Table of Contents
What is Thymus Gland?
- The thymus gland is a vital part of the lymphatic system, located in the mediastinum beneath the sternum. It extends from the fourth intercostal gap of the vertebrae to the lower margin of the thyroid gland. Unlike other endocrine glands, the thymus gland is primarily active before puberty. During puberty, it reaches its maximum size and then gradually undergoes replacement by adipose tissue.
- The thymus gland plays a critical role in the immune system, acting as a defense mechanism against diseases, cancers, and antigens. It is particularly important for the adaptive or thymus-dependent arm of the immune system, as it is responsible for the growth and activation of immune cells.
- Within the thymus, various immune cells are present, including macrophages, neutrophils, dendritic cells, and secretory cells. The growth of secretory cells and the regulation of their secretions are sustained by cytokines such as tumor necrosis factor (TNF) and interferon.
- It is worth noting that autoimmune conditions like myasthenia gravis can affect the anatomy and function of the thymus gland.
- The thymus gland is a lymphocyte-rich, bilobed, encapsulated organ situated behind the sternum, above and in front of the heart. Its activity is highest during fetal development and early childhood, after which it undergoes atrophy at puberty. However, it never completely disappears.
- During embryonic life, the thymus develops from the third and fourth pharyngeal pouches. It attracts circulating T cell precursors derived from hematopoietic stem cells in the bone marrow through chemoattractive molecules. The thymus serves as a primary lymphoid organ, essential for the maturation of T cells and the development of cell-mediated immunity. In fact, the term “T cell” refers to thymus-derived cells and is used to describe mature T cells.
- The thymus gland is composed of cortical and medullary epithelial cells, stromal cells, interdigitating cells, and macrophages. These cells play a crucial role in the differentiation of migrating T cell precursors and their “education” through positive and negative selection before they migrate into secondary lymphoid tissues.
Definition of Thymus Gland
The thymus gland is an important organ of the lymphatic system located in the chest behind the breastbone. It plays a crucial role in the development and maturation of immune cells known as T cells, which are essential for the body’s immune response. The thymus gland is most active during childhood and gradually diminishes in size and function after puberty.
Characterisitcs of Thymus Gland
The thymus gland is a unique organ with distinct characteristics. Here are the key characteristics of the thymus gland:
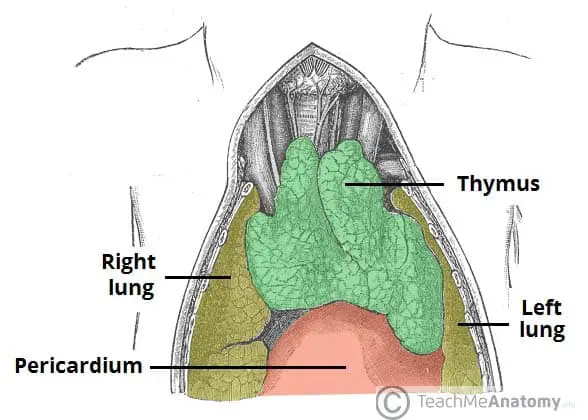
- Location: The thymus gland is located in the upper chest, behind the sternum (breastbone), in front of the heart, and above the superior vena cava. It is part of the mediastinum, which is the central region of the chest cavity.
- Structure: The thymus gland has a lobular structure, consisting of two lobes connected by a central portion called the isthmus. Each lobe is further divided into smaller lobules. It is composed of both glandular tissue and lymphoid tissue.
- Function: The primary function of the thymus gland is the maturation and development of T cells, which are a type of white blood cell involved in cell-mediated immunity. The thymus provides a microenvironment where T cells differentiate, mature, and acquire their immunological functions.
- Maturation Site: The thymus is the primary site for T cell maturation. Immature T cells, known as thymocytes, migrate from the bone marrow to the thymus. Within the thymus, they undergo a process of maturation, selection, and education to become functional T cells capable of recognizing foreign antigens and distinguishing them from self-antigens.
- Hormonal Influence: The thymus gland produces various hormones that play a role in T cell development and maturation. These hormones include thymosin, thymopoietin, and thymulin, among others. They help regulate the differentiation and function of thymocytes.
- Size and Involution: The size of the thymus gland changes throughout life. It is relatively large in infants and children, reaching its maximum size during puberty. However, with age, the thymus undergoes a process called involution, where it gradually decreases in size and becomes replaced by fatty tissue. This involution is a natural part of aging.
- Immune-Endocrine Interaction: The thymus gland serves as an interface between the immune and endocrine systems. It functions as both a lymphoid organ and an endocrine gland. It interacts with other components of the immune system, such as lymph nodes and spleen, as well as secretes hormones that influence T cell development and immune responses.
- Role in Autoimmunity: The thymus gland plays a crucial role in preventing autoimmune diseases. Through processes like positive and negative selection, the thymus eliminates T cells that could potentially attack the body’s own tissues, promoting self-tolerance and preventing autoimmune responses.
These characteristics make the thymus gland a vital organ for the development and regulation of the immune system, particularly in the maturation of T cells and the establishment of immune tolerance.
