estriol. These hormones are primarily produced by the ovaries and play a crucial role in the development and maintenance of female reproductive structures, regulation of the menstrual cycle, and the development of secondary sexual characteristics.
- Progesterone: Progesterone is produced by the ovaries, specifically the corpus luteum during the menstrual cycle and the placenta during pregnancy. It helps prepare the uterus for implantation of a fertilized egg and supports the growth and development of the embryo and fetus.
- Follicle-stimulating hormone (FSH): FSH is produced by the pituitary gland and is responsible for stimulating the growth and development of ovarian follicles, which contain the eggs.
- Luteinizing hormone (LH): LH is also produced by the pituitary gland and works in conjunction with FSH to regulate the menstrual cycle. It triggers ovulation, the release of a mature egg from the ovary.
- Prolactin: Prolactin is primarily known for its role in stimulating milk production in the breasts after childbirth. It is also involved in regulating the menstrual cycle and supporting reproductive function.
- Gonadotropin-releasing hormone (GnRH): GnRH is produced by the hypothalamus and plays a vital role in regulating the release of FSH and LH from the pituitary gland.
- Human chorionic gonadotropin (hCG): hCG is a hormone produced by the placenta during pregnancy. It helps maintain the corpus luteum, which in turn produces progesterone to support the pregnancy.
These are just a few examples of the hormones involved in the female reproductive system. Hormones work together in a complex interplay to regulate menstrual cycles, ovulation, pregnancy, and other aspects of female physiology.
List of Male Hormones
Here is a list of some of the key hormones involved in the male reproductive system:
- Testosterone: Testosterone is the primary male sex hormone. It is produced by the testes and plays a crucial role in the development and maintenance of male reproductive tissues, including the testes, prostate gland, and seminal vesicles. Testosterone is responsible for the development of secondary sexual characteristics in males, such as facial hair, deepening of the voice, and muscle mass.
- Follicle-stimulating hormone (FSH): FSH is produced by the pituitary gland and plays a role in male reproduction by stimulating the production of sperm in the testes.
- Luteinizing hormone (LH): LH, also produced by the pituitary gland, works in conjunction with FSH to regulate male reproductive function. It stimulates the production of testosterone in the testes and promotes the release of mature sperm cells.
- Gonadotropin-releasing hormone (GnRH): GnRH is produced by the hypothalamus and plays a vital role in regulating the release of FSH and LH from the pituitary gland.
- Prolactin: While prolactin is predominantly known for its role in milk production in females, it also has some effects in males. Prolactin can influence testosterone levels and may have an impact on reproductive function in males.
- Dihydrotestosterone (DHT): DHT is a derivative of testosterone and is a potent androgen. It plays a role in the development of male sex organs during fetal development and is involved in the maintenance of male secondary sexual characteristics.
These are some of the key hormones involved in male reproductive function. Hormonal regulation is crucial for the development and functioning of male reproductive organs, sperm production, sexual characteristics, and overall reproductive health.
Therapeutic use of Hormones
| Hormone | Therapeutic Use |
|---|---|
| Estrogens | Hormonal contraception, hormone replacement therapy (HRT) |
| Progestogens | Hormonal contraception, hormone replacement therapy (HRT) |
| Thyroxine | Treatment of hypothyroidism (as levothyroxine) |
| Steroids | Treatment of autoimmune diseases, respiratory disorders |
| Insulin | Treatment of diabetes mellitus |
| Adrenaline | Local preparations in otolaryngology |
| Vitamin D | Topical creams for dermatological conditions |
| Glucocorticoids | Suppression of inflammation at pharmacologic doses |
Differences Between neurotransmitters and Hormones
| Aspect | Neurotransmitters | Hormones |
|---|---|---|
| Spatial and Temporal Scale | Acts in micrometer-scale distances | Functions over a larger spatial and temporal scale |
| Travel Range | Restricted to pre-existing nerve tracts | Can travel virtually anywhere in the circulatory system |
| Speed of Transmission | Rapid transmission (milliseconds) | Slower transmission (seconds, minutes, or hours) |
| Signal Type | All-or-nothing (digital) action | Continuously variable action dependent on hormone concentration |
| Production | Produced by neurons | Produced by endocrine glands |
| Communication Pathway | Neural pathways | Endocrine pathways |
| Combination | Neurohormones share similarities with neurotransmitters | Classic hormones and neurohormones are the result of a combination between endocrine and neural reflexes |
| Release Mechanism | Released at synapses | Released into the bloodstream |
| Target | Act on adjacent neurons or specific cells | Act on target cells throughout the body |
Examples of Important Hormones with their Functions and Source
- Insulin:
- Function: Regulates blood glucose levels by facilitating the uptake of glucose from the bloodstream into cells, thereby lowering blood sugar levels.