Structure of Thymus Gland
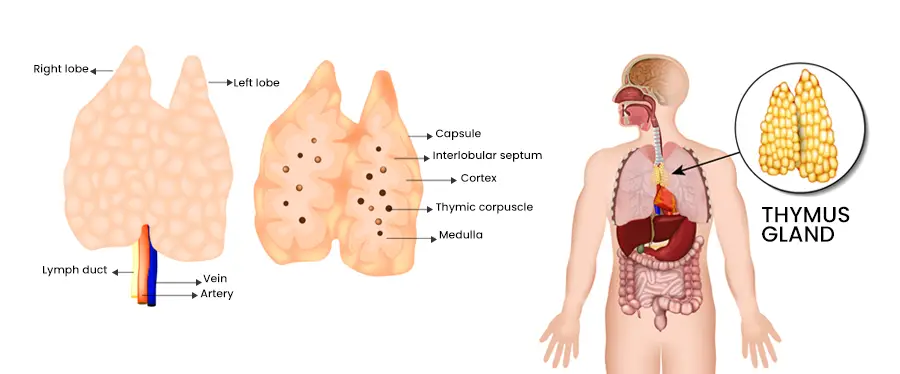
- The thymus gland has a distinctive structure consisting of two pyramid-shaped lobes. Each lobe has a lobulated surface and is divided by an interior connective tissue septum and a thick connective tissue capsule. The majority of the gland’s mass is composed of an intricate network of star-shaped reticular cells.
- The epithelial cells of the thymus gland are classified into four main subtypes based on various characteristics, including antigenic expression, ultrastructure, and hormone production. These subtypes are subcapsular cortical, inner cortical, medullary, and Hassall’s corpuscles.
- The outer cortex of the thymus gland contains loosely packed lymphocytes, while the medulla contains reticulocytes with abundant cytoplasm. Additionally, there are small structures called Hassall’s concentric corpuscles or thymic corpuscles, which consist of concentric arrays of squamous cells.
- In infants and young children, the thymus gland is relatively large and reaches its maximum size during puberty. However, after puberty, the gland gradually undergoes consolidation and is gradually replaced by adipose tissue.
- The blood supply to the thymus gland is provided by the inferior thyroid artery, internal thoracic artery, and intercostal arteries. The gland is connected to the sternum through bilateral muscles known as the sternohyoid and sternothyroid muscles.
Anatomy of Thymus Gland
The thymus gland is anatomically situated at the top of the sternum, near the collarbone, between the sternum and the aortic arch. At birth, it is approximately 1 to 2 inches wide and half an inch thick. Throughout childhood, the thymus gradually grows in size until it starts to shrink during adolescence.
Encased within a collagen-type tissue wall, the thymus gland is divided into two main lobes consisting of irregular lobules or sub-lobes. Each lobe contains several structures and cell types:
- Cortex: The cortex is located nearest to the organ’s wall and is responsible for housing developing T cell lymphocytes.
- Medulla: Positioned near the center of each lobule, the medulla contains fully developed T cells.
- Epithelioreticular cells: These cells form walls within the thymus, creating a lattice-like framework that separates the organ into distinct sections for developing and mature T cells.
- Blood vessels: The capsule and walls of the lobules contain blood vessels that supply oxygen to the tissues of the thymus.
- Lymphatic vessels: Similar to blood vessels, lymphatic vessels carry lymphatic fluid throughout the body’s lymphatic system, including the thymus.
- Macrophages: These immune system cells are responsible for eliminating T cells that have not properly developed.
The anatomy of the thymus gland can exhibit variations, particularly in infants, where it may extend above the clavicle. Some infants may have an enlarged thymus that exerts pressure on structures like the trachea or heart. However, it is not always advisable to remove the thymus in such cases, as it could negatively impact the development of the immune system.
Location of Thymus Gland
- The thymus gland is situated in the anterior (front) part of the chest, specifically behind the breastbone or sternum and between the lungs. It has a pinkish-grey color and is characterized by its lobed structure, consisting of two primary lobes and smaller lobes branching out from within. The size of the lobes can vary and they may be separate or fused together.
- The thymus gland is a soft, bilobed organ that is encapsulated. It is located near the pericardium in the superior mediastinum (the upper part of the middle compartment of the chest) and the anterior region of the inferior mediastinum (the lower part of the middle compartment of the chest). It lies deep within the sternum and anterior to the major arteries of the heart. It extends upward from the level of the inferior poles of the thyroid gland and reaches the fourth costal cartilage.
- On either side of the thymus gland, running parallel to it, are the phrenic nerves, which continue to supply the diaphragm. The two separate lobes of the thymus are connected in the middle by an isthmus.
- In summary, the thymus gland is located in the front part of the chest behind the sternum, with two lobes that can vary in size and are connected by an isthmus. It is positioned deep within the sternum and anterior to the heart arteries, near the pericardium in the superior and anterior mediastinum.
Blood supply in Thymus Gland
- The blood supply to the thymus gland is provided by several arteries, including branches of the internal thoracic artery, inferior thyroid artery, and occasionally the superior thyroid artery. These arterial branches reach the thymus and travel with the septa of the capsule, entering the space between the cortex and medulla. They either penetrate the thymus itself or directly enter the capsule.
- The veins of the thymus, known as thymic veins, drain into the left brachiocephalic vein, internal thoracic vein, and inferior thyroid veins. In some cases, the veins may directly empty into the superior vena cava.
- Lymphatic vessels in the thymus accompany the arteries and veins but only travel away from the thymus. They drain into various lymph nodes, including the brachiocephalic, tracheobronchial, and parasternal lymph nodes.
- The nerves that supply the thymus originate from the vagus nerve and the cervical sympathetic chain. While branches from the phrenic nerves reach the thymus capsule, they do not penetrate into the thymus itself.
- The internal thoracic artery, along with the superior and inferior thyroid arteries, supplies blood to the thymus. Within the thymus, the blood flow is organized into a series of intricate arcades in the cortex, forming the blood-thymus barrier. This barrier consists of non-fenestrated endothelium, a thick basal lamina, and reticular endothelial cells, along with lymphocytes and macrophages. The structure of the barrier prevents proteins from passing through the thymic capillaries. Subsequently, the blood enters the medullary veins within the thymus.
Development of Thymus Gland
- The development process of the thymus gland involves the differentiation and interaction of thymocytes (immature T cells) and the epithelial cells of the thymus. The epithelium of the thymus develops first as two outgrowths from the third pharyngeal pouch, and sometimes the fourth pharyngeal pouch, extending into the surrounding mesoderm and neural crest-derived mesenchyme. The thymocytes and epithelium meet and join with connective tissue, forming cellular cords and buds of cells. The invading mesoderm surrounds and isolates these buds, resulting in the formation of fine lobules and a sponge-like structure.
- During this developmental stage, hematopoietic bone marrow precursors migrate into the thymus. The proper development of the thymus relies on the interaction between the epithelium and the hematopoietic thymocytes. Iodine is also necessary for thymus development and activity.
- After birth, the thymus continues to grow and reaches its relative maximum size by puberty. It is most active during fetal and neonatal life. By puberty, it weighs around 20 to 50 grams. However, the thymus then begins to decrease in size and activity in a process called thymic involution. After the first year of life, the production of T cells in the thymus starts to decline. Fat and connective tissue gradually occupy a portion of the thymic volume. Thymic involution involves a decrease in size, activity, and the infiltration of fat cells.
- Thymic involution is influenced by factors such as increased levels of sex hormones, which occur during puberty. Chemical or physical castration of adults can cause the thymus to increase in size and activity. Severe illness or human immunodeficiency virus (HIV) infection can also contribute to thymic involution.
- Throughout the aging process, the thymus undergoes further involution, and fat cells progressively infiltrate the gland. In old age, the thymus may be difficult to detect, although it typically weighs between 5 to 15 grams. Thymic involution is a conserved evolutionary process found in most vertebrate species with a thymus.
Histology of Thymus Gland
The histology of the thymus gland reveals distinct regions and cell types that contribute to its function as an organ involved in T cell maturation and selection.
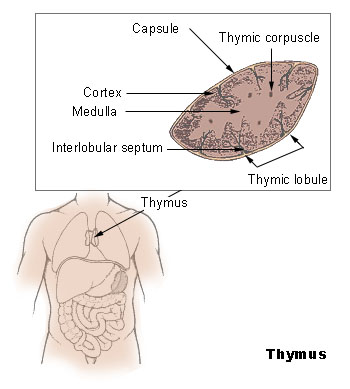
The thymus is enveloped by a connective tissue capsule that sends septa or trabeculae into the tissue, dividing it into incomplete lobules. Each lobule consists of a darker peripheral zone called the cortex and a lighter central zone called the medulla. The capsule’s inner and outer layers are composed of collagen and reticular fibers, between which lymphocytes are located.
- Cortex: The cortex forms the outer region of the thymus gland. It contains numerous tightly packed T lymphocyte progenitors known as thymocytes. Macrophages and epithelial reticular cells are also present in this region. The cortex houses the early stages of thymocyte development and gene rearrangement for T cell receptor surface proteins. It also contains the thymus’ blood arteries, which are associated with the network of epithelial reticular cells.
- Corticomedullary junction: This region represents the transition zone between the cortex and the medulla. It has fewer connective tissues but is rich in blood arteries and mature T lymphocytes. Dendritic cells and B cells can also be found in this area. Type IV epithelial reticular cells are present here as well.
- Medulla: The medulla occupies the central region of the thymus. It consists of a denser network of reticular endothelial cells and a lower number of lymphoid cells compared to the cortex. Hassall’s corpuscles, which are concentrically arranged structures, are a characteristic feature of the medulla. They are composed of flattened epithelial reticular cells packed with keratin filaments and contain a core mass of granular cells. In the medulla, later stages of thymocyte development take place after they have migrated from the cortex. Positive selection, receptor gene rearrangement, and a limited amount of negative selection occur in this region. The medulla is primarily responsible for the majority of negative selection processes.
In summary, the histological examination of the thymus gland reveals a distinct organization with a cortex rich in developing thymocytes and a medulla with Hassall’s corpuscles and mature T lymphocytes. The cortex is involved in early thymocyte growth and gene rearrangement, while the medulla is responsible for later stages of thymocyte maturation and selection processes.
Hormones of Thymus Gland
The thymus gland produces three hormones: thymosin, thymopoietin, and serum thymic factor. These hormones play important roles in immune function and T cell development.
- Thymosin: Thymosin is the primary hormone secreted by the thymus gland. It is produced by the epithelial cells of both the cortex and medulla. Thymosin’s main function is to trigger T cell differentiation and enhance the immunological capabilities of various immune cells. It plays a crucial role in the maturation and development of T cells. Increased levels of thymosin have been associated with changes in phenotypic markers in lymphocytes. Thymosin is a protein that is resistant to heat, capable of withstanding temperatures up to 80°C. It may also contain small amounts of sugar.
- Thymopoietin: Thymopoietin is another hormone produced by the thymus gland. It is a polypeptide hormone that serves more neuromuscular functions rather than immunological ones. However, increased levels of thymopoietin can also cause T cell activation and differentiation. Its precise role in T cell development and immune function is not fully understood.
Serum thymic factor is the third hormone produced by the thymus gland. Its exact function and mechanism of action are still being studied, and it is not as well-characterized as thymosin and thymopoietin. Serum thymic factor is believed to play a role in immune regulation, but further research is needed to fully understand its functions.
Overall, these thymic hormones, particularly thymosin, play crucial roles in T cell development, differentiation, and immunological function. They interact with adenylyl cyclase and bind to specific cell receptors to exert their effects at the cellular level. The thymus gland’s hormonal activity is essential for the maturation and proper functioning of the immune system.