- Source: Pancreas (specifically, beta cells in the islets of Langerhans).
- Estrogen:
- Function: Plays a key role in female sexual development and reproductive function, including regulation of the menstrual cycle, development of secondary sexual characteristics, and maintenance of pregnancy.
- Source: Ovaries (primarily), as well as the placenta during pregnancy.
- Testosterone:
- Function: Regulates male sexual development and reproductive function, including sperm production, development of secondary sexual characteristics (such as facial hair and muscle mass), and libido.
- Source: Testes (specifically, Leydig cells in the testes), as well as the adrenal glands in both males and females.
- Thyroid hormone (T3 and T4):
- Function: Controls the body’s metabolism, regulates growth and development, and helps maintain body temperature.
- Source: Thyroid gland.
- Growth hormone:
- Function: Stimulates growth and development in children, as well as regulates metabolism and body composition in adults.
- Source: Pituitary gland (specifically, the anterior pituitary).
- Cortisol:
- Function: Helps the body respond to stress, regulates metabolism, reduces inflammation, and plays a role in the sleep-wake cycle.
- Source: Adrenal glands (specifically, the adrenal cortex).
- Melatonin:
- Function: Regulates the sleep-wake cycle (circadian rhythm) and plays a role in maintaining the body’s internal clock.
- Source: Pineal gland (specifically, the pinealocytes).
- Parathyroid hormone:
- Function: Regulates calcium and phosphate levels in the blood, promoting the release of calcium from bones and increasing calcium absorption in the intestines.
- Source: Parathyroid glands (four small glands located behind the thyroid gland).
FAQ
What is the definition of a hormone?
Hormones are chemical messengers produced by glands in the endocrine system. They are released into the bloodstream and regulate various physiological processes in the body.
What is the structure of hormones?
Hormones can have different structures depending on their classification. They can be proteins, peptides, steroids, or amino acid derivatives.
What are the main types of hormones?
The main types of hormones are protein/peptide hormones (e.g., insulin), steroid hormones (e.g., estrogen), and amino acid derivative hormones (e.g., adrenaline).
What are the functions of hormones?
Hormones have diverse functions, including regulation of growth and development, metabolism, reproduction, mood, and stress response. They help maintain homeostasis and coordinate various body processes.
How do hormones work in the body?
Hormones bind to specific receptors on target cells or organs. This binding triggers a series of cellular responses that influence gene expression, enzyme activity, or other signaling pathways, resulting in physiological effects.
What are some examples of hormones?
Examples of hormones include insulin, estrogen, testosterone, cortisol, adrenaline, growth hormone, thyroid hormone, progesterone, and melatonin.
How are hormones regulated in the body?
Hormone production and release are regulated through complex feedback mechanisms. Negative feedback loops involve the hormone inhibiting its own production, maintaining hormone levels within a certain range.
Can hormone imbalances occur?
Yes, hormone imbalances can occur due to various factors such as diseases, hormonal disorders, stress, medications, or aging. Imbalances can lead to various health issues and may require medical intervention.
Can hormones be used as medications?
Yes, hormones can be used therapeutically to supplement or replace naturally occurring hormones. Examples include hormone replacement therapy (HRT) for menopause, insulin therapy for diabetes, and corticosteroids for inflammatory conditions.
How are hormone levels tested?
Hormone levels can be tested through blood, urine, or saliva tests. These tests can help diagnose hormonal disorders, monitor treatment efficacy, or assess fertility and reproductive health.
References
- https://opentextbc.ca/biology/chapter/18-1-types-of-hormones/
- https://dhingcollegeonline.co.in/attendence/classnotes/files/1603564542.pdf
- https://pcsstudies.com/chemical-classification-of-hormones/
- https://www.pharmaguideline.com/2021/11/classification-of-hormones-mechanism-of-hormone-action.html
- https://myendoconsult.com/learn/classification-of-hormones/
- https://courses.lumenlearning.com/suny-ap2/chapter/hormones/
- https://www.onlinebiologynotes.com/hormones-properties-functions-and-classification/
- https://www.biologydiscussion.com/hormones/classification-hormones/classification-of-hormones-5-categories/18429
- https://pressbooks-dev.oer.hawaii.edu/biology/chapter/types-of-hormones/
- http://www.rajasinghcollegesiwan.com/Zoology/Classification%20of%20hormones.pdf
- https://collegedunia.com/exams/hormones-in-animals-biology-articleid-1368