T cell maturation by Thymus Gland
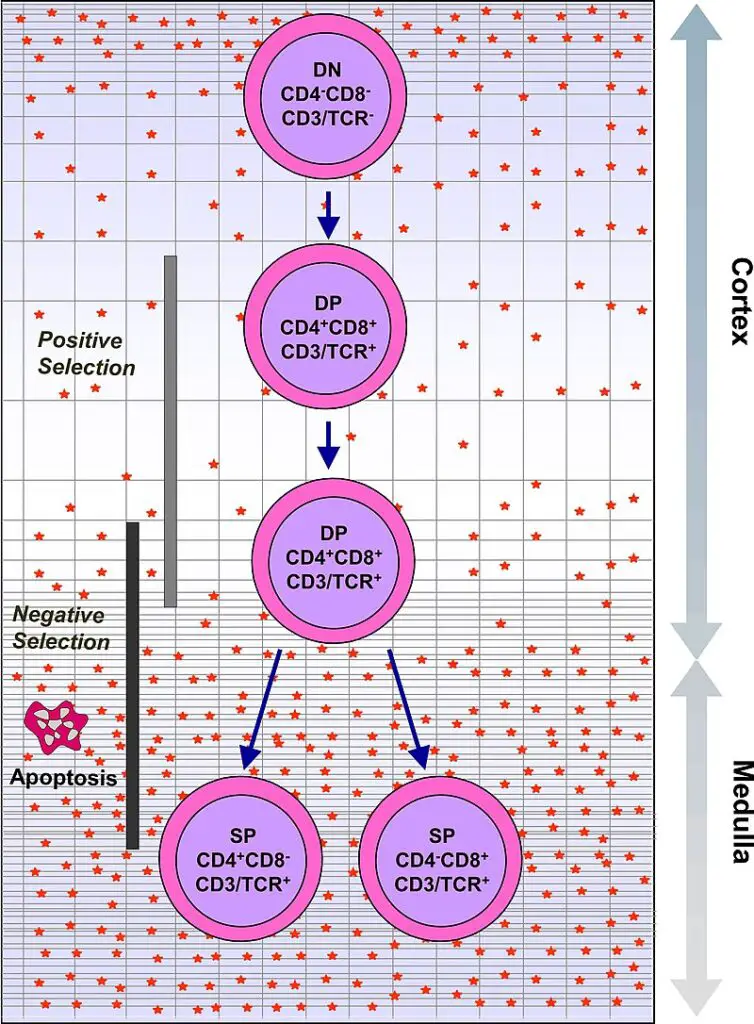
- The thymus gland plays a crucial role in the maturation of T cells, which are a vital component of the immune system responsible for cell-mediated immunity. T cells originate as hematopoietic precursors in the bone marrow and migrate to the thymus, where they are known as thymocytes. Within the thymus, a process of maturation takes place.
- During maturation, T cells undergo a selection process to ensure they can appropriately recognize antigens while avoiding reactions against self-antigens found on the body’s own tissues. This selection involves both positive and negative selection mechanisms. Positive selection ensures that T cells can bind to the major histocompatibility complex (MHC) molecules on the body’s cells. If a T cell receptor matches the specific antigen presented by the MHC, the T cell becomes activated. Negative selection, on the other hand, prevents T cells from reacting against self-antigens, thus avoiding autoimmune responses.
- The positive selection process occurs in the cortex of the thymus, where T cells that can properly bind to MHC molecules are selected. The negative selection process takes place in the medulla of the thymus, where T cells that would react against self-antigens are eliminated. After undergoing these selection processes, the mature T cells that have successfully passed leave the thymus, guided by a molecule called sphingosine-1-phosphate.
- While in the thymus, the maturation of T cells is influenced by various hormones and cytokines secreted by cells within the gland. These include thymulin, thymopoietin, and thymosins, which contribute to the development and functionality of T cells. Once T cells have left the thymus, further maturation occurs in the peripheral circulation.
- In summary, the thymus gland plays a vital role in T cell maturation by ensuring the proper selection and development of T cells capable of recognizing foreign antigens while avoiding self-reactivity. The thymus creates an environment for T cell maturation through a complex interplay of positive and negative selection processes, guided by various hormones and cytokines. The mature T cells that emerge from the thymus contribute to the effective functioning of the immune system in providing protection against pathogens and foreign substances.
Positive selection by Thymus Gland
Positive selection is a crucial process that occurs in the thymus gland, ensuring the development of functional T cells with the ability to recognize and interact appropriately with antigens presented by major histocompatibility complex (MHC) molecules. Here are the key points about positive selection:
- T cells undergo V(D)J recombination gene rearrangement stimulated by RAG1 and RAG2 genes, resulting in the formation of distinct T cell receptors. This process introduces diversity in the T cell receptor repertoire.
- The V(D)J recombination process is error-prone, leading to the production of thymocytes with non-functional T cell receptors or receptors that may react against self-antigens (autoreactive).
- Thymocytes that successfully generate a functional T cell receptor begin to express both CD4 and CD8 cell surface proteins simultaneously.
- The fate of the thymocytes depends on their interaction with the surrounding thymic epithelial cells. The T cell receptor on thymocytes interacts with the MHC molecules displayed on the surface of epithelial cells.
- Thymocytes with T cell receptors that do not react or react weakly with the MHC molecules will undergo apoptosis and be eliminated from further development.
- Thymocytes with T cell receptors that strongly interact with MHC molecules will survive and undergo proliferation.
- The outcome of positive selection determines the nature of the mature T cell. A mature T cell expresses either CD4 or CD8, but not both, depending on the strength of binding between the T cell receptor and MHC class I or class II molecules.
- T cell receptors that primarily bind to MHC class I molecules tend to develop into mature “cytotoxic” CD8-positive T cells, which are involved in cell-mediated immune responses.
- T cell receptors that predominantly bind to MHC class II molecules tend to develop into CD4-positive T cells, which play a role in activating other immune cells and coordinating immune responses.
In summary, positive selection in the thymus ensures the survival and maturation of T cells with functional T cell receptors that can interact appropriately with MHC molecules. This process eliminates autoreactive T cells and contributes to the development of a diverse T cell repertoire capable of recognizing a wide range of foreign antigens.
Negative selection by Thymus Gland
Negative selection is an important process that occurs in the thymus gland to eliminate T cells that could potentially attack the body’s own proteins, thus preventing autoimmune responses. Here are the key points about negative selection:
- Negative selection takes place in the medulla of the thymus, where epithelial cells and dendritic cells express a wide range of proteins from various tissues of the body.
- The negative selection process is stimulated by a gene called Autoimmune Regulator (AIRE), which plays a role in the expression of self-antigens in the thymus.
- Thymocytes, or developing T cells, undergo interaction with these self-antigens presented by thymic epithelial cells and dendritic cells.
- Thymocytes that strongly react to self-antigens, indicating a potential to recognize and attack the body’s own proteins, do not survive. They undergo apoptosis, a programmed cell death process.
- This process of eliminating autoreactive thymocytes helps to prevent the development of autoimmune diseases by removing T cells that could cause harm to the body’s own tissues.
- However, some CD4-positive T cells that are exposed to self-antigens can persist as a specialized subset of T cells called T regulatory cells (Tregs).
- T regulatory cells play a crucial role in maintaining immune tolerance by suppressing the activation of autoreactive T cells and preventing excessive immune responses against self-antigens.
- Tregs contribute to immune homeostasis and help prevent autoimmune diseases by regulating the immune system and promoting self-tolerance.
In summary, negative selection in the thymus eliminates T cells that have a strong reactivity to self-antigens, preventing the development of autoimmune responses. This process is crucial for shaping a functional and self-tolerant immune system, ensuring that T cells are capable of recognizing foreign antigens while avoiding harmful responses against the body’s own proteins.
Disorders of Thymus Gland
1. Thymic cysts
- Thymic cysts are abnormal fluid-filled sacs or pockets that can develop within the thymus gland. They are usually present from birth (congenital) and may interfere with the normal proliferation and functioning of thymocytes, which are the developing T cells in the thymus.
- Thymic cysts are generally benign and non-cancerous. They are typically detected incidentally during imaging studies or medical examinations, as they often do not cause any noticeable symptoms. However, in some cases, when thymic cysts become large or cause compression of surrounding structures, they can lead to symptoms and complications.
- One of the main concerns with thymic cysts is their potential impact on the immune system. The thymus gland plays a crucial role in the development and maturation of T cells, which are essential for immune function. Thymic cysts may disrupt this process, affecting the production and proliferation of thymocytes. As a result, individuals with thymic cysts may have compromised immune systems, making them more susceptible to infections.
- Common symptoms associated with thymic cysts include coughing, respiratory problems, and recurrent upper respiratory tract infections. These symptoms arise due to the compression of nearby structures, such as the trachea or bronchi, leading to airway obstruction or irritation.
- Treatment for thymic cysts typically involves surgical removal (excision) of the cyst. As the cysts are benign, removal usually resolves the symptoms and prevents further complications. However, close monitoring and follow-up care may be necessary to ensure the cysts do not recur.
- In summary, thymic cysts are congenital fluid-filled sacs that can occur within the thymus gland. While they are generally benign, they can hinder the normal proliferation of thymocytes and compromise immune function. Symptoms such as coughing and respiratory infections may arise, indicating the need for medical intervention. Surgical removal is often recommended to alleviate symptoms and prevent complications associated with thymic cysts.
2. Involution
- Involution refers to the natural process of shrinking or decreasing in size and activity of the thymus gland. While involution is a normal part of aging, certain factors can accelerate or affect the involution process.
- One of the factors that can contribute to thymic involution is stress. In infants and young children who experience neglect, malnourishment, or abuse, the thymus gland may undergo involution at a faster rate. Stress and adverse experiences can impact the functioning of the immune system, including the development and activity of T cells produced by the thymus.
- Furthermore, medical treatments such as chemotherapy, radiation therapy, and steroid therapy can also lead to thymic involution. These treatments, often used in cancer management or autoimmune disorders, can have immunosuppressive effects and affect the functioning of the thymus gland.
- It is worth noting that thymic involution is less common in newborns and young children compared to older individuals. The thymus is most active in fetal and neonatal life, contributing to the development of the immune system. However, as children grow and reach puberty, the thymus gradually decreases in size and activity.
- In some cases, premature thymic involution in young children or infants can be an indication of societal issues such as abuse or neglect. Severe stress or adverse circumstances can disrupt the normal functioning of the thymus, leading to accelerated involution.
- In summary, involution refers to the natural process of shrinking and decreasing activity in the thymus gland. Factors such as stress, medical treatments, and adverse experiences can influence the rate of thymic involution. While thymic involution is a normal part of aging, premature involution in infants and young children may be a sign of underlying societal issues.
3. Hypoplasia
- Hypoplasia refers to a condition characterized by a decrease in the number of cells in an organ, resulting in underdevelopment or incomplete development of that organ. In the case of the thymus gland, hypoplasia typically occurs in newborns and is associated with abnormal development of the third and fourth pharyngeal pouches.
- The proper development of the thymus gland involves the interaction between neural crest cells and the pharyngeal pouches. However, when substances like alcohol or organic acids are present, they can potentially affect the neural crest cells, leading to interference with the normal differentiation of the pharyngeal pouches. This abnormal development of the third and fourth pharyngeal pouches can result in hypoplasia of the thymus gland.
- The clinical manifestations of hypoplasia can vary depending on the degree of underdevelopment and the extent of genetic abnormalities. The severity of hypoplasia and the presence of defective genetic material will determine how the illness presents clinically. The symptoms and complications of thymic hypoplasia can range from mild immune dysfunction to more severe immunodeficiency disorders, depending on the extent of the organ’s underdevelopment.
- It is important to note that hypoplasia of the thymus gland is a complex condition influenced by various genetic and environmental factors. Ongoing research aims to further understand the underlying mechanisms and identify potential preventive measures or treatment options for individuals affected by thymic hypoplasia.
- In summary, hypoplasia refers to the decrease in cell number and underdevelopment of an organ. In the case of the thymus gland, hypoplasia can occur in newborns due to abnormal development of the third and fourth pharyngeal pouches. Factors such as exposure to substances like alcohol or organic acids may contribute to this abnormal development. The clinical presentation of hypoplasia depends on the degree of underdevelopment and the presence of genetic abnormalities, which will determine the specific symptoms and manifestations experienced by affected individuals.
4. Hypogammaglobulinemia
- Hypogammaglobulinemia is a condition characterized by low serum levels of immunoglobulins, also known as antibodies. Immunoglobulins play a vital role in the humoral immune response, as they are responsible for recognizing antigens and initiating a biological response to eliminate infectious agents. Hypogammaglobulinemia is the most common primary immunodeficiency disorder, affecting a significant number of patients with compromised immune systems.
- Early detection and prompt treatment of hypogammaglobulinemia are crucial in order to minimize the significant morbidity and mortality associated with this disorder. The evaluation of hypogammaglobulinemia typically involves a combination of laboratory studies, clinical observations, assessment of vaccine response, and genetic testing. These diagnostic approaches help identify the underlying cause and severity of the condition.
- The treatment of hypogammaglobulinemia often involves intravenous immunoglobulin (IVIG) transfusions, which provide the patient with a supplemental source of immunoglobulins to compensate for the deficiency. Antibiotics may also be prescribed to prevent or treat infections, which are more common in individuals with compromised immune systems. In some cases, glucocorticoids may be used to modulate the immune response.
- Managing and treating patients with hypogammaglobulinemia requires a comprehensive approach involving a practitioner or an interprofessional team. This team may include immunologists, infectious disease specialists, nurses, and other healthcare professionals. The goal is to appropriately examine, evaluate, and provide individualized care to patients with hypogammaglobulinemia, considering factors such as the underlying cause, the severity of the immunodeficiency, and the patient’s specific needs.
- In summary, hypogammaglobulinemia is characterized by low levels of immunoglobulins, leading to a compromised humoral immune response. Early detection, thorough evaluation, and timely treatment are essential to minimize the associated morbidity and mortality. The use of IVIG transfusions, antibiotics, and glucocorticoids are among the treatment options available. A collaborative and interprofessional approach is crucial in effectively managing and treating patients with hypogammaglobulinemia.
5. Pure red cell aplasia
- Pure red cell aplasia (PRCA) is a condition characterized by a severe reduction or absence of erythroid precursors in the bone marrow, leading to severe normocytic normochromic anemia and reticulocytopenia. PRCA can occur as a congenital type, such as Diamond-Blackfan anemia, or it can be acquired either as a primary disorder or secondary to another underlying condition or agent.
- In primary acquired PRCA, which is typically antibody-mediated, the immune system mistakenly targets and destroys erythroid precursors in the bone marrow. This autoimmune condition can be the sole disorder or may be associated with other autoimmune or collagen vascular diseases like systemic lupus erythematosus. Additionally, primary acquired PRCA shares morphologic features with myelodysplastic syndromes.
- Secondary acquired PRCA can be linked to various factors, including autoimmune or collagen vascular diseases, chronic lymphocytic leukemia, large granular lymphocyte leukemia, infections such as B19 parvovirus, thymoma, solid tumors, certain medications, or exposure to toxic substances.
- The treatment of PRCA often involves immunosuppression to suppress the immune response. Immunosuppressive therapy, commonly used in conjunction with corticosteroids, aims to prevent the immune system from attacking erythroid precursors. Cyclosporine A is considered one of the most effective immunosuppressive medications used in the treatment of PRCA, although specific therapeutic approaches may vary depending on the underlying subtype of the disease.
- In summary, pure red cell aplasia is a condition characterized by a severe reduction or absence of erythroid precursors in the bone marrow, leading to severe normocytic normochromic anemia. It can be congenital or acquired, with primary acquired PRCA typically being antibody-mediated and secondary acquired PRCA associated with various underlying conditions or agents. Immunosuppression, particularly with medications like cyclosporine A, is commonly used in the treatment of PRCA to suppress the immune response and restore red blood cell production.
6. Myasthenia gravis
- Myasthenia gravis (MG) is a condition characterized by the presence of antibodies that interfere with the communication between neurons and muscles, leading to weakness in the skeletal muscles. The impact of MG is primarily seen in the voluntary muscles of the body, particularly those involved in controlling the eyes, mouth, throat, and limbs.
- While myasthenia gravis can affect individuals of any age, it is more commonly observed in young women between the ages of 20 and 30, as well as older men. The exact cause of myasthenia gravis is unknown, and there is currently no known cure for the condition. However, with early diagnosis and prompt medical intervention, individuals with MG can manage their symptoms and lead longer and more active lives.
- During a myasthenia gravis crisis, individuals may experience difficulties with breathing or swallowing, which can be potentially life-threatening. These crises require immediate medical attention to ensure proper management and support.
- Treatment for myasthenia gravis focuses on symptom management and improving muscle strength. This may involve the use of medications such as acetylcholinesterase inhibitors, which help enhance communication between neurons and muscles. Immunosuppressive drugs may also be prescribed to suppress the production of the antibodies responsible for interfering with muscle function. In some cases, surgical intervention or other therapies, such as plasma exchange or intravenous immunoglobulin therapy, may be considered.
- Although myasthenia gravis poses challenges and has no definitive cure, proper medical care and treatment can significantly improve the quality of life for individuals with this condition. It is essential for individuals experiencing symptoms suggestive of myasthenia gravis to seek medical attention promptly to receive an accurate diagnosis and appropriate management.
7. Thymus Cancer
- Thymus cancer, also known as thymic cancer, is a rare form of cancer that affects the thymus gland, an organ located under the breastbone in the chest. The thymus gland plays a crucial role in the lymphatic system, which is a part of the body’s immune system. It produces lymphocytes, a type of white blood cell that helps in fighting off infections.
- There are two main types of thymus cancer: thymoma and thymic carcinoma. Both types are considered rare. Thymoma occurs when cancerous cells develop on the outer surface of the thymus gland. Thymic carcinoma, on the other hand, is a more aggressive form of thymus cancer and can be more challenging to treat. Type C thymoma is a specific subtype of thymic cancer.
- Patients with thymoma may also have associated autoimmune conditions such as rheumatoid arthritis, myasthenia gravis, or acquired pure red cell aplasia. These autoimmune conditions can coexist with thymoma and may require additional management and treatment.
- Due to the rarity of thymus cancer, treatment approaches can vary depending on the individual case. Surgery is often the primary treatment for localized thymus cancer, and additional treatments such as radiation therapy, chemotherapy, or targeted therapies may be considered based on the stage and characteristics of the cancer.
- Regular follow-up and monitoring are crucial for individuals diagnosed with thymus cancer, as recurrence or the development of other autoimmune conditions may occur. An interdisciplinary approach involving oncologists, surgeons, and other healthcare professionals is typically employed to provide comprehensive care for thymus cancer patients.
- Early detection, accurate diagnosis, and appropriate treatment are essential in managing thymus cancer. Individuals with symptoms or concerns related to the thymus gland should consult a healthcare professional for proper evaluation and guidance.
Symptoms of Thymus Cancer
Thymus cancer, located in the center of the chest near the airways and certain blood vessels, can cause various symptoms due to the pressure exerted by tumors on surrounding structures. These symptoms may include:
- Shortness of breath: Tumors in the thymus can compress the airways, leading to difficulty in breathing and a sensation of breathlessness.
- Cough: Thymus cancer can cause a persistent cough, which may be accompanied by the presence of bloody sputum.
- Chest pain: The presence of tumors in the thymus can result in chest discomfort or pain.
- Trouble swallowing: Tumors pressing on the esophagus, which is located near the thymus, can lead to difficulty in swallowing or a sensation of food getting stuck.
- Loss of appetite: Thymus cancer can cause a decreased desire to eat or a loss of appetite.
- Weight loss: Unexplained weight loss may occur as a result of thymus cancer, often associated with loss of appetite.
In addition to these symptoms, thymus tumors may also affect the superior vena cava, a major blood vessel that transports blood from the head and upper body to the heart. This can lead to a condition called superior vena cava syndrome, characterized by the following symptoms:
- Swelling in the face, neck, and upper chest, sometimes with a bluish color: The pressure on the superior vena cava can result in swelling of the surrounding tissues, leading to a bluish discoloration.
- Swelling of visible veins: The visible veins in the face, neck, and upper chest may become enlarged and more prominent.
- Headaches: Thymus tumors compressing the superior vena cava can cause headaches.
- Feeling dizzy or light-headed: Insufficient blood flow due to the compression of the superior vena cava may result in feelings of dizziness or lightheadedness.
It is important to note that these symptoms can be associated with various other conditions, and the presence of these symptoms does not necessarily indicate thymus cancer. If experiencing any of these symptoms, it is recommended to consult a healthcare professional for proper evaluation and diagnosis.
Functions of Thymus Gland
The thymus gland serves several important functions in the immune system:
- T Cell Development: The primary function of the thymus gland is to stimulate the growth, activation, and differentiation of T cells, which are a type of white blood cell. Prothymocytes are stimulated to develop into thymocytes and T lymphocytes by the thymic hormones thymosin and thymopoietin. The thymus provides an environment where T cells mature and acquire their specific receptors, which are crucial for their role in cellular immunity.
- Cytokine Secretion: The thymus gland also plays a role in the secretion of cytokines, which are small signaling proteins that regulate the growth and activity of T cells at various stages. Cytokines help to coordinate and modulate the immune response, ensuring the proper development and functioning of T cells.
- Development of Fetal Immunity: The thymus starts contributing to fetal immunity as early as the 12th week of pregnancy. Throughout fetal life and into childhood, the thymus continues to function and play a vital role in the development of the immune system. It helps in the production and maturation of T cells, which are important for defending against infections and diseases.
- Endocrine Function: In addition to its immune-related functions, the thymus gland also has an endocrine role. It produces hormones, including human growth hormone, which is essential for the growth and development of the body.
The thymus gland’s functions are essential for the proper functioning of the immune system. By producing and maturing T cells, the thymus plays a crucial role in cellular immunity, immune regulation, and defense against pathogens.
Difference between Thyroid and Thymus
Thyroid and thymus are two distinct glands in the body with different characteristics and functions. Here is a comparison between the two:
Definition:
- Thyroid: The thyroid is a gland of the endocrine system responsible for producing thyroid hormones.
- Thymus: The thymus is an organ of the lymphatic system involved in the production and maturation of T cells of the immune system.
Anatomy:
- Thyroid: The thyroid consists of two lobes located in the neck region. It is composed of follicles surrounded by epithelial cells.
- Thymus: The thymus has an outer capsule and an inner medulla section. It consists of two lobules.
Changes in Size with Age:
- Thyroid: The size of the thyroid gland does not change significantly as you age.
- Thymus: The thymus tends to become smaller as you age. This process is known as thymic involution.
What It Produces:
- Thyroid: The thyroid gland produces two important hormones called thyroxine (T4) and triiodothyronine (T3), which regulate the metabolic rate and activity in the body.
- Thymus: The thymus produces and matures T cells, which are crucial for the cell-mediated immune response.
Functions:
- Thyroid: The thyroid gland plays a key role in controlling the metabolic rate and various physiological functions in the body, such as energy production, growth, and development.
- Thymus: The thymus is involved in the development and maturation of T cells, which are responsible for the cell-mediated immune response, including recognizing and attacking foreign substances and pathogens.
Disorders:
- Thyroid: Disorders of the thyroid gland include hypothyroidism (too few thyroid hormones) and hyperthyroidism (excess production of thyroid hormones).
- Thymus: Disorders associated with the thymus include myasthenia gravis, an autoimmune condition that affects the neuromuscular junction, and hypogammaglobulinemia, a condition characterized by low levels of immunoglobulins (antibodies).
In summary, while both the thyroid and thymus are glands in the body, they have distinct anatomical structures, functions, and associated disorders. The thyroid primarily produces thyroid hormones for metabolic control, while the thymus is involved in the production and maturation of T cells, contributing to the immune response.
| Characteristics | Thyroid | Thymus |
|---|---|---|
| Definition | A gland of the endocrine system | An organ of the lymphatic system |
| Anatomy | Two lobes comprised of follicles surrounded by epithelia | An outer capsule and inner medulla section, two lobules |
| Changes in size with age | Does not change in size as you age | Becomes smaller as you age |
| What it produces | Two thyroid hormones called thyroxine (T4) and triiodothyronine (T3) | T cells of the immune system |
| Functions | Controls metabolic rate and activity in the body | Cell-mediated immune response |
| Disorders | Too few hormones or too many hormones may be produced | The disorder, myasthenia gravis, and the condition, hypogammaglobulinemia |
FAQ
What is the thymus gland?
The thymus gland is a small organ located in the chest, near the heart. It is part of the immune system and plays a crucial role in the maturation of T cells, a type of white blood cell.
What is the function of the thymus gland?
The thymus gland is responsible for the development and maturation of T cells, which are essential for cell-mediated immunity. It helps educate T cells to recognize foreign antigens while preventing them from attacking the body’s own tissues.
When does the thymus gland reach its maximum size?
The thymus gland is relatively large during infancy and childhood. It reaches its maximum size during puberty and gradually decreases in size thereafter through a process called involution.
What is thymic involution?
Thymic involution is the natural shrinking and replacement of the thymus gland with fatty tissue that occurs as a person ages. It is a normal part of the aging process.
Can the thymus gland be affected by diseases?
Yes, the thymus gland can be affected by various diseases, including thymic tumors (thymomas), thymic carcinomas, and autoimmune disorders such as myasthenia gravis.
How is thymus cancer diagnosed?
Thymus cancer is diagnosed through a combination of imaging tests (such as CT scans), biopsy, and analysis of the tumor tissue. Medical professionals use these methods to determine the type and stage of the cancer.
Are there any symptoms associated with thymus cancer?
Symptoms of thymus cancer may include coughing, chest pain, difficulty swallowing, shortness of breath, and weight loss. However, symptoms can vary depending on the location and size of the tumor.
Can thymus cancer be treated?
Yes, treatment options for thymus cancer include surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. The choice of treatment depends on the type and stage of the cancer, as well as individual factors.
Can the removal of the thymus gland affect the immune system?
While the thymus gland is important for T cell maturation, its removal (thymectomy) is sometimes necessary in certain medical conditions, such as thymus tumors or myasthenia gravis. However, other lymphoid organs and tissues can compensate for its absence, and the immune system can still function effectively.
Can thymus gland disorders lead to immune system problems?
Yes, disorders of the thymus gland can impact the immune system. For example, thymic hypoplasia or dysfunction can lead to immune deficiencies, affecting the body’s ability to mount an adequate immune response. Additionally, autoimmune disorders such as myasthenia gravis can arise from dysfunction within the thymus gland.
Reference
- Lydyard, P.M., Whelan,A.,& Fanger,M.W. (2005).Immunology (2 ed.).London: BIOS Scientific Publishers.
- Brooks, G. F., Jawetz, E., Melnick, J. L., & Adelberg, E. A. (2010). Jawetz, Melnick, & Adelberg’s medical microbiology. New York: McGraw Hill Medical.
- Playfair, J., & Chain, B. (2001). Immunology at a Glance. London: Blackwell Publishing.
- Owen, J. A., Punt, J., & Stranford, S. A. (2013). Kuby Immunology (7 ed.). New York: W.H. Freeman and Company.
- Pearse G. Normal structure, function and histology of the thymus. Toxicol Pathol. 2006;34(5):504-14. doi: 10.1080/01926230600865549. PMID: 17067941.
- Askin DF, Young S. The thymus gland. Neonatal Netw. 2001 Dec;20(8):7-13. doi: 10.1891/0730-0832.20.8.7. PMID: 12144107.
- Thapa, Puspa, and Donna L Farber. “The Role of the Thymus in the Immune Response.” Thoracic surgery clinics vol. 29,2 (2019): 123-131. doi:10.1016/j.thorsurg.2018.12.001
- Bach JF. Thymic hormones. J Immunopharmacol. 1979;1(3):277-310. doi: 10.3109/08923977909026377. PMID: 233313.
- Zdrojewicz Z, Pachura E, Pachura P. The Thymus: A Forgotten, But Very Important Organ. Adv Clin Exp Med. 2016 Mar-Apr;25(2):369-75. doi: 10.17219/acem/58802. PMID: 27627572.
- Remien K, Jan A. Anatomy, Head and Neck, Thymus. [Updated 2021 Feb 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539748/
